Neurointervention.
2022 Nov;17(3):152-160. 10.5469/neuroint.2022.00234.
National Trends in Medical Costs and Prognosis of Acute Ischemic Stroke Patients in Endovascular Thrombectomy Era: Analysis Using Medical Claim Data in Korea
- Affiliations
-
- 1Department of Radiology, Ajou University Hospital, Ajou University School of Medicine, Suwon, Korea
- 2Department of Neurology, National Health Insurance Service Ilsan Hospital, Goyang, Korea
- 3Department of Radiology, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2535950
- DOI: http://doi.org/10.5469/neuroint.2022.00234
Abstract
- Purpose
The purpose of this study was to evaluate trends in medical costs and prognosis in acute ischemic stroke (AIS) patients in Korea from 2008 to 2017 using medical claims data.
Materials and Methods
All data for the past decade was collected from a big data hub provided by the Health Insurance Review & Assessment Service. Using several Korean Standard Classification of Disease codes, we estimated the number of patients, the costs of medical insurance, and prognosis according to the treatment with or without endovascular thrombectomy (EVT) among in-patients with AIS.
Results
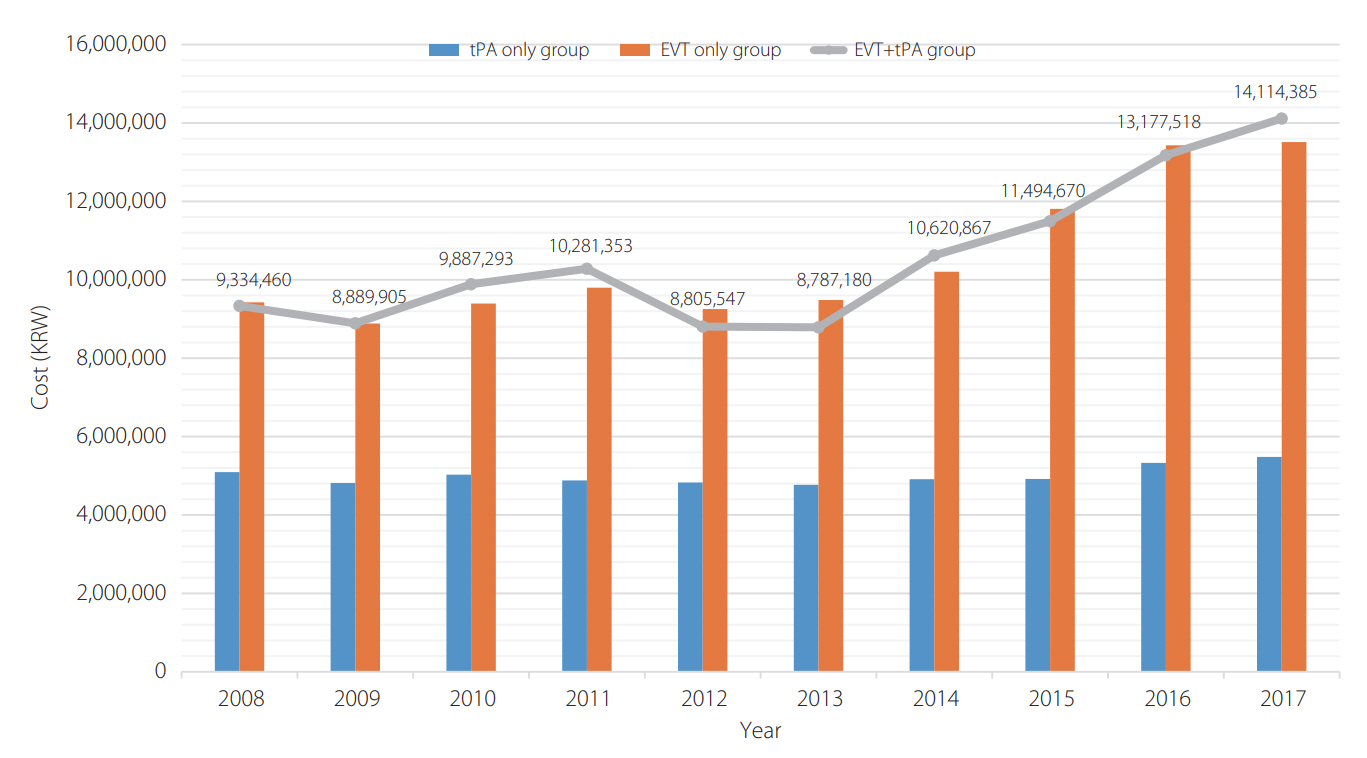
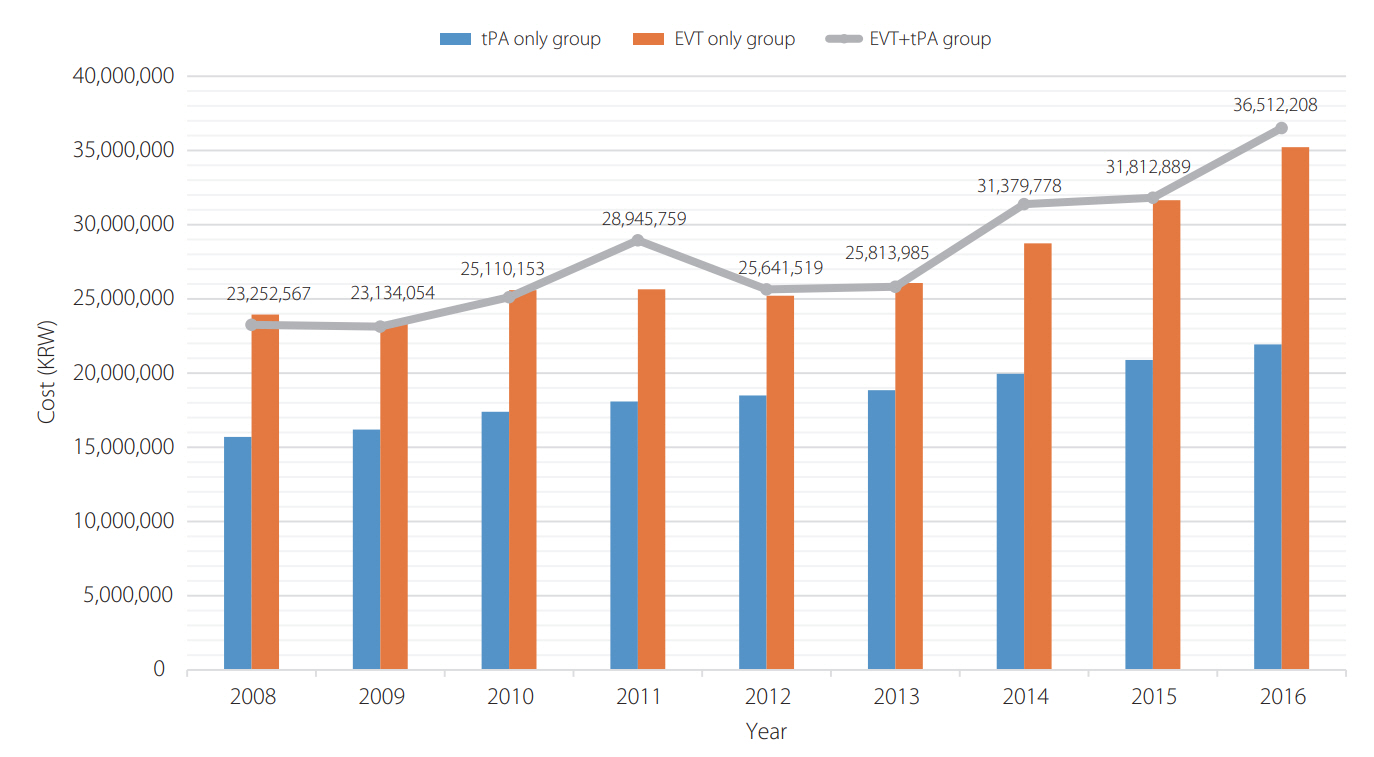
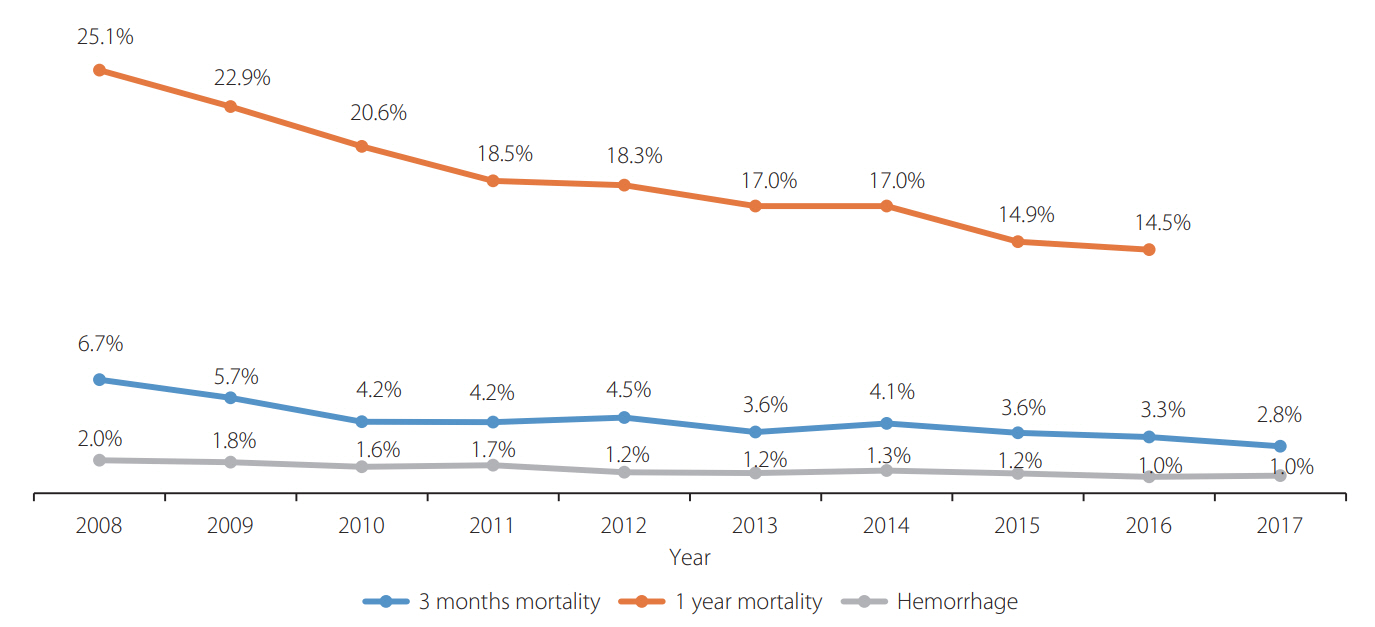
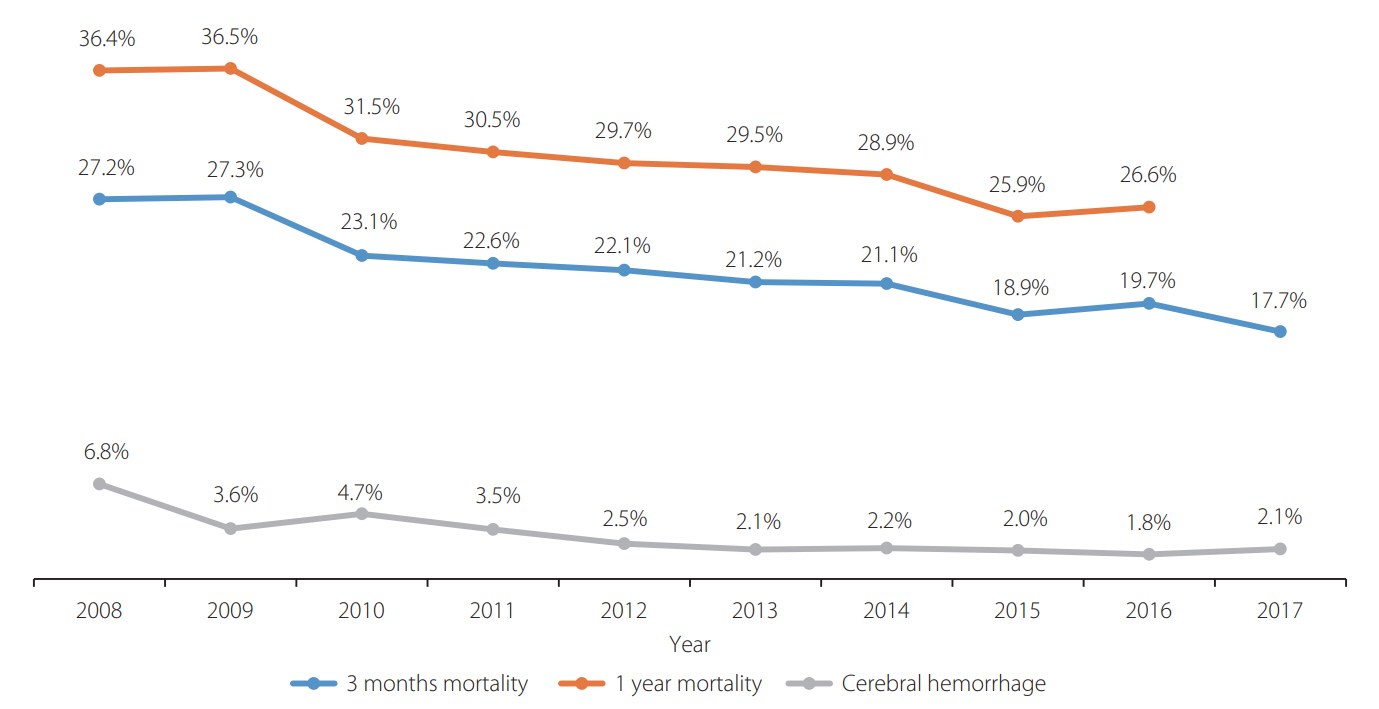
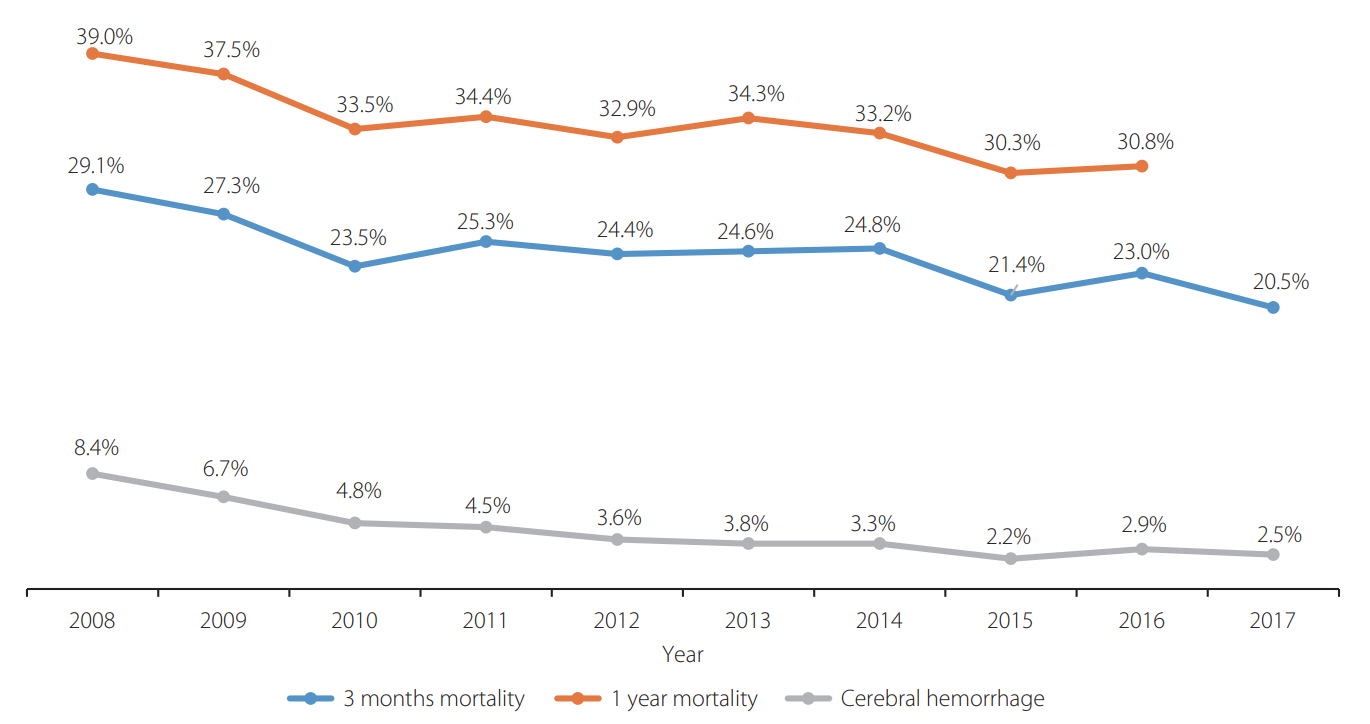
Since 2014, when EVT was covered by insurance, the number of patients who underwent EVT for AIS has increased significantly. Also, in the past decade, the medical costs following inpatient care for AIS with EVT have increased gradually, and the overall medical costs for the first year post-stroke have also increased. The prognosis of AIS patients with EVT was different according to the time of treatment. Annual trends for both mortality and cerebral hemorrhage after treatment of AIS with EVT have gradually decreased.
Conclusion
In this study, we found that both inpatient medical costs and 1-year cumulative medical costs have gradually increased, and the prognosis has gradually improved in patients receiving EVT treatment among AIS patients.
Keyword
Figure
Cited by 1 articles
-
Deep Learning-Based Automatic Classification of Ischemic Stroke Subtype Using Diffusion-Weighted Images
Wi-Sun Ryu, Dawid Schellingerhout, Hoyoun Lee, Keon-Joo Lee, Chi Kyung Kim, Beom Joon Kim, Jong-Won Chung, Jae-Sung Lim, Joon-Tae Kim, Dae-Hyun Kim, Jae-Kwan Cha, Leonard Sunwoo, Dongmin Kim, Sang-Il Suh, Oh Young Bang, Hee-Joon Bae, Dong-Eog Kim
J Stroke. 2024;26(2):300-311. doi: 10.5853/jos.2024.00535.
Reference
-
1. Powers WJ, Derdeyn CP, Biller J, Coffey CS, Hoh BL, Jauch EC, American Heart Association Stroke Council, et al. 2015 American Heart Association/American Stroke Association focused update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2015; 46:3020–3035.
Article2. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, American Heart Association Stroke Council, et al. 2018 Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018; 49:e46–e110.
Article3. National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. Tissue plasminogen activator for acute ischemic stroke. N Engl J Med. 1995; 333:1581–1587.4. Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, MR CLEAN Investigators, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015; 372:11–20.5. Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, EXTEND-IA Investigators, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015; 372:1009–1018.
Article6. Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, ESCAPE Trial Investigators, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015; 372:1019–1030.
Article7. Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, REVASCAT Trial Investigators, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015; 372:2296–2306.
Article8. Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM, SWIFT PRIME Investigators, et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med. 2015; 372:2285–2295.
Article9. Hong KS, Ko SB, Yu KH, Jung C, Park SQ, Kim BM, et al. Update of the Korean clinical practice guidelines for endovascular recanalization therapy in patients with acute ischemic stroke. J Stroke. 2016; 18:102–113.
Article10. Seo KD, Suh SH. Endovascular treatment in acute ischemic stroke: a nationwide survey in Korea. Neurointervention. 2018; 13:84–89.
Article11. Furlan AJ. Stent-retriever thrombectomy for stroke. N Engl J Med. 2015; 373:1078.
Article12. Ko SB, Park HK, Kim BM, Heo JH, Rha JH, Kwon SU, et al. 2019 Update of the Korean clinical practice guidelines of stroke for endovascular recanalization therapy in patients with acute ischemic stroke. J Stroke. 2019; 21:231–240.
Article13. Saber H, Navi BB, Grotta JC, Kamel H, Bambhroliya A, Vahidy FS, et al. Real-world treatment trends in endovascular stroke therapy. Stroke. 2019; 50:683–689.
Article14. Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P, DAWN Trial Investigators, et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. 2018; 378:11–21.15. Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, Ortega-Gutierrez S, DEFUSE 3 Investigators, et al. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. 2018; 378:708–718.
Article16. Lim SJ, Kim HJ, Nam CM, Chang HS, Jang YH, Kim S, et al. Socioeconomic costs of stroke in Korea: estimated from the Korea national health insurance claims database. J Prev Med Public Health. 2009; 42:251–260.
Article17. Kim JY, Kang K, Kang J, Koo J, Kim DH, Kim BJ, et al. Executive summary of stroke statistics in Korea 2018: a report from the Epidemiology Research Council of the Korean Stroke Society. J Stroke. 2019; 21:42–59.
Article18. Zhai S, Gardiner F, Neeman T, Jones B, Gawarikar Y. The cost-effectiveness of a stroke unit in providing enhanced patient outcomes in an Australian teaching hospital. J Stroke Cerebrovasc Dis. 2017; 26:2362–2368.
Article19. Yoo SD, Jeong YS, Kim TW. Medical rehabilitation system for patients in acute rehabilitation units. J Korean Med Assoc. 2017; 60:864–869.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intravenous Thrombolysis and Endovascular Thrombectomy in Acute Ischemic Stroke with Minor Symptom
- Endovascular Treatment of Acute Ischemic Stroke
- An Update of Recent Guideline for the Endovascular Recanalization Therapy in Acute Ischemic Stroke
- Differences in Effectiveness among Devices for Endovascular Thrombectomy in Patients with Acute Ischemic Stroke
- The Clinical Benefit and Care Burden of Extending the Window of Endovascular Thrombectomy for Stroke in the Emergency Room