J Korean Med Sci.
2022 Nov;37(45):e330. 10.3346/jkms.2022.37.e330.
Age at Menopause and Suicidal Ideation in Menopausal Women: A Study of Korea National Health and Nutrition Examination Survey Data
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Korea University College of Medicine, Seoul, Korea
- 2Department of Biostatistics, Korea University College of Medicine, Seoul, Korea
- 3Department of Obstetrics and Gynecology, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2536131
- DOI: http://doi.org/10.3346/jkms.2022.37.e330
Abstract
- Background
Although menopause is considered a risk factor for depression, no association has been established between the risk of suicidal ideation and age at menopause. This study aimed to evaluate the association between age at menopause and suicidal ideation in middleaged menopausal Korean women.
Methods
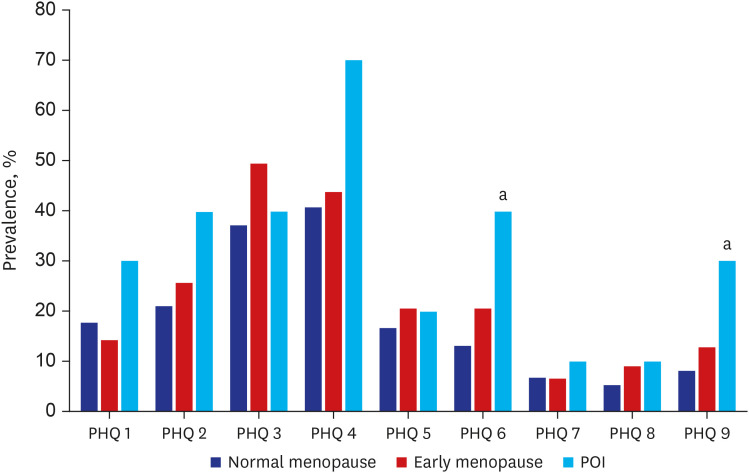
This cross-sectional study used data from the Korea National Health and Nutrition Examination Survey (2013–2018). Women aged 40–65 years were divided into the following three categories: primary ovarian insufficiency (POI), early menopause, and menopause, according to age at natural menopause (< 40, 40–45, and > 45 years, respectively). Depressive symptoms were assessed using the Patient Health Questionnaire-9 (PHQ-9).
Results
Among 2,232 menopausal women, 25 (1.1%) experienced POI and 114 (5.1%) experienced early menopause. The PHQ-9 items that pertained to low self-esteem and suicidal ideation scored higher in women with POI than in those who experienced menopause after 45 years of age. The prevalence of suicidal ideation differed significantly according to age at menopause (POI, 30.0%; early menopause, 12.7%; menopause, 8.0%; P = 0.016). Logistic regression analysis revealed that POI was significantly associated with suicidal ideation after the adjustment for age, body mass index, and education, household income, and walking levels (odds ratio, 4.2; 95% confidence interval, 1.0–17.7).
Conclusion
Korean middle-aged women with POI were more likely to have suicidal ideation than those who experienced menopause at 45 years or above, despite not being diagnosed with major depressive disorder.
Figure
Reference
-
1. Xu X, Jones M, Mishra GD. Age at natural menopause and development of chronic conditions and multimorbidity: results from an Australian prospective cohort. Hum Reprod. 2020; 35(1):203–211. PMID: 31955198.2. Santoro N. Mechanisms of premature ovarian failure. Ann Endocrinol (Paris). 2003; 64(2):87–92. PMID: 12773939.3. Kokcu A. Premature ovarian failure from current perspective. Gynecol Endocrinol. 2010; 26(8):555–562. PMID: 20500113.4. Lim YM, Jeong K, Lee SR, Chung HW, Lee W. Association between premature ovarian insufficiency, early menopause, socioeconomic status in a nationally representative sample from Korea. Maturitas. 2019; 121:22–27. PMID: 30704561.5. Choe SA, Sung J. Trends of premature and early menopause: a comparative study of the US National Health and Nutrition Examination Survey and the Korea National Health and Nutrition Examination Survey. J Korean Med Sci. 2020; 35(14):e97. PMID: 32281314.6. Uygur D, Sengül O, Bayar D, Erdinç S, Batioğlu S, Mollamahmutoglu L. Bone loss in young women with premature ovarian failure. Arch Gynecol Obstet. 2005; 273(1):17–19. PMID: 16007508.7. Roeters van Lennep JE, Heida KY, Bots ML, Hoek A. collaborators of the Dutch Multidisciplinary Guideline Development Group on Cardiovascular Risk Management after Reproductive Disorders. Cardiovascular disease risk in women with premature ovarian insufficiency: a systematic review and meta-analysis. Eur J Prev Cardiol. 2016; 23(2):178–186. PMID: 25331207.8. Deeks AA, Gibson-Helm M, Teede H, Vincent A. Premature menopause: a comprehensive understanding of psychosocial aspects. Climacteric. 2011; 14(5):565–572. PMID: 21854296.9. Georgakis MK, Thomopoulos TP, Diamantaras AA, Kalogirou EI, Skalkidou A, Daskalopoulou SS, et al. Association of age at menopause and duration of reproductive period with depression after menopause: a systematic review and meta-analysis. JAMA Psychiatry. 2016; 73(2):139–149. PMID: 26747373.10. Bromet E, Andrade LH, Hwang I, Sampson NA, Alonso J, de Girolamo G, et al. Cross-national epidemiology of DSM-IV major depressive episode. BMC Med. 2011; 9(1):90. PMID: 21791035.11. Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012; 380(9859):2163–2196. PMID: 23245607.12. Cuadros JL, Fernández-Alonso AM, Cuadros-Celorrio AM, Fernández-Luzón N, Guadix-Peinado MJ, del Cid-Martín N, et al. Perceived stress, insomnia and related factors in women around the menopause. Maturitas. 2012; 72(4):367–372. PMID: 22721806.13. Pérez-López FR, Chedraui P, Gilbert JJ, Pérez-Roncero G. Cardiovascular risk in menopausal women and prevalent related co-morbid conditions: facing the post-Women’s Health Initiative era. Fertil Steril. 2009; 92(4):1171–1186. PMID: 19700149.14. Nock MK, Hwang I, Sampson NA, Kessler RC. Mental disorders, comorbidity and suicidal behavior: results from the National Comorbidity Survey Replication. Mol Psychiatry. 2010; 15(8):868–876. PMID: 19337207.15. Kweon S, Kim Y, Jang MJ, Kim Y, Kim K, Choi S, et al. Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES). Int J Epidemiol. 2014; 43(1):69–77. PMID: 24585853.16. Han C, Jo SA, Kwak JH, Pae CU, Steffens D, Jo I, et al. Validation of the Patient Health Questionnaire-9 Korean version in the elderly population: the Ansan Geriatric study. Compr Psychiatry. 2008; 49(2):218–223. PMID: 18243897.17. Gilbody S, Richards D, Brealey S, Hewitt C. Screening for depression in medical settings with the Patient Health Questionnaire (PHQ): a diagnostic meta-analysis. J Gen Intern Med. 2007; 22(11):1596–1602. PMID: 17874169.18. Cannon DS, Tiffany ST, Coon H, Scholand MB, McMahon WM, Leppert MF. The PHQ-9 as a brief assessment of lifetime major depression. Psychol Assess. 2007; 19(2):247–251. PMID: 17563207.19. Koo KM, Kim K. Effects of physical activity on the stress and suicidal ideation in Korean adult women with depressive disorder. Int J Environ Res Public Health. 2020; 17(10):3502. PMID: 32429561.20. Kim J, Kim JH. A facilitator of leisure activities for stress-related growth experience among middle-aged Korean women with depression. Health Care Women Int. 2014; 35(11-12):1245–1266. PMID: 25372946.21. Rocca WA, Grossardt BR, Geda YE, Gostout BS, Bower JH, Maraganore DM, et al. Long-term risk of depressive and anxiety symptoms after early bilateral oophorectomy. Menopause. 2008; 15(6):1050–1059. PMID: 18724263.22. Saunders KE, Hawton K. Suicidal behaviour and the menstrual cycle. Psychol Med. 2006; 36(7):901–912. PMID: 16573848.23. Arevalo MA, Azcoitia I, Garcia-Segura LM. The neuroprotective actions of oestradiol and oestrogen receptors. Nat Rev Neurosci. 2015; 16(1):17–29. PMID: 25423896.24. Baca-Garcia E, Vaquero C, Diaz-Sastre C, Ceverino A, Saiz-Ruiz J, Fernández-Piquera J, et al. A pilot study on a gene-hormone interaction in female suicide attempts. Eur Arch Psychiatry Clin Neurosci. 2003; 253(6):281–285. PMID: 14714116.25. Wie JH, Nam SK, Ko HS, Shin JC, Park IY, Lee Y. The association between abortion experience and postmenopausal suicidal ideation and mental health: results from the 5th Korean National Health and Nutrition Examination Survey (KNHANES V). Taiwan J Obstet Gynecol. 2019; 58(1):153–158. PMID: 30638471.26. Chang JC, Yen AM, Lee CS, Chen SL, Chiu SY, Fann JC, et al. Metabolic syndrome and the risk of suicide: a community-based integrated screening samples cohort study. Psychosom Med. 2013; 75(9):807–814. PMID: 24163389.27. Simon GE, Rutter CM, Peterson D, Oliver M, Whiteside U, Operskalski B, et al. Does response on the PHQ-9 depression questionnaire predict subsequent suicide attempt or suicide death? Psychiatr Serv. 2013; 64(12):1195–1202. PMID: 24036589.28. Park SC, Sakong J, Koo BH, Kim JM, Jun TY, Lee MS, et al. Clinical significance of the number of depressive symptoms in major depressive disorder: results from the CRESCEND study. J Korean Med Sci. 2016; 31(4):617–622. PMID: 27051248.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Metabolic Syndrome and Suicidal Ideation in Korean Based on the 2010 Korean National Health and Nutrition Examination Survey
- The Risk Factors of Suicidal Ideation by Age Groups among the Elderly in Korea
- The Risk Factors of Suicidal Ideation according to Age Groups among the Adolescents in Korea
- Association of Breastfeeding Duration with Menopausal Age and Menstrual Period: Analysis based on the Korea National Health and Nutrition Examination Survey 2016–2018
- Combined Influence of Smoking and Alcohol Drinking on Suicidal Ideation and Attempts among Korean Adults: Using Data from the Korean National Health and Nutrition Examination Survey 2008~2011