COVID-19 and vaccination during pregnancy: a systematic analysis using Korea National Health Insurance claims data
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Korea University College of Medicine, Seoul, Korea
- 2School of Industrial Management Engineering, Korea University, Seoul, Korea
- 3AI Center, Korea University Anam Hospital, Seoul, Korea
- 4Department of Pediatrics, Korea University College of Medicine, Seoul, Korea
- KMID: 2535957
- DOI: http://doi.org/10.5468/ogs.22060
Abstract
Objective
This study systematically analyzed coronavirus disease 2019 (COVID-19) and vaccination details during pregnancy by using the national health insurance claims data.
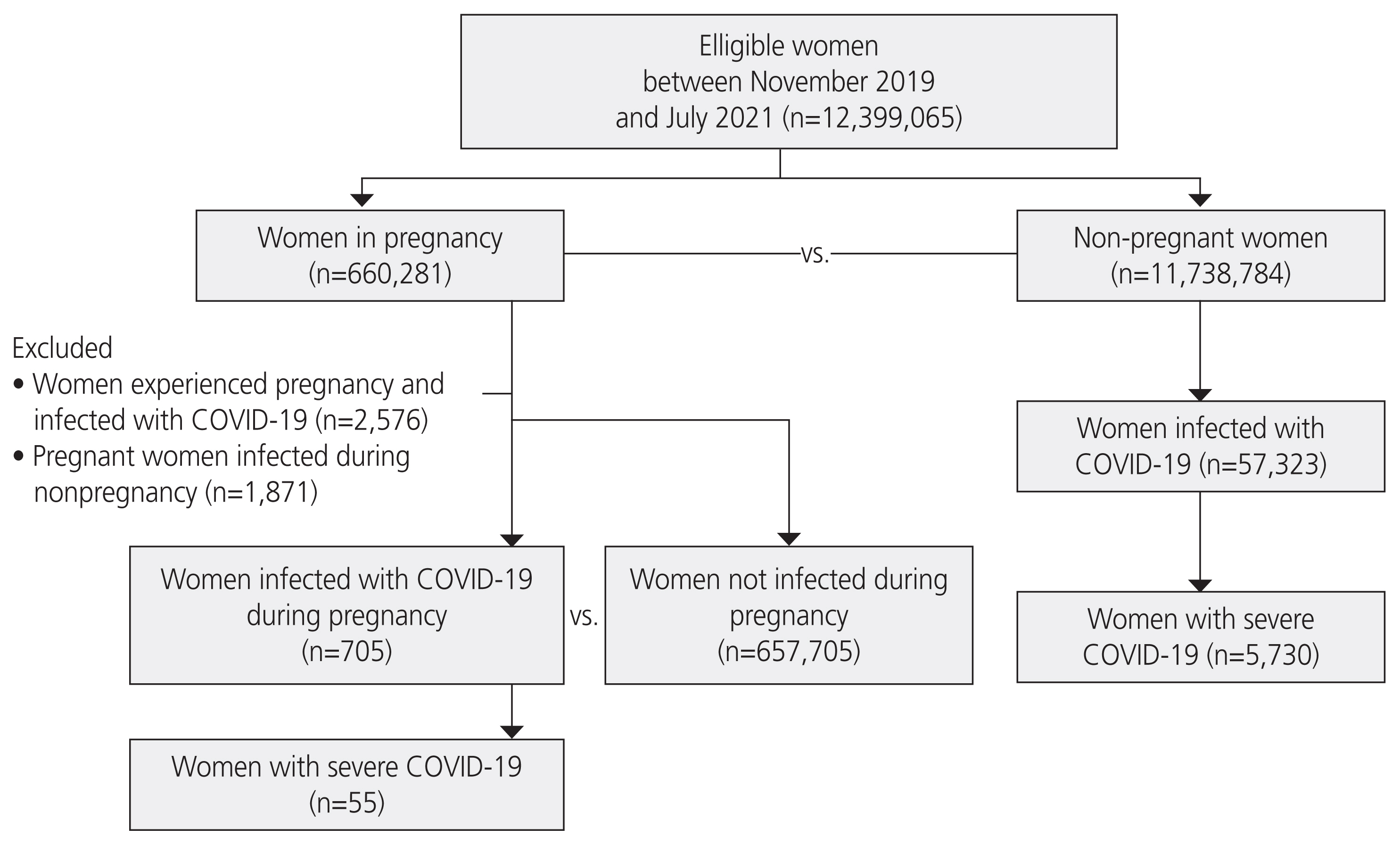
Methods
Population-based retrospective cohort data of 12,399,065 women aged 15-49 years were obtained from the Korea National Health Insurance Service claims database between 2019 and 2021. Univariate analysis was performed to compare the obstetric outcomes of pregnant women (ICD-10 O00-O94) and their newborns (ICD-10 P00-P96) with and without COVID-19. Univariate analysis was also performed to compare the age and obstetric outcomes of pregnant women receiving different types of vaccines.
Results
The percentage of pregnant women with COVID-19 during pregnancy was 0.11%. Some obstetric outcomes of pregnant women with COVID-19, including the rates of preterm birth or cesarean delivery, were significantly better than those of pregnant women without COVID-19. The rate of miscarriage was higher in pregnant women with COVID-19 than without COVID-19. However, the outcomes of newborns of women with and without COVID-19 were not significantly different. Regarding vaccination type, obstetric outcomes of pregnant women appeared to be worse with the viral vector vaccine than with the mRNA vaccine.
Conclusion
To the best of our knowledge, this is the first study to systematically analyze COVID-19 and vaccination details during pregnancy using the national health insurance claims data in Korea. The obstetric outcomes in pregnant women with and without COVID-19 and their newborns were similar.
Keyword
Figure
Cited by 4 articles
-
The introduction to air pollution on pregnancy outcome (APPO) study: a multicenter cohort study
Young Min Hur, Sunwha Park, Eunjin Kwon, Young-Ah You, AbuZar Ansari, Soo Min Kim, Gain Lee, Mi Hye Park, Kyung A Lee, Soo Jung Kim, Young-Han Kim, Yeon-Sung Jung, Geum Joon Cho, Min-Jeong Oh, Sung Hun Na, Se Jin Lee, Tae Gyu An, Jin-Gon Bae, Yu-Hwan Kim, Soo-Jeong Lee, Na Kyung Kim, Eun-Hee Ha, Young Ju Kim
Obstet Gynecol Sci. 2023;66(3):169-180. doi: 10.5468/ogs.22278.Pregnancy and COVID-19: past, present and future
Young Keun Kim, Eui Hyeok Kim
Obstet Gynecol Sci. 2023;66(3):149-160. doi: 10.5468/ogs.23001.The coronavirus disease 2019 infection in pregnancy and adverse pregnancy outcomes: a systematic review and meta-analysis
Yeonsong Jeong, Min-A Kim
Obstet Gynecol Sci. 2023;66(4):270-289. doi: 10.5468/ogs.22323.Trends, statistics, and policy recommendations on maternal, fetal, and infant mortality before and after COVID-19: a review of the past decade (2012-2022) based on national health information data
Kyung Ju Lee, Seokmin Lee
Obstet Gynecol Sci. 2025;68(1):59-68. doi: 10.5468/ogs.24264.
Reference
-
References
1. Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020; 323:1061–69.2. Yuen KS, Ye ZW, Fung SY, Chan CP, Jin DY. SARS-CoV-2 and COVID-19: the most important research questions. Cell Biosci. 2020; 10:40.3. Wan S, Xiang Y, Fang W, Zheng Y, Li B, Hu Y, et al. Clinical features and treatment of COVID-19 patients in northeast Chongqing. J Med Virol. 2020; 92:797–806.
Article4. Munn MB, Groome LJ, Atterbury JL, Baker SL, Hoff C. Pneumonia as a complication of pregnancy. J Matern Fetal Med. 1999; 8:151–4.5. Goodnight WH, Soper DE. Pneumonia in pregnancy. Crit Care Med. 2005; 33(10 Suppl):S390–7.
Article6. Amirian A, Pakzad R, Hasanpour V, Mirzadeh N, Abdi F. Neonatal outcome among pregnant women with COVID-19: a systematic review and meta-analysis. J Matern Fetal Neonatal Med. 2022; 4:1–15.
Article7. Bae JG, Ha JK, Kwon M, Park HY, Seong WJ, Hong SY. A case of delivery of a pregnant woman with COVID-19 infection in Daegu, Korea. Obstet Gynecol Sci. 2020; 63:745–9.
Article8. Centers for Disease Control and Prevention (CDC). COVID-19 vaccines while pregnant or breastfeeding [Internet]. Atlanta (GA): CDC;c2021. [cited 2021 Apr 18]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/recommendations/pregnancy .9. American College of Obstetricians and Gynecologists (ACOG). The American College of Obstetrics and Gynecology [Internet]. Washington, DC: ACOG;c2021. [cited 2021 Apr 18]. Available from: https://www.acog.org/clinical/clinical-guidance/practice-advisory/articles/2020/12/covid-19-vaccination-considerations-for-obstetric-gynecologic-care .10. Kim HY. Statistical notes for clinical researchers: chi-squared test and Fisher’s exact test. Restor Dent Endod. 2017; 42:152–5.
Article11. Centers for Disease Control and Prevention (CDC). United states centers for disease control and prevention. Investigating the impact of COVID-19 during pregnancy [Internet]. Atlanta (GA): CDC;c2021. [cited 2021Dec 30]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/special-populations/pregnancy-data-on-covid-19/what-cdc-is-doing.html .12. Jamieson DJ, Rasmussen SA. An update on COVID-19 and pregnancy. Am J Obstet Gynecol. 2021; 226:177–86.
Article13. Smith V, Seo D, Warty R, Payne O, Salih M, Chin KL, et al. Maternal and neonatal outcomes associated with COVID-19 infection: a systematic review. PLoS One. 2020; 15:e0234187.
Article14. Yan J, Guo J, Fan C, Juan J, Yu X, Li J, et al. Coronavirus disease 2019 in pregnant women: a report based on 116 cases. Am J Obstet Gynecol. 2020; 223:111e1–111.e14.
Article15. Bellos I, Pandita A, Panza R. Maternal and perinatal outcomes in pregnant women infected by SARS-CoV-2: a meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2021; 256:194–204.
Article16. Cardona-Pérez JA, Villegas-Mota I, Helguera-Repetto AC, Acevedo-Gallegos S, Rodríguez-Bosch M, Aguinaga-Ríos M, et al. Prevalence, clinical features, and outcomes of SARS-CoV-2 infection in pregnant women with or without mild/moderate symptoms: results from universal screening in a tertiary care center in Mexico City, Mexico. PLoS One. 2021; 16:e0249584.
Article17. Akhtar H, Patel C, Abuelgasim E, Harky A. COVID-19 (SARS-CoV-2) infection in pregnancy: a systematic review. Gynecol Obstet Invest. 2020; 85:295–306.
Article18. Abedzadeh-Kalahroudi M, Sehat M, Vahedpour Z, Talebian P, Haghighi A. Clinical and obstetric characteristics of pregnant women with covid-19: a case series study on 26 patients. Taiwan J Obstet Gynecol. 2021; 60:458–462.
Article19. de Medeiros KS, Sarmento ACA, Costa APF, Macêdo LTA, da Silva LAS, de Freitas CL, et al. Consequences and implications of the coronavirus disease (COVID-19) on pregnancy and newborns: a comprehensive systematic review and meta-analysis. Int J Gynaecol Obstet. 2022; 156:394–405.
Article20. Trippella G, Ciarcià M, Ferrari M, Buzzatti C, Maccora I, Azzari C, et al. COVID-19 in pregnant women and neonates: a systematic review of the literature with quality assessment of the studies. Pathogens. 2020; 9:485.21. Selvaratnam RJ, Davey MA, Mol BW, Wallace EM. Increasing obstetric intervention for fetal growth restriction is shifting birthweight centiles: a retrospective cohort study. BJOG. 2020; 127:1074–80.
Article22. Philip RK, Purtill H, Reidy E, Daly M, Imcha M, McGrath D, et al. Unprecedented reduction in births of very low birthweight (VLBW) and extremely low birthweight (ELBW) infants during the COVID-19 lockdown in Ireland: a ‘natural experiment’ allowing analysis of data from the prior two decades. BMJ Glob Health. 2020; 5:e003075.
Article23. Bian Z, Qu X, Ying H, Liu X. Are COVID-19 mitigation measures reducing preterm birth rate in China? BMJ Glob Health. 2021; 6:e006359.
Article24. Korea Disease Control and Prevention Agency (KDCA). COVID-19 breifing [Internet]. Cheongju: KDCA;c2021. [cited 2021 Apr 18]. Available from: http://ncov.mohw.go.kr/supportPolicyBoardList.do .25. Lee H, Lee JR, Jung H, Lee JY. Power of universal health coverage in the era of COVID-19: a nationwide observational study. Lancet Reg Health West Pac. 2021; 7:100088.
Article26. Celewicz A, Celewicz M, Michalczyk M, Woźniakowska-Gondek P, Krejczy K, Misiek M, et al. Pregnancy as a risk factor of severe COVID-19. J Clin Med. 2021; 10:5458.
Article27. Linder N, Linder I, Fridman E, Kouadio F, Lubin D, Merlob P, et al. Birth trauma--risk factors and short-term neonatal outcome. J Matern Fetal Neonatal Med. 2013; 26:1491–5.28. Moczygemba CK, Paramsothy P, Meikle S, Kourtis AP, Barfield WD, Kuklina E, et al. Route of delivery and neonatal birth trauma. Am J Obstet Gynecol. 2010; 202:361e1–6.
Article29. Leik NKO, Ahmedy F, Guad RM, Baharuddin DMP. Covid-19 vaccine and its consequences in pregnancy: brief review. Ann Med Surg (Lond). 2021; 72:103103.
Article30. Lipkind HS, Vazquez-Benitez G, DeSilva M, Vesco KK, Ackerman-Banks C, Zhu J, et al. Receipt of COVID-19 vaccine during pregnancy and preterm or small-for-gestational-age at birth - eight Integrated Health Care Organizations, United States, December 15, 2020–July 22, 2021. MMWR Morb Mortal Wkly Rep. 2022; 71:26–30.
Article31. Shay DK, Gee J, Su JR, Myers TR, Marquez P, Liu R, et al. Safety monitoring of the Janssen (Johnson & Johnson) COVID-19 vaccine - United States, March-April 2021. MMWR Morb Mortal Wkly Rep. 2021; 70:680–4.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Enhancing COVID-19 vaccination coverage using financial incentives: arguments to help health providers counterbalance erroneous claims
- COVID-19 infection and severe clinical outcomes in patients with kidney disease by vaccination status: a nationwide cohort study in Korea
- Sensitivity of Medical Insurance Claims Data Using Population-based Cancer Registry Data
- The Role of COVID-19 Vaccination for Patients With Atherosclerotic Cardiovascular Disease in the Upcoming Endemic Era
- Preparations for the Assessment of COVID-19 Infection and Long-Term Cardiovascular Risk