J Korean Soc Matern Child Health.
2022 Oct;26(4):283-288. 10.21896/jksmch.2022.26.4.283.
Association Between Female Bony Pelvimetry Using Magnetic Resonance Imaging and Cesarean Delivery due to Cephalopelvic Disproportion
- Affiliations
-
- 1Department of Obstetrics and Gynecology, CHA Bundang Medical Center, CHA University School of Medicine, Seongnam, Korea
- KMID: 2535918
- DOI: http://doi.org/10.21896/jksmch.2022.26.4.283
Abstract
- Purpose
To analyze the difference in bony pelvimetry using magnetic resonance imaging (MRI) in women who delivered vaginally and those who underwent cesarean section (CS) due to cephalopelvic disproportion (CPD).
Methods
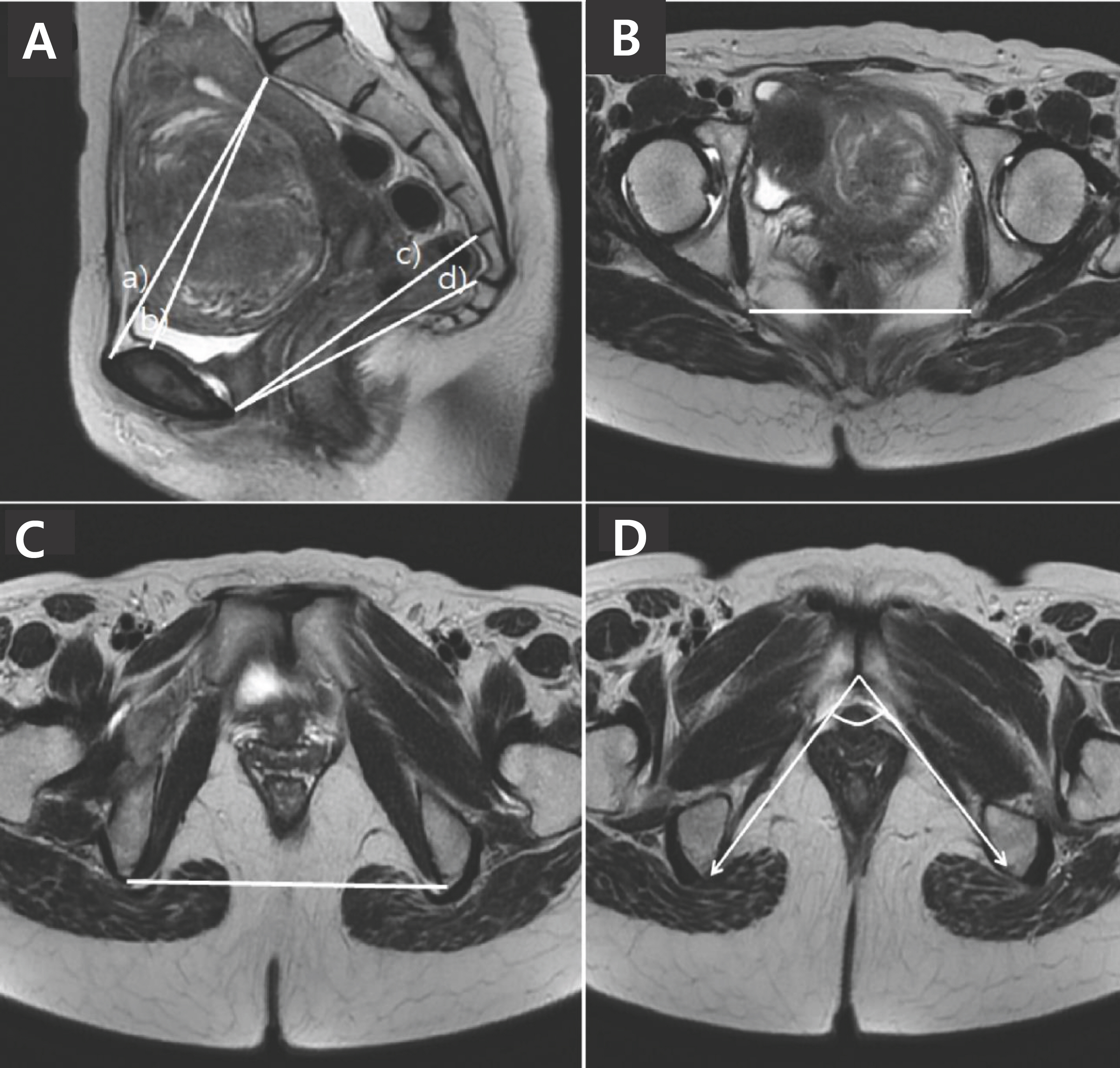
This retrospective case-control study enrolled Korean women who gave birth to their first child between 37 and 42 weeks of pregnancy and underwent pelvic MRI between January 2014 and June 2020. These women were classified into 3 groups: vaginal delivery (VD), CS due to CPD (CPD-CS), and CS due to reasons other than CPD (Other-CS). In MRI images, true conjugate (TC), obstetric conjugate (OC), mid anterior-posterior (AP) distance (MAD), outlet AP distance (OAD), ischial spine distance (ISD), ischial tuberosity distance (ITD), and pubic angle (PA) were measured.
Results
In total, 392 women were enrolled. There were no significant differences in maternal height and body mass index at birth among the 3 groups. The ISD was statistically different between the VD group (106.2±6.4 mm) and the Other-CS group (110.4±8.8 mm) (p=0.014). After multiple regression analysis, short ISD (adjusted odds ratio [aOR], 0.92; 95% confidence interval [CI], 0.87-0.97; p=0.002), short MAD (aOR, 0.95; 95% CI, 0.89-0.99; p=0.047), and short ITD (aOR, 0.95; 95% CI, 0.91-0.99; p=0.019) were significantly associated with CS due to CPD.
Conclusion
Short ISD, MAD, and ITD, measured using MRI, are important parameters that can predict CS due to CPD. The accumulation of related research could promote the development of an excellent imaging method in terms of cost-effectiveness. Thus, it may be possible to establish a method to reduce obstetric and perinatal complications due to dystonia.
Figure
Reference
-
Aronson D., Kier R. CT pelvimetry: the foveae are not an accurate landmark for the level of the ischial spines. AJR Am J Roentgenol. 1991. 156:527–30.
ArticleChen HY., Chen YP., Lee LS., Huang SC. Pelvimetry of Chinese females with special reference to pelvic type and maternal height. Int Surg. 1982. 67:57–62.Fasler T., Burkhardt T., Wisser J., Keller T., Kurmanavicius J. Does a combination of foetal biometry and maternal MRI pelvimetry decrease the frequency of secondary caesarean section? Z Ge- burtshilfe Neonatol. 2010. 214:68–73.Gerace JR. The midpelvis in pelvimetry. Can Med Assoc J. 1959. 80:166–8.Gowri V., Jain R., Rizvi S. Magnetic resonance pelvimetry for trial of labour after a previous caesarean section. Sultan Qaboos Univ Med J. 2010. 10:210–4.Klemt AS., Schulze S., Brüggmann D., Louwen F. MRI-based pelvimetric measurements as predictors for a successful vaginal breech delivery in the Frankfurt Breech at term cohort (FRABAT). Eur J Obstet Gynecol Reprod Biol. 2019. 232:10–7.
ArticleKorhonen U., Taipale P., Heinonen S. Fetal pelvic index to predict cephalopelvic disproportion - a retrospective clinical cohort study. Acta Obstet Gynecol Scand. 2015. 94:615–21.Liselele HB., Tshibangu CK., Meuris S. Association between external pelvimetry and vertex delivery complications in African women. Acta Obstet Gynecol Scand. 2000. 79:673–8.
ArticleMaharaj D. Assessing cephalopelvic disproportion: back to the basics. Obstet Gynecol Surv. 2010. 65:387–95.
ArticleMartinsen AC., Risdal M., Bay T., Drolsum A. Pelvimetry with compute tomography. Tidsskr Nor Laegeforen. 2005. 125:2023–5.Mendez-Dominguez N., Vazquez-Vazquez GG., Laviada-Molina HA., de Jesus Inurreta-Diaz M., Fajardo-Ruiz LS., Azcorra H. Cephalo- pelvic disproportion as primary diagnosis for cesarean section: Role of neonatal birthweight in relation to maternal height at a Hospital in Merida, Mexico. Am J Hum Biol. 2021. 33:e23463.Nelson DB., Alexander JM., McIntire DD., Leveno KJ. ‘New or not-so-new’ labor management practices and cesarean delivery for arrest of progress. Am J Obstet Gynecol. 2020. 222:71.e1–71.e6.
ArticleOboro VO., Ande AB., Olagbuji BN., Ezeanochie MC., Aderoba A., Ir- hibogbe I. Influence of maternal height on mode of delivery in Nigerian women. Niger Postgrad Med J. 2010. 17:223–6.Pattinson RC. Pelvimetry for fetal cephalic presentations at term. Cochrane Database Syst Rev. 2000. 2:CD000161.Pattinson RC., Cuthbert A., Vannevel V. Pelvimetry for fetal cephalic presentations at or near term for deciding on mode of delivery. Cochrane Database Syst Rev. 2017. 3:CD000161.
ArticlePerlman S., Raviv-Zilka L., Levinsky D., Gidron A., Achiron R., Gilboa Y, et al. The birth canal: correlation between the pubic arch angle, the interspinous diameter, and the obstetrical conjugate: a com- puted tomography biometric study in reproductive age women. J Matern Fetal Neonatal Med. 2019. 32:3255–65.Rozenberg P. Is there a role for X-ray pelvimetry in the twenty-first century? Gynecol Obstet Fertil. 2007. 35:6–12.Rozenholc AT., Ako SN., Leke RJ., Boulvain M. The diagnostic accuracy of external pelvimetry and maternal height to predict dystocia in nulliparous women: a study in Cameroon. BJOG. 2007. 114:630–5.
ArticleSalk I., Cetin A., Salk S., Cetin M. Pelvimetry by three-dimensional computed tomography in non-pregnant multiparous women who delivered vaginally. Pol J Radiol. 2016. 81:219–27.
ArticleSheiner E., Levy A., Katz M., Mazor M. Short stature–an independent risk factor for Cesarean delivery. Eur J Obstet Gynecol Reprod Biol. 2005. 120:175–8.
ArticleShirley MK., Cole TJ., Arthurs OJ., Clark CA., Wells JCK. Developmental origins of variability in pelvic dimensions: Evidence from nulli- parous South Asian women in the United Kingdom. Am J Hum Biol. 2020. 32:e23340.Toh-Adam R., Srisupundit K., Tongsong T. Short stature as an inde- pendent risk factor for cephalopelvic disproportion in a country of relatively small-sized mothers. Arch Gynecol Obstet. 2012. 285:1513–6.
ArticleZaretsky MV., Alexander JM., McIntire DD., Hatab MR., Twickler DM., Leveno KJ. Magnetic resonance imaging pelvimetry and the pre- diction of labor dystocia. Obstet Gynecol. 2005. 106:919–26.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Maternal Height and the Risk of Cesarean Delivery Due to Cephalopelvic Disproportion in Nulliparous Women
- Measurement of retropubic tissue thickness using intrapartum transperineal ultrasound to assess cephalopelvic disproportion
- A Case of Hypoglycemia following Cesarean Section
- Clinical Survey of Fetal Macrosomia
- Decision Making about Mode of Delivery Among Pregnant Women with Previous Cesarean Delivery