Arch Hand Microsurg.
2022 Dec;27(4):292-295. 10.12790/ahm.22.0039.
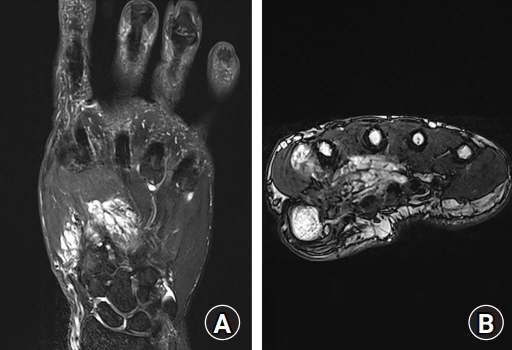
Vascular malformation in the hand causing adduction contracture of the thumb: a case report
- Affiliations
-
- 1Department of Orthopaedic Surgery, St. Vincent’s Hospital, College of Medicine, The Catholic University of Korea, Suwon, Korea
- 2Department of Internal Medicine, Kirk Kerkorian School of Medicine, Las Vegas, NV, USA
- 3Department of Orthopaedic Surgery, Bucheon St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Bucheon, Korea
- 4Department of Orthopedic Surgery, Gyeongsang National University Changwon Hospital, Gyeongsang National University College of Medicine, Changwon, Korea
- KMID: 2536214
- DOI: http://doi.org/10.12790/ahm.22.0039
Abstract
- Vascular malformations of the muscle are rare non-proliferative vascular lesions, and few case reports have described intramuscular vascular malformations in the upper extremities. Vascular malformations of the muscle may produce musculoskeletal deformities due to muscle contracture. Symptomatic intramuscular vascular malformations are commonly treated with surgery and interventional management. We report a vascular malformation that could not be completely resected. It caused adduction contracture of the thumb in the hand. Sclerotherapy was performed before surgery, but the contracture did not improve. Thus, we additionally performed adductor tenotomy. There was no evidence of recurrence during 6 months of follow-up.
Keyword
Figure
Reference
-
References
1. Wassef M, Blei F, Adams D, et al. Vascular anomalies classification: recommendations from the International Society for the Study of Vascular Anomalies. Pediatrics. 2015; 136:e203–14.
Article2. Hein KD, Mulliken JB, Kozakewich HP, Upton J, Burrows PE. Venous malformations of skeletal muscle. Plast Reconstr Surg. 2002; 110:1625–35.
Article3. Flors L, Leiva-Salinas C, Maged IM, et al. MR imaging of soft-tissue vascular malformations: diagnosis, classification, and therapy follow-up. Radiographics. 2011; 31:1321–41.
Article4. Wieck MM, Nowicki D, Schall KA, Zeinati C, Howell LK, Anselmo DM. Management of pediatric intramuscular venous malformations. J Pediatr Surg. 2017; 52:598–601.
Article5. Liu Y, Li R, Liu Z, Wang S, Lu L. Intramuscular hemangioma within the biceps brachii causing the limitations of elbow extension and forearm pronation: a case report. Medicine (Baltimore). 2019; 98:e14343.6. Chen RJ, Vrazas JI, Penington AJ. Surgical management of intramuscular venous malformations. J Pediatr Orthop. 2021; 41:e67–73.
Article7. Domb BG, Khanna AJ, Mitchell SE, Frassica FJ. Toe-walking attributable to venous malformation of the calf muscle. Clin Orthop Relat Res. 2004; (420):225–9.
Article8. Bella GP, Manivel JC, Thompson RC Jr, Clohisy DR, Cheng EY. Intramuscular hemangioma: recurrence risk related to surgical margins. Clin Orthop Relat Res. 2007; 459:186–91.9. James CA, Braswell LE, Wright LB, et al. Preoperative sclerotherapy of facial venous malformations: impact on surgical parameters and long-term follow-up. J Vasc Interv Radiol. 2011; 22:953–60.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical experiences in Thumb reconstruction
- Vascular Malformation of Flexor Hallucis Longus Muscle Associated with a Flexion Deformities of Toes: A Case Report
- Functional reconstruction of the thumb by heterotopic thumb-to-thumb replantation and secondary opponensplasty in bilateral amputation in the upper extremities: a case report
- Cortical Infarction with Weakness of Individual Intrinsic Hand Muscles
- Clinical Experience of Thumb-in-palm Deformity