Intest Res.
2022 Oct;20(4):482-494. 10.5217/ir.2021.00161.
Gastrointestinal bleeding risk of non-vitamin K antagonist oral anticoagulants versus warfarin in general and after polypectomy: a population-based study with propensity score matching analysis
- Affiliations
-
- 1Division of Gastroenterology, Department of Internal Medicine, School of Medicine, Kyungpook National University, Daegu, Korea
- 2Division of Cardiology, Department of Internal Medicine, School of Medicine, Kyungpook National University, Daegu, Korea
- 3Data Science Team, Hanmi Pharm. Co., Ltd., Seoul, Korea
- KMID: 2535822
- DOI: http://doi.org/10.5217/ir.2021.00161
Abstract
- Background/Aims
Gastrointestinal bleeding (GIB) risk for non-vitamin K antagonist oral anticoagulants (NOACs) compared with warfarin is largely unknown. We aimed to determine the risk of overall and post-polypectomy GIB for NOACs and warfarin.
Methods
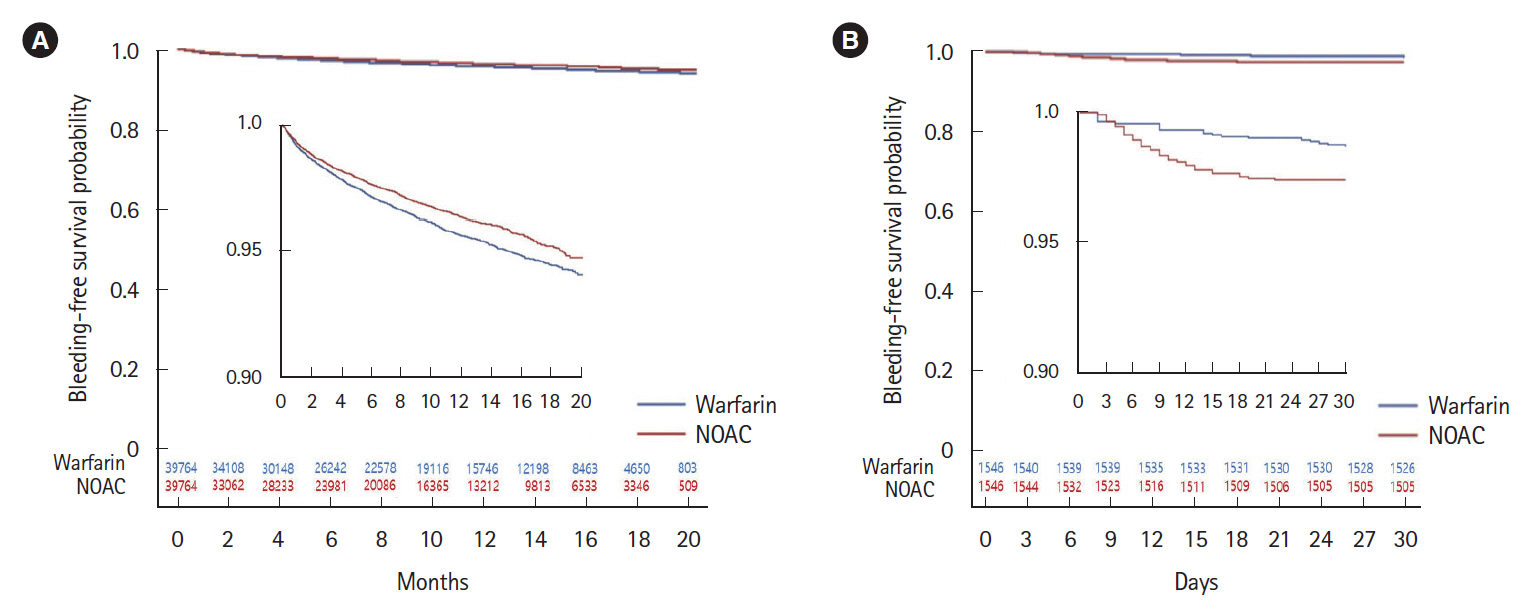
Using the Korean National Health Insurance database, we created a cohort of patients who were newly prescribed NOACs or warfarin between July 2015 and December 2017 using propensity score matching (PSM). Kaplan-Meier analysis with log-rank test was performed to compare the risk of overall and post-polypectomy GIB between NOACs (apixaban, dabigatran, and rivaroxaban) and warfarin. Post-polypectomy GIB was defined as bleeding within 1 month after gastrointestinal endoscopic polypectomy.
Results
Out of 234,206 patients taking anticoagulants (187,687 NOACs and 46,519 warfarin), we selected 39,764 pairs of NOACs and warfarin users after PSM. NOACs patients showed significantly lower risk of overall GIB than warfarin patients (log-rank P<0.001, hazard ratio, 0.86; 95% confidence interval, 0.78–0.94; P=0.001). Among NOACs, apixaban showed the lowest risk of GIB. In the subgroup of 7,525 patients who underwent gastrointestinal polypectomy (lower gastrointestinal polypectomy 93.1%), 1,546 pairs were chosen for each group after PSM. The NOACs group showed a high risk of post-polypectomy GIB compared with the warfarin group (log-rank P=0.001, hazard ratio, 1.97; 95% confidence interval, 1.16–3.33; P=0.012).
Conclusions
This nationwide, population-based study demonstrates that risk of overall GIB is lower for NOACs than for warfarin, while risk of post-polypectomy GIB is higher for NOACs than for warfarin.
Keyword
Figure
Reference
-
1. Mega JL, Simon T. Pharmacology of antithrombotic drugs: an assessment of oral antiplatelet and anticoagulant treatments. Lancet. 2015; 386:281–291.
Article2. Ruff CT, Giugliano RP, Braunwald E, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet. 2014; 383:955–962.
Article3. Kirley K, Qato DM, Kornfield R, Stafford RS, Alexander GC. National trends in oral anticoagulant use in the United States, 2007 to 2011. Circ Cardiovasc Qual Outcomes. 2012; 5:615–621.
Article4. Abraham NS, Castillo DL. Novel anticoagulants: bleeding risk and management strategies. Curr Opin Gastroenterol. 2013; 29:676–683.5. Connolly SJ, Ezekowitz MD, Yusuf S, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009; 361:1139–1151.
Article6. Patel MR, Mahaffey KW, Garg J, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011; 365:883–891.
Article7. Cangemi DJ, Krill T, Weideman R, Cipher DJ, Spechler SJ, Feagins LA. A comparison of the rate of gastrointestinal bleeding in patients taking non-vitamin K antagonist oral anticoagulants or warfarin. Am J Gastroenterol. 2017; 112:734–739.
Article8. Abraham NS, Singh S, Alexander GC, et al. Comparative risk of gastrointestinal bleeding with dabigatran, rivaroxaban, and warfarin: population based cohort study. BMJ. 2015; 350:h1857.
Article9. Adeboyeje G, Sylwestrzak G, Barron JJ, et al. Major bleeding risk during anticoagulation with warfarin, dabigatran, apixaban, or rivaroxaban in patients with nonvalvular atrial fibrillation. J Manag Care Spec Pharm. 2017; 23:968–978.
Article10. Cheol Seong S, Kim YY, Khang YH, et al. Data resource profile: the National Health Information Database of the National Health Insurance Service in South Korea. Int J Epidemiol. 2017; 46:799–800.
Article11. Cha JM, Kim HS, Kwak MS, et al. Features of postcolonoscopy colorectal cancer and survival times of patients in Korea. Clin Gastroenterol Hepatol. 2019; 17:786–788.
Article12. Nagata N, Yasunaga H, Matsui H, et al. Therapeutic endoscopy-related GI bleeding and thromboembolic events in patients using warfarin or direct oral anticoagulants: results from a large nationwide database analysis. Gut. 2018; 67:1805–1812.
Article13. Niikura R, Yasunaga H, Yamada A, et al. Factors predicting adverse events associated with therapeutic colonoscopy for colorectal neoplasia: a retrospective nationwide study in Japan. Gastrointest Endosc. 2016; 84:971–982.
Article14. Brodie MM, Newman JC, Smith T, Rockey DC. Severity of gastrointestinal bleeding in patients treated with direct-acting oral anticoagulants. Am J Med. 2018; 131:573.e9–573.e15.
Article15. Feagins LA, Weideman RA. GI bleeding risk of DOACs versus warfarin: is newer better? Dig Dis Sci. 2018; 63:1675–1677.
Article16. Joseph DA, Meester RG, Zauber AG, et al. Colorectal cancer screening: estimated future colonoscopy need and current volume and capacity. Cancer. 2016; 122:2479–2486.
Article17. Tien A, Kwok K, Dong E, et al. Impact of direct-acting oral anticoagulants and warfarin on postendoscopic GI bleeding and thromboembolic events in patients undergoing elective endoscopy. Gastrointest Endosc. 2020; 92:284–292.
Article18. Yanagisawa N, Nagata N, Watanabe K, et al. Post-polypectomy bleeding and thromboembolism risks associated with warfarin vs direct oral anticoagulants. World J Gastroenterol. 2018; 24:1540–1549.
Article19. Chan FKL, Goh KL, Reddy N, et al. Management of patients on antithrombotic agents undergoing emergency and elective endoscopy: joint Asian Pacific Association of Gastroenterology (APAGE) and Asian Pacific Society for Digestive Endoscopy (APSDE) practice guidelines. Gut. 2018; 67:405–417.
Article20. ASGE Standards of Practice Committee, Acosta RD, Abraham NS, et al. The management of antithrombotic agents for patients undergoing GI endoscopy. Gastrointest Endosc. 2016; 83:3–16.
Article21. Lau LH, Guo CL, Yip TC, et al. Risks of post-colonoscopic polypectomy bleeding and thromboembolism with warfarin and direct oral anticoagulants: a population-based analysis. Gut. 2022; 71:100–110.
Article22. Granger CB, Alexander JH, McMurray JJ, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011; 365:981–992.
Article23. Holster IL, Valkhoff VE, Kuipers EJ, Tjwa E. New oral anticoagulants increase risk for gastrointestinal bleeding: a systematic review and meta-analysis. Gastroenterology. 2013; 145:105–112.
Article24. Kohsaka S, Murata T, Izumi N, Katada J, Wang F, Terayama Y. Bleeding risk of apixaban, dabigatran, and low-dose rivaroxaban compared with warfarin in Japanese patients with nonvalvular atrial fibrillation: a propensity matched analysis of administrative claims data. Curr Med Res Opin. 2017; 33:1955–1963.
Article25. Ray WA, Chung CP, Murray KT, et al. Association of oral anticoagulants and proton pump inhibitor cotherapy with hospitalization for upper gastrointestinal tract bleeding. JAMA. 2018; 320:2221–2230.
Article26. Lanas Á, Carrera-Lasfuentes P, Arguedas Y, et al. Risk of upper and lower gastrointestinal bleeding in patients taking nonsteroidal anti-inflammatory drugs, antiplatelet agents, or anticoagulants. Clin Gastroenterol Hepatol. 2015; 13:906–912.
Article27. Washio E, Esaki M, Maehata Y, et al. Proton pump inhibitors increase incidence of nonsteroidal anti-inflammatory druginduced small bowel injury: a randomized, placebo-controlled trial. Clin Gastroenterol Hepatol. 2016; 14:809–815.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Adaptation of New Oral Anticoagulants for Warfarin Anticoagulated Patient with Traumatic Ongoing Hemorrhage
- Effect of Non-vitamin K Antagonist Oral Anticoagulants in Atrial Fibrillation Patients with Newly Diagnosed Cancer
- Comparison of Early Complications of Oral Anticoagulants after Totally Thoracoscopic Ablation: Warfarin versus Non-vitamin K Antagonist Oral Anticoagulants
- Risk Factors of Gastrointestinal Bleeding in Patients Receiving New Oral Anticoagulants
- Heart Failure as a Risk Factor for Stroke