Healthc Inform Res.
2022 Oct;28(4):376-386. 10.4258/hir.2022.28.4.376.
Simulation Education Incorporating Academic Electronic Medical Records for Undergraduate Nursing Students: A Pilot Study
- Affiliations
-
- 1College of Nursing and Brain Korea 21 FOUR Project, Yonsei University, Seoul, Korea
- 2Department of Nursing, Inha University, Incheon, Korea
- 3College of Nursing, Chungnam National University, Daejeon, Korea
- 4College of Nursing, Gachon University, Incheon, Korea
- 5Department of Nursing, College of Life & Health Sciences, Hoseo University, Cheonan, Korea
- 6Mo-Im Kim Nursing Research Institute, College of Nursing, Yonsei University, Seoul, Korea
- KMID: 2535812
- DOI: http://doi.org/10.4258/hir.2022.28.4.376
Abstract
Objectives
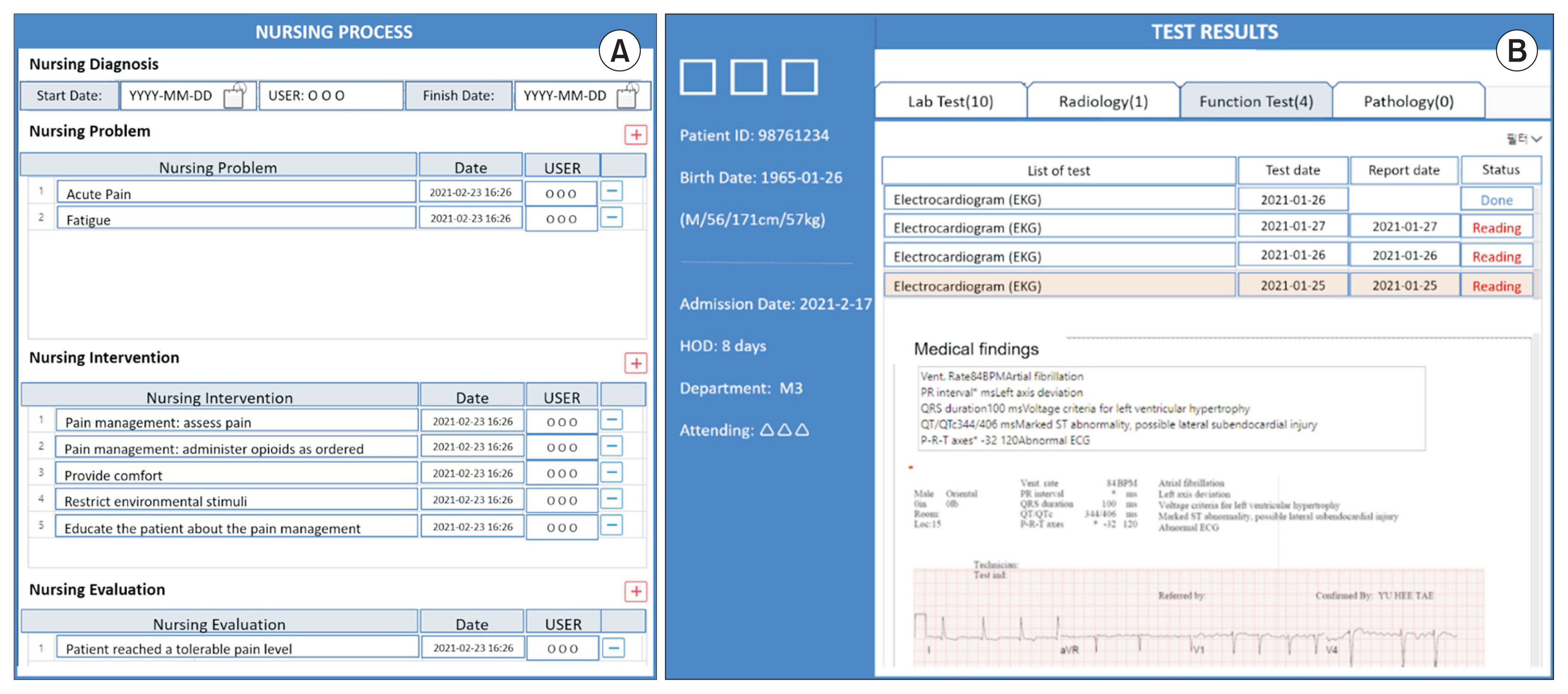
Academic electronic medical records (AEMRs) can be utilized for a variety of educational programs that can enhance nursing students’ nursing informatics and clinical reasoning competencies. This study aimed to identify the applicability and effectiveness of simulation education incorporating AEMRs.
Methods
We developed simulation education scenarios incorporating AEMRs and evaluated them with 76 third- and fourth-year nursing students from five nursing schools using a mixed-methods design. We incorporated three simulation case scenarios involving preeclampsia, diabetes mellitus, and myocardial infarction into the AEMRs. After the simulation education, participants’ feedback on the usability of the AEMR system and their self-efficacy for AEMR utilization were collected via self-reported surveys. Subsequently, the simulation education incorporating AEMRs was evaluated through a focus group interview. The survey data were examined using descriptive statistics, and thematic analysis was done for the focus group interview data.
Results
The average mean scores for the AEMR system’s usability and participants’ self-efficacy for AEMR utilization were 5.36 of 7 and 3.96 of 5, respectively. According to the focus group interviews, the participants were satisfied with the simulation education incorporating AEMRs and recognized their confidence in AEMR utilization. In addition, participants addressed challenges to simulation education incorporating AEMRs, including the need for pre-education and AEMR utilization difficulties.
Conclusions
Nursing students were satisfied with and recognized the value of simulation education incorporating AEMRs. Although the actual application of simulation education incorporating AEMRs remains challenging, further research can help develop and implement this approach for nursing students.
Keyword
Figure
Reference
-
References
1. Organisation for Economic Co-operation and Development. Strengthening health information infrastructure for health care quality governance: good practices, new opportunities and data privacy protection challenges. Paris, France: Organisation for Economic Co-operation and Development;2013.2. Institute of Medicine Health professions education: a bridge to quality. Washington (DC): National Academies Press;2003.3. American Association of Colleges of Nursing. The essentials: core competencies for professional nursing education [Internet]. Washington (DC): American Association of Colleges of Nursing;2021. [cited at 2022 Oct 10]. Available from: https://nursing.byu.edu/Documents/academics/undergrad/EssentialAbilities-Document19.pdf .4. Forman TM, Armor DA, Miller AS. A review of clinical informatics competencies in nursing to inform best practices in education and nurse faculty development. Nurs Educ Perspect. 2020; 41(1):E3–7. https://doi.org/10.1097/01.nep.0000000000000588 .
Article5. Jones S, Donelle L. Assessment of electronic health record usability with undergraduate nursing students. Int J Nurs Educ Scholarsh. 2011; 8:24. https://doi.org/10.2202/1548-923x.2123 .
Article6. Choi M, Lee HS, Park JH. Usability of academic electronic medical record application for nursing students’ clinical practicum. Healthc Inform Res. 2015; 21(3):191–5. https://doi.org/10.4258/hir.2015.21.3.191 .
Article7. Herbert VM, Connors H. Integrating an academic electronic health record: challenges and success strategies. Comput Inform Nurs. 2016; 34(8):345–54. https://doi.org/10.1097/cin.0000000000000264 .
Article8. Choi M, Park JH, Lee HS. Assessment of the need to integrate academic electronic medical records into the undergraduate clinical practicum: a focus group interview. Comput Inform Nurs. 2016; 34(6):259–65. https://doi.org/10.1097/cin.0000000000000244 .
Article9. Mollart L, Newell R, Geale SK, Noble D, Norton C, O’Brien AP. Introduction of patient electronic medical records (EMR) into undergraduate nursing education: an integrated literature review. Nurse Educ Today. 2020; 94:104517. https://doi.org/10.1016/j.nedt.2020.104517 .
Article10. Abrahamson K, Anderson JG, Borycki EM, Kushniruk AW, Malovec S, Espejo A, et al. The impact of university provided nurse electronic medical record training on health care organizations: an exploratory simulation approach. Stud Health Technol Inform. 2015; 208:1–6. https://doi.org/10.3233/978-1-61499-488-6-1 .
Article11. Jung SY, Hwang H, Lee K, Lee D, Yoo S, Lim K, et al. User perspectives on barriers and facilitators to the implementation of electronic health records in behavioral hospitals: qualitative study. JMIR Form Res. 2021; 5(4):e18764. https://doi.org/10.2196/18764 .
Article12. Chung J, Cho I. The need for academic electronic health record systems in nurse education. Nurse Educ Today. 2017; 54:83–8. https://doi.org/10.1016/j.nedt.2017.04.018 .
Article13. Elliott K, Marks-Maran D, Bach R. Teaching student nurses how to use electronic patient records through simulation: a case study. Nurse Educ Pract. 2018; 30:7–12. https://doi.org/10.1016/j.nepr.2018.02.003 .
Article14. Sittner BJ, Aebersold ML, Paige JB, Graham LL, Schram AP, Decker SI, et al. INACSL standards of best practice for simulation: past, present, and future. Nurs Educ Perspect. 2015; 36(5):294–8. https://doi.org/10.5480/15-1670 .
Article15. Choi M, Lee H, Park JH. Effects of using mobile device-based academic electronic medical records for clinical practicum by undergraduate nursing students: a quasi-experimental study. Nurse Educ Today. 2018; 61:112–9. https://doi.org/10.1016/j.nedt.2017.11.018 .
Article16. Whang JH, Kim DH. An empirical study on the critical factors for successful m-learning implementation. J Inf Technol Appl Manag. 2005; 12(3):57–80.17. Vijayalakshmi P, Math SB. Response and attitudes of undergraduate nursing students towards computers in health care. Can J Nurs Inf. 2013; 8(3):1–8.18. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006; 3(2):77–101. https://doi.org/10.1191/1478088706qp063oa .
Article19. Jang A, Park H. Clinical judgment model-based nursing simulation scenario for patients with upper gastro-intestinal bleeding: a mixed methods study. PLoS One. 2021; 16(5):e0251029. https://doi.org/10.1371/journal.pone.0251029 .
Article20. Li J, Li X, Gu L, Zhang R, Zhao R, Cai Q, et al. Effects of simulation-based deliberate practice on nursing students’ communication, empathy, and self-efficacy. J Nurs Educ. 2019; 58(12):681–9. https://doi.org/10.3928/01484834-20191120-02 .
Article21. Yang F, Wang Y, Yang C, Zhou MH, Shu J, Fu B, et al. Improving clinical judgment by simulation: a randomized trial and validation of the Lasater clinical judgment rubric in Chinese. BMC Med Educ. 2019; 19(1):20. https://doi.org/10.1186/s12909-019-1454-9 .
Article22. Kuiper R, O’Donnell SM, Pesut DJ, Turrise SL. 2017 The essentials of clinical reasoning for nurses: using the outcome-present state test model for reflective practice. Indianapolis (IN): Sigma Theta Tau International;2017.23. Page-Cutrara K. Use of prebriefing in nursing simulation: a literature review. J Nurs Educ. 2014; 53(3):136–41. https://doi.org/10.3928/01484834-20140211-07 .
Article24. Dileone C, Chyun D, Diaz DA, Maruca AT. An examination of simulation prebriefing in nursing education: an integrative review. Nurs Educ Perspect. 2020; 41(6):345–8. https://doi.org/10.1097/01.nep.0000000000000689 .
Article25. Kleib M, Chauvette A, Furlong K, Nagle L, Slater L, Mc-Closkey R. Approaches for defining and assessing nursing informatics competencies: a scoping review. JBI Evid Synth. 2021; 19(4):794–841. https://doi.org/10.11124/jbies-20-00100 .
Article26. Vana KD, Silva GE. Evaluating the use of a simulated electronic health record and online drug reference in a case study to enhance nursing students’ understanding of pharmacologic concepts and resources. Nurse Educ. 2014; 39(4):160–5. https://doi.org/10.1097/nne.0000000000000046 .
Article27. Samadbeik M, Fatehi F, Braunstein M, Barry B, Saremian M, Kalhor F, et al. Education and training on electronic medical records (EMRs) for health care professionals and students: a scoping review. Int J Med Inform. 2020; 142:104238. https://doi.org/10.1016/j.ijmedinf.2020.104238 .
Article28. Behrends M, Paulmann V, Koop C, Foadi N, Mikuteit M, Steffens S. Interdisciplinary teaching of digital competencies for undergraduate medical students: experiences of a teaching project by medical informatics and medicine. Stud Health Technol Inform. 2021; 281:891–5. https://doi.org/10.3233/shti210307 .
Article29. Udelsman B, Chien I, Ouchi K, Brizzi K, Tulsky JA, Lindvall C. Needle in a haystack: natural language processing to identify serious illness. J Palliat Med. 2019; 22(2):179–82. https://doi.org/10.1089/jpm.2018.0294 .
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Usability of Academic Electronic Medical Record Application for Nursing Students' Clinical Practicum
- A Meta-analysis of the Effect of Simulation Based Education: Korean Nurses and Nursing Students
- Exploring Experiences of Psychiatric Nursing Simulations Using Standardized Patients for Undergraduate Students
- Effect of a Simulated Education-based Hypoglycemia Scenario Using a High-fidelity Simulator on Acquisition and Retention of Diabetes Knowledge and Academic Self-efficacy in Nursing Students
- Learning Experience of Undergraduate Nursing Students in Simulation: A Meta-synthesis and Meta-ethnography Study