J Korean Med Sci.
2022 Dec;37(47):e340. 10.3346/jkms.2022.37.e340.
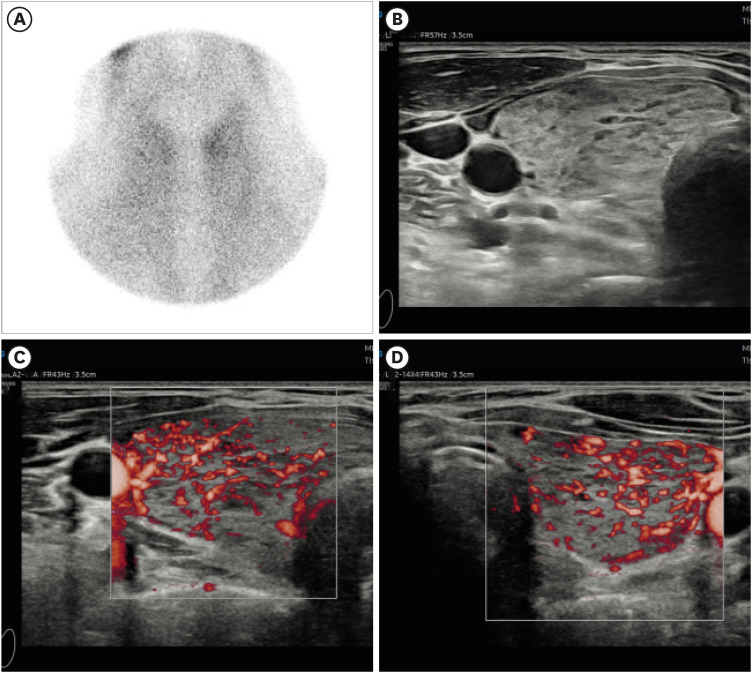
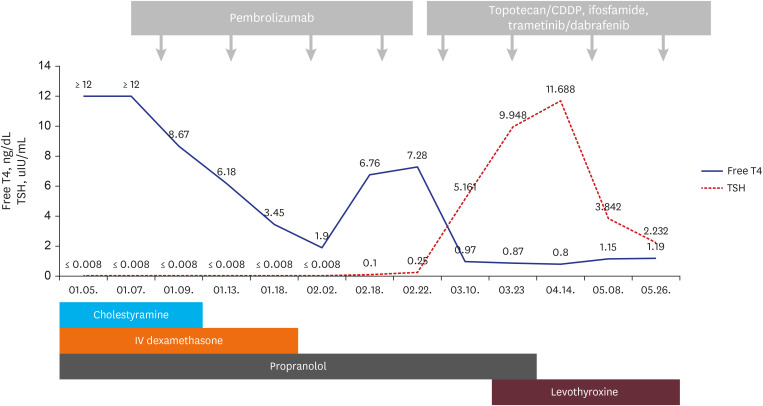
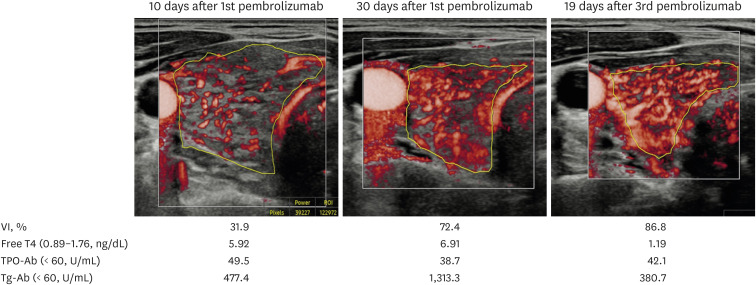
Case 5: A 41-Year-Old Woman With Palpitation
- Affiliations
-
- 1Division of Endocrinology and Metabolism, Department of Internal Medicine, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Division of Medical Oncology, Department of Internal Medicine, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 3Division of Endocrinology and Metabolism, Department of Internal Medicine, Eunpyeong St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2536517
- DOI: http://doi.org/10.3346/jkms.2022.37.e340
Figure
Reference
-
1. Baek HS, Park JY, Jeong CH, Ha J, Kang MI, Lim DJ. Usefulness of real-time quantitative microvascular ultrasonography for differentiation of Graves’ disease from destructive thyroiditis in thyrotoxic patients. Endocrinol Metab (Seoul). 2022; 37(2):323–332. PMID: 35413779.2. Badiu CM. Williams Textbook of Endocrinology. Acta Endocrinol (Bucur). 2019; 15(3):416.3. Yamauchi I, Sakane Y, Fukuda Y, Fujii T, Taura D, Hirata M, et al. Clinical features of nivolumab-induced thyroiditis: a case series study. Thyroid. 2017; 27(7):894–901. PMID: 28537531.4. Yoon JH, Hong AR, Kim HK, Kang HC. Characteristics of immune-related thyroid adverse events in patients treated with PD-1/PD-L1 inhibitors. Endocrinol Metab (Seoul). 2021; 36(2):413–423. PMID: 33820396.5. Friedman CF, Proverbs-Singh TA, Postow MA. Treatment of the immune-related adverse effects of immune checkpoint inhibitors: a review. JAMA Oncol. 2016; 2(10):1346–1353. PMID: 27367787.6. Lee H, Hodi FS, Giobbie-Hurder A, Ott PA, Buchbinder EI, Haq R, et al. Characterization of thyroid disorders in patients receiving immune checkpoint inhibition therapy. Cancer Immunol Res. 2017; 5(12):1133–1140. PMID: 29079654.7. Illouz F, Drui D, Caron P, Do Cao C. Expert opinion on thyroid complications in immunotherapy. Ann Endocrinol (Paris). 2018; 79(5):555–561. PMID: 30126627.8. Zhan L, Feng HF, Liu HQ, Guo LT, Chen C, Yao XL, et al. Immune checkpoint inhibitors-related thyroid dysfunction: epidemiology, clinical presentation, possible pathogenesis, and management. Front Endocrinol (Lausanne). 2021; 12:649863. PMID: 34177799.9. El Sabbagh R, Azar NS, Eid AA, Azar ST. Thyroid dysfunctions due to immune checkpoint inhibitors: a review. Int J Gen Med. 2020; 13:1003–1009. PMID: 33177863.10. Baek HS, Jeong C, Shin K, Lee J, Suh H, Lim DJ, et al. Association between the type of thyroid dysfunction induced by immune checkpoint inhibitors and prognosis in cancer patients. BMC Endocr Disord. 2022; 22(1):89. PMID: 35379219.11. Kreamer KM. Immune checkpoint blockade: a new paradigm in treating advanced cancer. J Adv Pract Oncol. 2014; 5(6):418–431. PMID: 26328216.12. Petitprez F, Meylan M, de Reyniès A, Sautès-Fridman C, Fridman WH. The tumor microenvironment in the response to immune checkpoint blockade therapies. Front Immunol. 2020; 11:784. PMID: 32457745.13. Kotwal A, Kottschade L, Ryder M. PD-L1 inhibitor-induced thyroiditis is associated with better overall survival in cancer patients. Thyroid. 2020; 30(2):177–184. PMID: 31813343.14. Delivanis DA, Gustafson MP, Bornschlegl S, Merten MM, Kottschade L, Withers S, et al. Pembrolizumab-induced thyroiditis: comprehensive clinical review and insights into underlying involved mechanisms. J Clin Endocrinol Metab. 2017; 102(8):2770–2780. PMID: 28609832.15. González-Rodríguez E, Rodríguez-Abreu D. Spanish Group for Cancer Immuno-Biotherapy (GETICA). Immune checkpoint inhibitors: review and management of endocrine adverse events. Oncologist. 2016; 21(7):804–816. PMID: 27306911.16. Muir CA, Clifton-Bligh RJ, Long GV, Scolyer RA, Lo SN, Carlino MS, et al. Thyroid immune-related adverse events following immune checkpoint inhibitor treatment. J Clin Endocrinol Metab. 2021; 106(9):e3704–e3713. PMID: 33878162.17. Schneider BJ, Naidoo J, Santomasso BD, Lacchetti C, Adkins S, Anadkat M, et al. Management of immune-related adverse events in patients treated with immune checkpoint inhibitor therapy: ASCO guideline update. J Clin Oncol. 2021; 39(36):4073–4126. PMID: 34724392.18. Lima Ferreira J, Costa C, Marques B, Castro S, Victor M, Oliveira J, et al. Improved survival in patients with thyroid function test abnormalities secondary to immune-checkpoint inhibitors. Cancer Immunol Immunother. 2021; 70(2):299–309. PMID: 32712715.19. de Miguel M, Calvo E. Clinical challenges of immune checkpoint inhibitors. Cancer Cell. 2020; 38(3):326–333. PMID: 32750319.20. Muir CA, Menzies AM, Clifton-Bligh R, Tsang VH. Thyroid toxicity following immune checkpoint inhibitor treatment in advanced cancer. Thyroid. 2020; 30(10):1458–1469. PMID: 32264785.21. Mazarico I, Capel I, Giménez-Palop O, Albert L, Berges I, Luchtenberg F, et al. Low frequency of positive antithyroid antibodies is observed in patients with thyroid dysfunction related to immune check point inhibitors. J Endocrinol Invest. 2019; 42(12):1443–1450. PMID: 31093955.22. Pollack R, Ashash A, Cahn A, Rottenberg Y, Stern H, Dresner-Pollak R. Immune checkpoint inhibitor-induced thyroid dysfunction is associated with higher body mass index. J Clin Endocrinol Metab. 2020; 105(10):e3620–e3627.23. Cortellini A, Bersanelli M, Buti S, Cannita K, Santini D, Perrone F, et al. A multicenter study of body mass index in cancer patients treated with anti-PD-1/PD-L1 immune checkpoint inhibitors: when overweight becomes favorable. J Immunother Cancer. 2019; 7(1):57. PMID: 30813970.24. Kichenadasse G, Miners JO, Mangoni AA, Rowland A, Hopkins AM, Sorich MJ. Association between body mass index and overall survival with immune checkpoint inhibitor therapy for advanced non-small cell lung cancer. JAMA Oncol. 2020; 6(4):512–518. PMID: 31876896.