Obstet Gynecol Sci.
2022 Nov;65(6):552-559. 10.5468/ogs.22133.
The effect of diluted ropivacaine in distending fluid on cramping pain after hysteroscopic surgeries: a randomized clinical trial study
- Affiliations
-
- 1Endometriosis Research Center, Iran University of Medical Sciences, Tehran, Iran
- 2Department of Obstetrics and Gynecology, School of Medicine, Iran University of Medical Sciences, Tehran, Iran
- 3Medical Biotechnology, Iran University of Medical Sciences, Tehran, Iran
- 4Department of Anesthesiology, Iran University of Medical Sciences, Tehran, Iran
- 5Department of Obstetrics and Gynecology, School of Medicine, Fatemieh Hospital, Hamadan, Iran
- 6Clinical Research Development Unit of Fatemieh Hospital, Hamadan University of Medical Sciences, Hamadan, Iran
- KMID: 2535963
- DOI: http://doi.org/10.5468/ogs.22133
Abstract
Objective
The effect of ropivacaine on postoperative hysteroscopy has not yet been evaluated; this study investigated the effect of diluted ropivacaine in distending media during hysteroscopy on postoperative cramping pain.
Methods
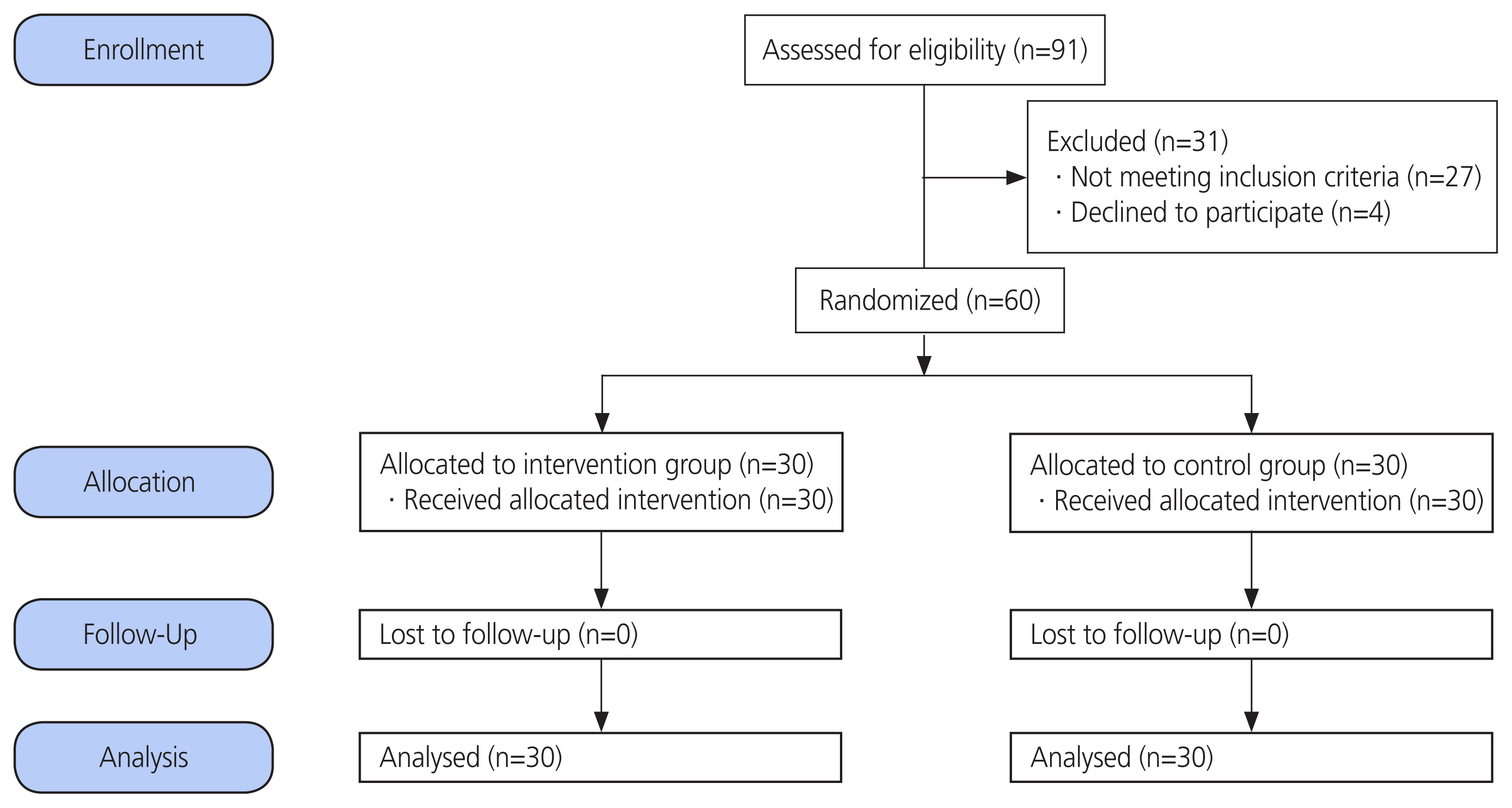
This double-blind randomized clinical trial was conducted on 60 women who underwent hysteroscopy at a tertiary hospital. Normal saline was used as the distending fluid in both groups. The intervention group received 10 mL of 2% ropivacaine in only one bottle of 1,000 mL normal saline as a distending fluid, while the control group received 10 mL of normal saline in 1,000 mL normal saline during hysteroscopy. Patients’ pain scores were evaluated before hysteroscopy and at 2, 6, 12, 24, and 48 hours after hysteroscopy.
Results
Based on the results, the pain measured by visual analog scale (VAS) score was significant at 6 and 12 hours after the intervention was significantly lower than that in the ropivacaine group (3.03±1.57 vs. 4±1.49, P=0.02 at 6 hours and 1.28±1.36 vs. 2.4±1.43, P=0.003 at 12 hours). There were no significant differences in the VAS scores at 2, 24, and 48 hours after the intervention between the two groups.
Conclusion
Ropivacaine in the distending fluid during hysteroscopy is associated with a significant reduction in pain within a few hours after hysteroscopy with no remarkable adverse effects.
Keyword
Figure
Reference
-
References
1. Gkrozou F, Dimakopoulos G, Vrekoussis T, Lavasidis L, Koutlas A, Navrozoglou I, et al. Hysteroscopy in women with abnormal uterine bleeding: a meta-analysis on four major endometrial pathologies. Arch Gynecol Obstet. 2015; 291:1347–54.2. van Dongen H, de Kroon CD, Jacobi CE, Trimbos JB, Jansen FW. Diagnostic hysteroscopy in abnormal uterine bleeding: a systematic review and meta-analysis. BJOG. 2007; 114:664–75.
Article3. Salazar CA, Isaacson KB. Office operative hysteroscopy: an update. J Minim Invasive Gynecol. 2018; 25:199–208.
Article4. Ma T, Readman E, Hicks L, Porter J, Cameron M, Ellett L, et al. Is outpatient hysteroscopy the new gold standard? Results from an 11 year prospective observational study. Aust N Z J Obstet Gynaecol. 2017; 57:74–80.
Article5. Zupi E, Luciano AA, Valli E, Marconi D, Maneschi F, Romanini C. The use of topical anesthesia in diagnostic hysteroscopy and endometrial biopsy. Fertil Steril. 1995; 63:414–6.
Article6. de Carvalho Schettini JA, Ramos de Amorim MM, Ribeiro Costa AA, Albuquerque Neto LC. Pain evaluation in outpatients undergoing diagnostic anesthesia-free hysteroscopy in a teaching hospital: a cohort study. J Minim Invasive Gynecol. 2007; 14:729–35.
Article7. Evangelista A, Oliveira MA, Crispi CP, Lamblet MF, Raymundo TS, Santos LC. Diagnostic hysteroscopy using liquid distention medium: comparison of pain with warmed saline solution vs room-temperature saline solution. J Minim Invasive Gynecol. 2011; 18:104–7.
Article8. Mak N, Reinders IMA, Slockers SA, Westen EHMN, Maas JWM, Bongers MY. The effect of music in gynaecological office procedures on pain, anxiety and satisfaction: a randomized controlled trial. Gynecol Sur. 2017; 14:14.
Article9. Bernatzky G, Strickner S, Presch M, Wendtner F, Kullich W. Music as non-pharmacological pain management in clinics. MacDonald R, Kreutz G, Mitchell L, editors. Music, health, and wellbeing. New York (NY): Oxford Univereity Press Inc;2012. p. 257–75.10. Singh M, Khan RM, Bano S, Huda W, Hakim S, Grover N. Non-pharmacological relief of acute pain following total abdominal hysterectomy. Can J Anaesth. 2002; 49:530–1.
Article11. Sohl SJ, Avis NE, Stanbery K, Tooze JA, Moormann K, Danhauer SC. Feasibility of a brief yoga intervention for improving acute pain and distress post gynecologic surgery. Int J Yoga Therap. 2016; 26:43–7.
Article12. Ahmad G, Attarbashi S, O’Flynn H, Watson AJ. Pain relief in office gynaecology: a systematic review and meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2011; 155:3–13.
Article13. Cooper NA, Khan KS, Clark TJ. Local anaesthesia for pain control during outpatient hysteroscopy: systematic review and meta-analysis. BMJ. 2010; 340:c1130.
Article14. De Silva PM, Carnegy A, Smith PP, Clark TJ. Local anaesthesia for office hysteroscopy: a systematic review & meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2020; 252:70–81.
Article15. Miranda DB, Bastos MM, Govêia CS, Silva RE, Rodrigues FW. Efficacy of ropivacaine versus bupivacaine in preventing peribulbar block failure: a meta-analysis. Efficacy of ropivacaine versus bupivacaine in preventing peribulbar block failure: a meta-analysis. Miranda DB, Bastos MM, Govêia CS, Silva RE, Rodrigues FW, editors. Eur J Ophthalmol. 2021. 31:p. 2731–7.16. Barel O, Preuss E, Stolovitch N, Weinberg S, Barzilay E, Pansky M. Addition of lidocaine to the distension medium in hysteroscopy decreases pain during the procedure- a randomized double-blind, placebo-controlled trial. J Minim Invasive Gynecol. 2021; 28:865–71.17. Kabli N, Tulandi T. A randomized trial of outpatient hysteroscopy with and without intrauterine anesthesia. J Minim Invasive Gynecol. 2008; 15:308–10.
Article18. Foster RH, Markham A. Levobupivacaine: a review of its pharmacology and use as a local anaesthetic. Drugs. 2000; 59:551–79.19. Kucuk C, Kadiogullari N, Canoler O, Savli S. A placebocontrolled comparison of bupivacaine and ropivacaine instillation for preventing postoperative pain after laparoscopic cholecystectomy. Surg Today. 2007; 37:396–400.
Article20. Mahomed K, McLean J, Ahmed M, Zolotarev B, Shaddock N. I Intrauterine anaesthetic after hysteroscopy to reduce post-operative pain - a double blind randomised controlled trial. Aust N Z J Obstet Gynaecol. 2016; 56:484–8.
Article21. Frawley N, Jones R, Pearce D, Vollenhoven B. The effect of intraperitoneal ropivacaine on post-operative pain and recovery after diagnostic laparoscopy and hysteroscopy: a randomised double-blind placebo-controlled trial. Aust N Z J Obstet Gynaecol. 2022; 62:118–24.
Article22. Yong L, Guang B. Intraperitoneal ropivacaine instillation versus no intraperitoneal ropivacaine instillation for laparoscopic cholecystectomy: a systematic review and meta-analysis. Int J Surg. 2017; 44:229–43.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Complications of fluid overload during hysteroscopic surgery: cardiomyopathy and epistaxis - A case report -
- Comparison of clinical efficacy of ropivacaine and lignocaine with adrenaline for implant surgery anesthesia: a split-mouth randomized controlled clinical trial
- Analgesic effect of ropivacaine with fentanyl in comparison with ropivacaine alone for continuous femoral nerve block after knee replacement arthroplasty: a prospective, randomized, double-blinded study
- A comparison of the influence of 2.7% sorbitol-0.54% mannitol and 5% glucose irrigating fluids on plasma serum physiology during hysteroscopic procedures
- Pulmonary edema during hysteroscopic surgery: Three cases report