Ann Clin Neurophysiol.
2022;24(2):101-106. 10.14253/acn.2022.24.2.101.
Post-infectious basal ganglia encephalitis and axonal variant of Guillain-Barré syndrome after COVID-19 infection: an atypical case report
- Affiliations
-
- 1Department of Neurology, Gil Medical Center, Gachon University College of Medicine, Incheon, Korea
- KMID: 2535728
- DOI: http://doi.org/10.14253/acn.2022.24.2.101
Abstract
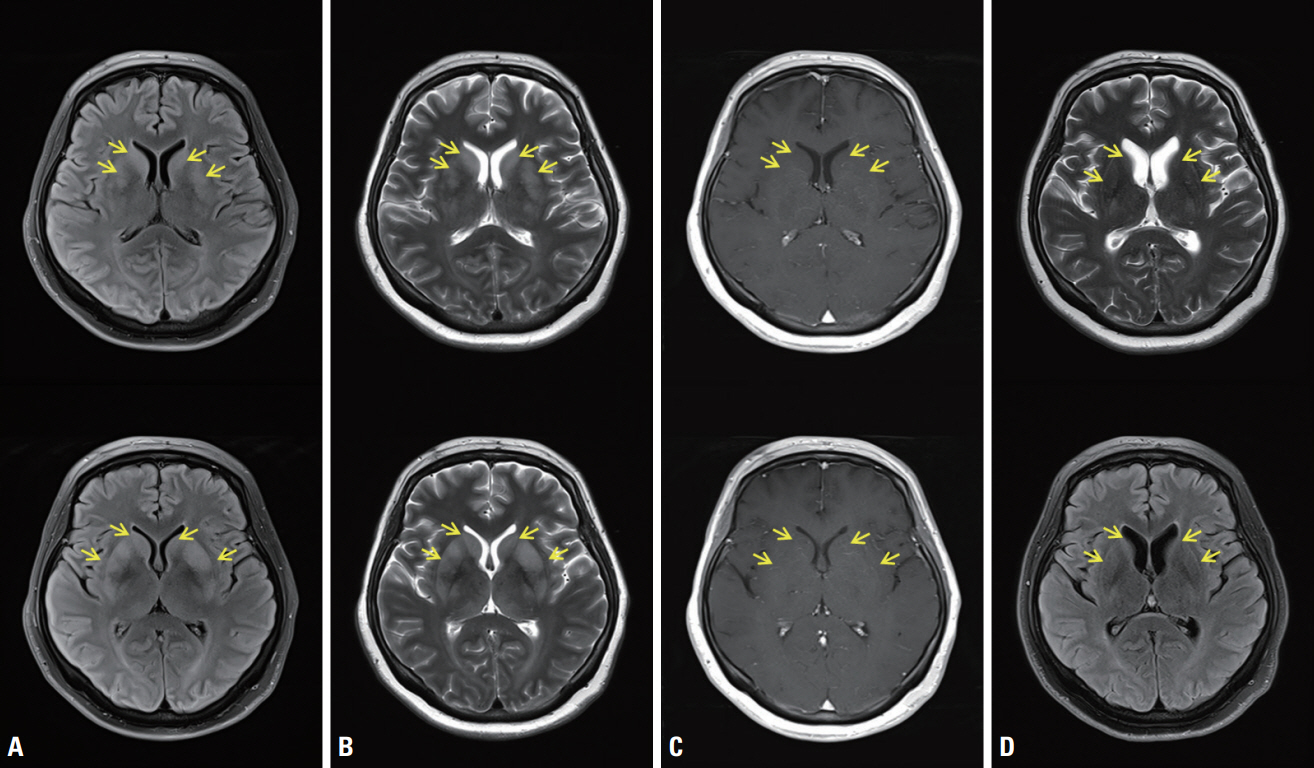
- Neurological complications attributed to coronavirus disease-19 (COVID-19) infection have been reported including acute disseminated encephalomyelitis, Guillain-Barré syndrome, and so on. Herein, we report a 49-year-old woman presented with acute encephalopathy and paraplegia simultaneously after COVID-19 infection. Brain magnetic resonance imaging (MRI) showed symmetric hyperintense basal ganglia lesions on T2-weighted imaging. Cerebrospinal fluid pleocytosis, motor axonal neuropathy and enhancement of conus medullaris nerve roots on spine MRI were observed. We treated her with high-dose corticosteroid and intravenous immunoglobulin.
Keyword
Figure
Reference
-
1. Ellul MA, Benjamin L, Singh B, Lant S, Michael BD, Easton A, et al. Neurological associations of COVID-19. Lancet Neurol. 2020; 19:767–783.2. Palaiodimou L, Stefanou MI, Katsanos AH, Fragkou PC, Papadopoulou M, Moschovos C, et al. Prevalence, clinical characteristics and outcomes of Guillain-Barré syndrome spectrum associated with COVID-19: a systematic review and meta-analysis. Eur J Neurol. 2021; 28:3517–3529.3. Siow I, Lee KS, Zhang JJY, Saffari SE, Ng A. Encephalitis as a neurological complication of COVID-19: a systematic review and meta-analysis of incidence, outcomes, and predictors. Eur J Neurol. 2021; 28:3491–3502.4. Bertrand A, Leclercq D, Martinez-Almoyna L, Girard N, Stahl JP, De-Broucker T. MR imaging of adult acute infectious encephalitis. Med Mal Infect. 2017; 47:195–205.5. Pohl D, Alper G, Van Haren K, Kornberg AJ, Lucchinetti CF, Tenembaum S, et al. Acute disseminated encephalomyelitis: updates on an inflammatory CNS syndrome. Neurology. 2016; 87(9 Suppl 2):S38–S45.6. Gulko E, Oleksk ML, Gomes W, Ali S, Mehta H, Overby P, et al. MRI brain findings in 126 patients with COVID-19: initial observations from a descriptive literature review. AJNR Am J Neuroradiol. 2020; 41:2199–2203.7. Van Cauter S, Severino M, Ammendola R, Van Berkel B, Vavro H, van den Hauwe L, et al. Bilateral lesions of the basal ganglia and thalami (central grey matter)-pictorial review. Neuroradiology. 2020; 62:1565–1605.8. Werner R, Lohr B, Lodemann P, Chemnitz JM, Woehrle JC. Autoimmune basal ganglia encephalitis with hemolytic anemia. Ann Hematol. 2022; 101:1857–1858.9. Pawela C, Brunsdon RK, Williams TA, Porter M, Dale RC, Mohammad SS. The neuropsychological profile of children with basal ganglia encephalitis: a case series. Dev Med Child Neurol. 2017; 59:445–448.10. Fokke C, van den Berg B, Drenthen J, Walgaard C, van Doorn PA, Jacobs BC. Diagnosis of Guillain-Barré syndrome and validation of Brighton criteria. Brain. 2014; 137(Pt 1):33–43.11. Wakerley BR, Yuki N. Mimics and chameleons in Guillain-Barré and Miller Fisher syndromes. Pract Neurol. 2015; 15:90–99.12. Yang J, Lee YB, Lee KW, Park HM. Atypical acute motor axonal neuropathy with cerebrospinal pleocytosis mimicking myelitis. J Clin Neurol. 2017; 13:205–206.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Correction of dosage of the drug: Post-infectious basal ganglia encephalitis and axonal variant of Guillain-Barré syndrome after COVID-19 infection: an atypical case report
- Finger Drop-Dominant Variant of Guillain-Barre Syndrome in a Patient With COVID-19: A Case Report
- Guillain-Barre Syndrome in a Patient with Chemotherapy for HIV Related Burkitt's Lymphoma
- An Unusual Case of Pure Motor Variant of Guillain-Barre Syndrome Initially Presenting with Hemiparesis
- Guillain-Barré Syndrome with Atypical Clinical Course after BNT162b2 COVID-19 Vaccination