Ann Rehabil Med.
2022 Oct;46(5):237-247. 10.5535/arm.22039.
Esophageal Motility Disorders in Patients With Esophageal Barium Residue After Videofluoroscopic Swallowing Study
- Affiliations
-
- 1Department of Rehabilitation Medicine, Kangwon National University Hospital, Kangwon National University School of Medicine, Chuncheon, Korea
- 2Division of Gastroenterology and Hepatology, Department of Internal Medicine, Kangwon National University School of Medicine, Chuncheon, Korea
- KMID: 2535741
- DOI: http://doi.org/10.5535/arm.22039
Abstract
Objective
To investigate esophageal motility disorders in patients with esophageal residual barium on chest x-rays after videofluoroscopic swallowing studies (VFSS) through high-resolution esophageal manometry (HREM).
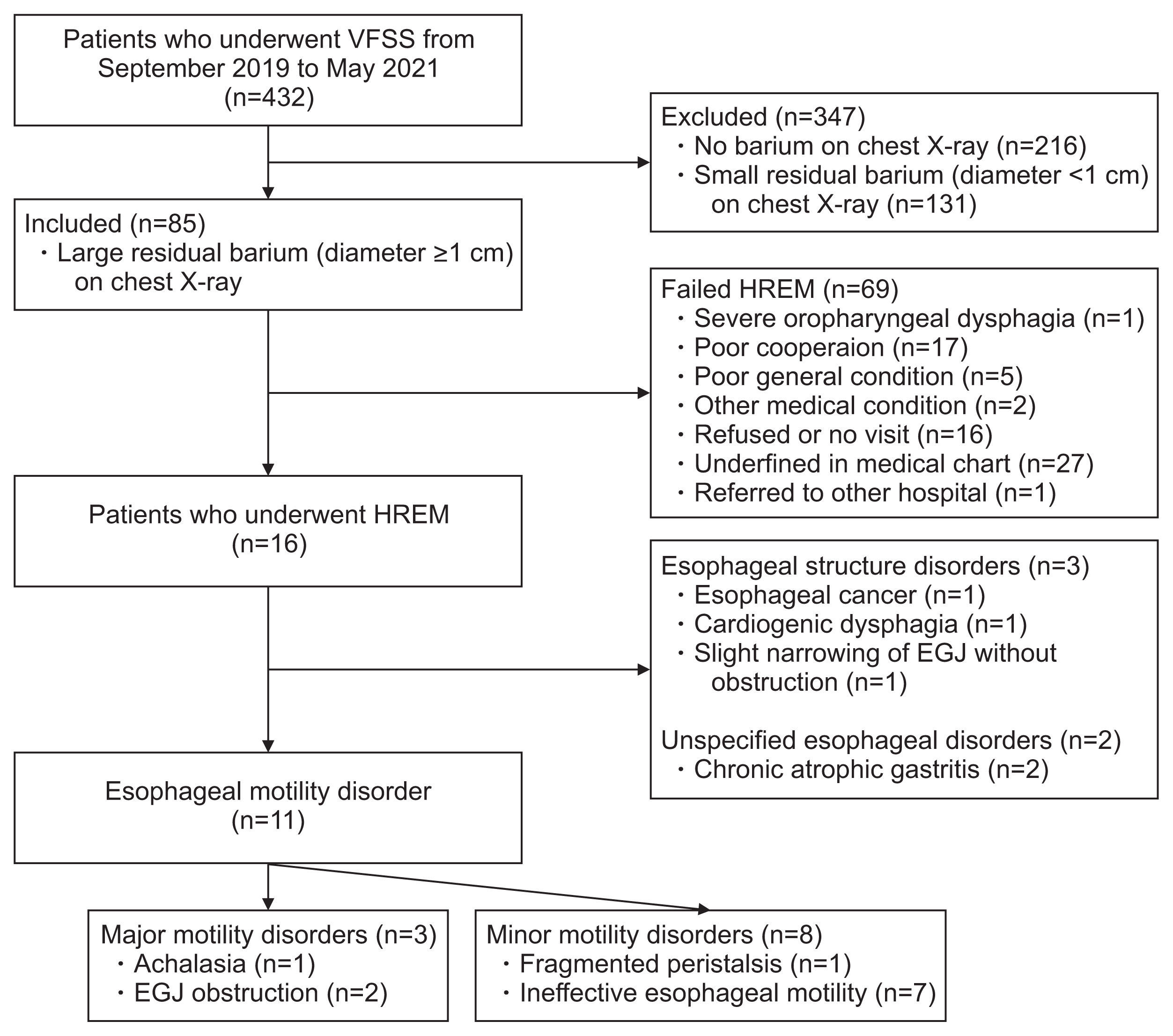
Methods
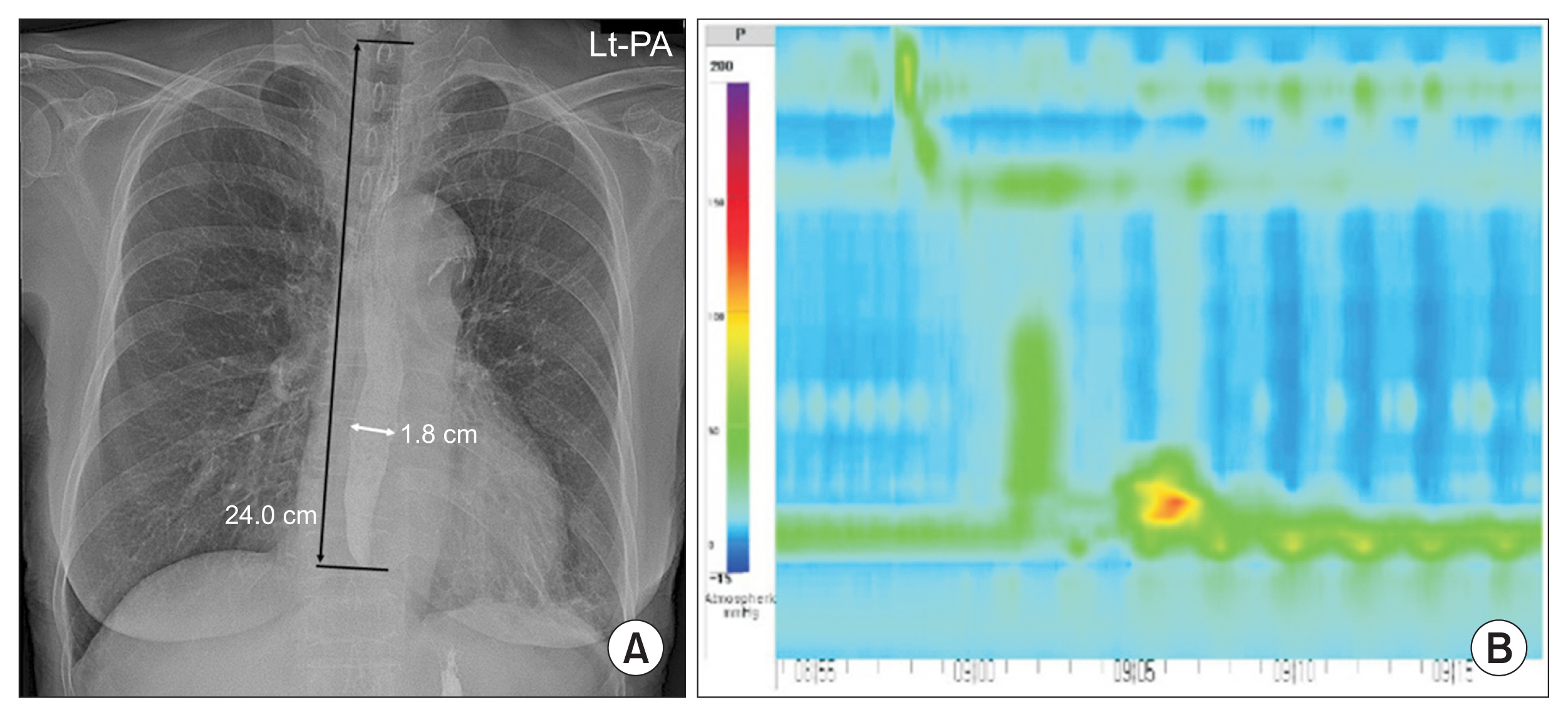
We reviewed the records of 432 patients who underwent VFSS from September 2019 to May 2021, and 85 patients (19.7%) with large residual barium (diameter ≥1 cm) were included. As a result of HREM, motility disorders were classified as major or minor motility disorders according. Esophagogastroduodenoscopy and chest computed tomography results available were also reviewed.
Results
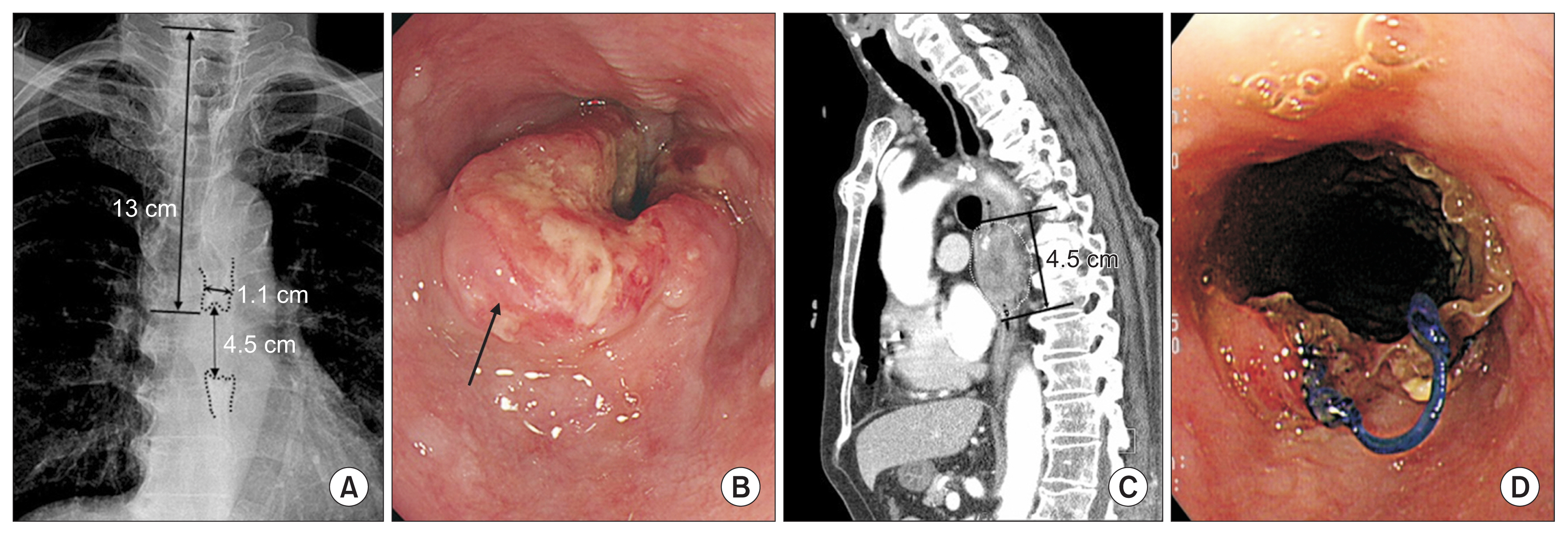
Among 85 patients with large residual barium in the esophagus, 16 patients (18.8%) underwent HREM. Abnormal esophageal motilities were identified in 68.8% patient: three patients (18.8%) had major motility disorders—achalasia (n=1), esophagogastric junction (EGJ) outflow obstruction (n=2)—and eight patients (50%) had minor motility disorders—ineffective esophageal motility (n=7), fragmented peristalsis (n=1). In those with normal esophageal motility, three patients of esophageal structure disorders (18.8%)—esophageal cancer (n=1), cardiogenic dysphagia (n=1), slight narrowing without obstruction of EGJ (n=1)—and two patients (12.5%) with chronic atrophic gastritis (n=2) were confirmed.
Conclusion
Esophageal motility disorders were identified in 68.8% of 16 patients with large esophageal residual barium with three patients in the major and eight patients in the minor categories. Residual barium in the esophagus was not rare and can be a sign of significant esophageal motility disorders.
Figure
Reference
-
1. Triadafilopoulos G, Hallstone A, Nelson-Abbott H, Bedinger K. Oropharyngeal and esophageal interrelationships in patients with nonobstructive dysphagia. Dig Dis Sci. 1992; 37:551–7.
Article2. Liu LW, Andrews CN, Armstrong D, Diamant N, Jaffer N, Lazarescu A, et al. Clinical practice guidelines for the assessment of uninvestigated esophageal dysphagia. J Can Assoc Gastroenterol. 2018; 1:5–19.
Article3. Cockeram AW. Canadian Association of Gastroenterology practice guidelines: evaluation of dysphagia. Can J Gastroenterol. 1998; 12:409–13.
Article4. Yoon SW, Kim KW, Park HJ, Kim EK, Yu JS, Seo JK, et al. The usefulness of esophagogram with marshmallow bolus in patients with esophageal-related symptoms. J Korean Radiol Soc. 1996; 34:399–404.
Article5. Smith DF, Ott DJ, Gelfand DW, Chen MY. Lower esophageal mucosal ring: correlation of referred symptoms with radiographic findings using a marshmallow bolus. AJR Am J Roentgenol. 1998; 171:1361–5.
Article6. Min YK, Baek S, Kang EK, Nam SJ. Characteristics of patients with esophageal dysphagia assessed by chest x-ray imaging after videofluoroscopic swallowing study. Ann Rehabil Med. 2020; 44:38–47.
Article7. Kahrilas PJ, Bredenoord AJ, Fox M, Gyawali CP, Roman S, Smout AJ, et al. The Chicago classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil. 2015; 27:160–74.
Article8. Blonski W, Kumar A, Feldman J, Richter JE. Timed barium swallow: diagnostic role and predictive value in untreated achalasia, esophagogastric junction outflow obstruction, and non-achalasia dysphagia. Am J Gastroenterol. 2018; 113:196–203.
Article9. Kostic S, Andersson M, Hellstrom M, Lonroth H, Lundell L. Timed barium esophagogram in the assessment of patients with achalasia: reproducibility and observer variation. Dis Esophagus. 2005; 18:96–103.
Article10. Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. 1996; 11:93–8.
Article11. Park J, Yoo W, Yoo B. Standard recipes for the preparation of thickened barium liquids used in the diagnosis of dysphagia. Clin Nutr Res. 2019; 8:265–71.
Article12. Richter JE, Wu WC, Johns DN, Blackwell JN, Nelson JL, Castell JA, et al. Esophageal manometry in 95 healthy adult volunteers: variability of pressures with age and frequency of “abnormal” contractions. Dig Dis Sci. 1987; 32:583–92.13. Varadarajulu S, Eloubeidi MA, Patel RS, Mulcahy HE, Barkun A, Jowell P, et al. The yield and the predictors of esophageal pathology when upper endoscopy is used for the initial evaluation of dysphagia. Gastrointest Endosc. 2005; 61:804–8.
Article14. Qureshi NA, Hallissey MT, Fielding JW. Outcome of index upper gastrointestinal endoscopy in patients presenting with dysphagia in a tertiary care hospital: a 10 years review. BMC Gastroenterol. 2007; 7:43.15. Spieker MR. Evaluating dysphagia. Am Fam Physician. 2000; 61:3639–48.16. Lin SH, Chang JY. Esophageal cancer: diagnosis and management. Chin J Cancer. 2010; 29:843–54.
Article17. Park J, Baek S, Kim G, Nam SJ, Cho BR. Dysphagia secondary to esophageal compression in a patient with decompensated heart failure. Korean J Helicobacter Up Gastrointest Res. 2022; 22:146–51.
Article18. Sweis R, Anggiansah A, Wong T, Kaufman E, Obrecht S, Fox M. Normative values and inter-observer agreement for liquid and solid bolus swallows in upright and supine positions as assessed by esophageal high-resolution manometry. Neurogastroenterol Motil. 2011; 23:509-e198.
Article19. Xiao Y, Nicodeme F, Kahrilas PJ, Roman S, Lin Z, Pandolfino JE. Optimizing the swallow protocol of clinical high-resolution esophageal manometry studies. Neurogastroenterol Motil. 2012; 24:e489–96.
Article20. Yadlapati R, Kahrilas PJ, Fox MR, Bredenoord AJ, Prakash Gyawali C, Roman S, et al. Esophageal motility disorders on high-resolution manometry: Chicago classification version 4.0. Neurogastroenterol Motil. 2021; 33:e14058.21. Shinjo Y, Okitsu A, Ukeda I, Miyagi A, Domen K, Koyama T. Effects of posture on subjective swallowing difficulty during screening tests for dysphagia. Int J Phys Med Rehabil. 2013; 1:133.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Esophageal Motility and Acid Clearance in Patients with Esophageal Varices
- How to Perform and Interpret Timed Barium Esophagogram
- Characteristics of Patients With Esophageal Dysphagia Assessed by Chest X-Ray Imaging After Videofluoroscopic Swallowing Study
- A Case of Tubular Duplication of the Esophagus
- Oropharyngeal Dysphagia in Esophageal Diseases