Korean J Women Health Nurs.
2022 Sep;28(3):222-234. 10.4069/kjwhn.2022.08.22.
Comparison of health behaviors of adult women in Korea before and during the COVID-19 pandemic: secondary analysis of the Korea National Health and Nutrition Examination Survey 2019–2020
- Affiliations
-
- 1Department of Nursing, Hannam University, Daejeon, Korea
- 2Department of Nursing, Joongbu University, Geumsan, Korea
- KMID: 2535439
- DOI: http://doi.org/10.4069/kjwhn.2022.08.22
Abstract
- Purpose
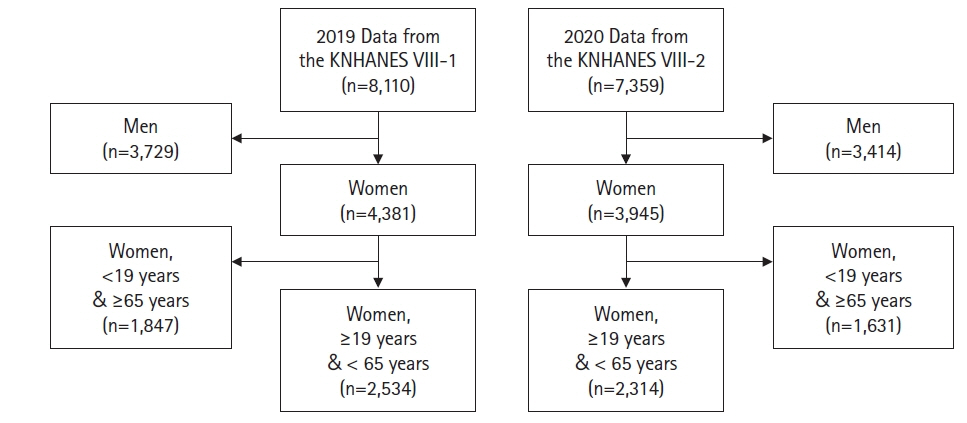
This study investigated the changes in the health-related behaviors of adult women in Korea during the coronavirus disease 2019 (COVID-19) pandemic. Methods: Data from the eighth Korea National Health and Nutrition Examination Survey (2019- 2020) were analyzed. The participants were 4,848 women aged 19 to 64 years in 2019 and 2020. Data analysis using the complex sampling design was performed using SPSS 20.1. Results: Positive changes during the pandemic compared to before the pandemic in Korean adult women were found for improved subjective oral health perceptions (odds ratio [OR], 1.77; p<.001), increased moderate-intensity exercise in work and leisure activities (OR, 1.75; p<.001 and OR; 1.29, p=.004), and a decrease in secondhand smoke exposure at the workplace and in public places (OR, 0.64; p=.004 and OR, 0.60; p<.001). However, the following negative health behavior changes were found: decreased frequency of walking 5 days a week (OR, 0.81; p=.011) and an increase in unhealthy daytime sleep durations (OR, 1.40; p=006). Conclusion: Compared to before the COVID-19 pandemic, Korean adult women perceived their subjective dental health more positively during the COVID-19 pandemic, decreased their exposure to secondhand smoke at work and in public places, decreased walking, and increased sleep duration during the week. Since this study only compared data between 1 year before and after the start of the pandemic, it is necessary to investigate a longer period of time in the future. A future study should attempt to identify the factors related to changes in health behaviors caused by the pandemic.
Keyword
Figure
Reference
-
References
1. Reizer A, Koslowsky M, Geffen L. Living in fear: The relationship between fear of COVID-19, distress, health, and marital satisfaction among Israeli women. Health Care Women Int. 2020; 41(11-12):1273–1293. https://doi.org/10.1080/07399332.2020.1829626.
Article2. Centers for Disease Control and Prevention. COVID Data Tracker [Internet]. Atlanta: Author; 2022 [cited 2022 Jul 2]. Available from: https://covid.cdc.gov/covid-data-tracker/#datatracker-home.3. Choi JY. COVID-19 in South Korea. Postgrad Med J. 2020; 96(1137):399–402. https://doi.org/10.1136/postgradmedj-2020-137738.
Article4. Park JH. Jang JE, Choi YH. The impact of the COVID-19 pandemic on oral health behavior and oral symptoms in young adults. J Korean Acad Oral Health. 2021; 45(4):192–197. https://doi.org/10.11149/jkaoh.2021.45.4.192.
Article5. Mathieu E, Ritchie H, Ortiz-Ospina E, Roser M, Hasell J, Appel C, et al. A global database of COVID-19 vaccinations. Nat Hum Behav. 2021; 5(7):947–953. https://doi.org/10.1038/s41562-021-01122-8.
Article6. Proto E, Quintana-Domeque C. COVID-19 and mental health deterioration by ethnicity and gender in the UK. PLoS One. 2021; 16(1):e0244419. https://doi.org/10.1371/journal.pone.0244419.
Article7. Oberndorfer M, Dorner TE, Brunnmayr M, Berger K, Dugandzic B, Bach M. Health-related and socio-economic burden of the COVID-19 pandemic in Vienna. Health Soc Care Community. 2022; 30(4):1550–1561. https://doi.org/10.1111/hsc.13485.
Article8. Pant S, Subedi M. Impact of COVID-19 on the elderly. JPAHS. 2020; 7(2):32–38. https://doi.org/10.3126/jpahs.v7i2.31104.
Article9. Bambra C, Albani V, Franklin P. COVID-19 and the gender health paradox. Scand J Public Health. 2021; 49(1):17–26. https://doi.org/10.1177/1403494820975604.
Article10. Pereira MD. Researching gender inequalities in academic labor during the COVID-19 pandemic: avoiding common problems and asking different questions. Gend Work Organ. 2021; 28(Suppl 2):498–509. https://doi.org/10.1111/gwao.12618.
Article11. Allen S, Julian Z, Coyne-Beasley T, Erwin PC, Fletcher FE. COVID-19’s impact on women: a stakeholder-engagement approach to increase public awareness through virtual town halls. J Public Health Manag Pract. 2020; 26(6):534–538. https://doi.org/10.1097/PHH.0000000000001249.
Article12. Llop-Gironés A, Vračar A, Llop-Gironés G, Benach J, Angeli-Silva L, Jaimez L, et al. Employment and working conditions of nurses: where and how health inequalities have increased during the COVID-19 pandemic? Hum Resour Health. 20. 2116; 19(1):112. https://doi.org/10.1186/s12960-021-00651-7.
Article13. Auzan AA. The economy under the pandemic and afterwards. Popul Econ. 2020; 4(2):4–12. https://doi.org/10.3897/popecon.4.e53403.
Article14. Coman C, Țîru LG, Meseșan-Schmitz L, Stanciu C, Bularca MC. Online teaching and learning in higher education during the coronavirus pandemic: students’ perspective. Sustainability. 2020; 12(24):10367. https://doi.org/10.3390/su122410367.
Article15. Khlystova O, Kalyuzhnova Y, Belitski M. The impact of the COVID-19 pandemic on the creative industries: a literature review and future research agenda. J Bus Res. 2022; 139:1192–1210. https://doi.org/10.1016/j.jbusres.2021.09.062.
Article16. Prowse R, Sherratt F, Abizaid A, Gabrys RL, Hellemans KG, Patterson ZR, et al. Coping with the COVID-19 pandemic: examining gender differences in stress and mental health among university students. Front Psychiatry. 2021; 12:650759. https://doi.org/10.3389/fpsyt.2021.650759.
Article17. Varma P, Junge M, Meaklim H, Jackson ML. Younger people are more vulnerable to stress, anxiety and depression during COVID-19 pandemic: a global cross-sectional survey. Prog Neuropsychopharmacol Biol Psychiatry. 2021; 109:110236. https://doi.org/10.1016/j.pnpbp.2020.110236.
Article18. Lee JH, Kim BS. Relationship between the objective oral health status and the subjective oral health awareness of Korean adults. AJMAHS. 2015; 5(3):119–130. http://doi.org/10.35873/ajmahs.2015.5.3.013.
Article19. Choi MJ, Kim SY, Choi SJ. The relationship between secondhand smoke exposure and mental health of adult female non-smokers in Korea: based on the Korea National Health and Nutrition Examination Survey 2019. Korean J Health Serv Manag. 2021; 15(5):105–115. https://doi.org/10.12811/kshsm.2021.15.3.105.
Article20. World Health Organization. #HealthyAtHom-physical activity [Internet]. Geneva; Author: 2022 [cited 2022 Mar 1]. Available from: https://www.who.int/news-room/campaigns/connecting-the-world-to-combat-coronavirus/healthyathome/healthyathome---physical-activity.21. Korea Society for the Study of Obesity. Quick reference guideline 2020 [Internet]. Seoul: Author; 2022 [cited 2022 Jun 1]. Available from: http://general.kosso.or.kr/html/?pmode=BBBS0001300003&page=1&smode=view&seq=1375&searchValue=&searchTitle=strTitle.22. World Health Organization. WHO guidelines on physical activity and sedentary behavior [Internet]. Geneva; Author: 2020 [cited 2020 Apr 20]. Available from: https://apps.who.int/iris/bitstream/handle/10665/336656/9789240015128-eng.pdf?sequence=1&isAllowed=y.23. Ekelund U, Tarp J, Steene-Johannessen J, Hansen BH, Jefferis B, Fagerland MW, et al. Dose-response associations between accelerometry measured physical activity and sedentary time and all cause mortality: systematic review and harmonised meta-analysis. BMJ. 2019; 366:14570. https://doi.org/10.1136/bmj.l4570.
Article24. Lima MG, Barros MB, Ceolim MF, Zancanella E, Cardoso TAMO. Sleep duration, health status, and subjective well-being: a population-based study. Rev Saude Publica. 2018; 52:82. https://doi.org/10.11606/S1518-8787.2018052000602.
Article25. Kim MJ, Lim CY. Correlation of self-perceived oral health status and objective oral health status of adults. J Korea Acad-Industr Coop Soc. 2017; 18(5):375–381. https://doi.org/10.5762/KAIS.2017.18.5.375.
Article26. Chu DK, Akl EA, Duda S, Solo K, Yaacoub S, Schünemann HJ, et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. 2020; 395(10242):1973–1987. https://doi.org/10.1016/S0140-6736(20)31142-9.
Article27. Jin S, Han KM, Nam M, Chang J. Association between secondhand smoke exposure and depressive symptoms among Korean adults. Korean J Biol Psychiatry. 2020; 27(2):101–111. https://doi.org/10.22857/kjbp.2020.27.2.008.
Article28. Lee J, Kwon M. Health behavior changes in Korean adolescents before and during the COVID-19 pandemic: secondary data analysis of the 2019-2020 Youth Health Risk Behavior web-based survey. J Korean Soc Sch Health. 2021; 34(3):179–189. https://doi.org/10.15434/kssh.2021.34.3.179.
Article29. Kim MS, Kim YH. A study on the assertive behavior among non-smoking college students under secondhand smoke exposure. J Korea Acad-Industr Coop Soc. 2012; 13(11):5187–5195. https://doi.org/10.5762/KAIS.2012.13.11.5187.
Article30. Kim SS. The urine cotinine level and periodontal disease among environmental tobacco smoke exposure on convergence study. J Korean Converg Soc. 2018; 9(12):295–299. https://doi.org/10.15207/JKCS.2018.9.12.295.
Article31. Oberg M, Jaakkola MS, Woodward A, Peruga A, Prüss-Ustün A. Worldwide burden of disease from exposure to second-hand smoke: a retrospective analysis of data from 192 countries. Lancet. 2011; 377(9760):139–146. https://doi.org/10.1016/S0140-6736(10)61388-8.
Article32. Guak S, Lee K, Kim S, Kim S, Yang W, Ha K. Impact of the smoke-free law on secondhand smoke in computer game rooms. J Environ Health Sci. 2015; 41(1):11–16. https://doi.org/10.5668/JEHS.2015.41.1.11.
Article33. Kashyap VK, Dhasmana A, Massey A, Kotnala S, Zafar N, Jaggi M, et al. Smoking and COVID-19: adding fuel to the flame. Int J Mol Sci. 2020; 21(18):6581. https://doi.org/10.3390/ijms21186581.
Article34. Castañeda-Babarro A, Arbillaga-Etxarri A, Gutiérrez-Santamaría B, Coca A. Physical activity change during COVID-19 confinement. Int J Environ Res Public Health. 2020; 17(18):6878. https://doi.org/10.3390/ijerph17186878.
Article35. Lee SY. In the era of COVID-19, 8 out of 10 people have done ‘home training’. Yunhap news. 2020 Apr 24.36. Hall G, Laddu DR, Phillips SA, Lavie CJ, Arena R. A tale of two pandemics: how will COVID-19 and global trends in physical inactivity and sedentary behavior affect one another? Prog Cardiovasc Dis. 2021; 64:108–110. https://doi.org/10.1016/j.pcad.2020.04.005.
Article37. Sallis JF, Adlakha D, Oyeyemi A, Salvo D. An international physical activity and public health research agenda to inform coronavirus disease-2019 policies and practices. J Sport Health Sci. 2020; 9(4):328–334. https://doi.org/10.1016/j.jshs.2020.05.005.
Article38. Farah BQ, do Prado WL, Malik N, Lofrano-Prado MC, de Melo PH, Botero JP, et al. Barriers to physical activity during the COVID-19 pandemic in adults: a cross-sectional study. Sport Sci Health. 2021; 17(2):441–447. https://doi.org/10.1007/s11332-020-00724-5.
Article39. Dwyer MJ, Pasini M, De Dominicis S, Righi E. Physical activity: benefits and challenges during the COVID-19 pandemic. Scand J Med Sci Sports. 2020; 30(7):1291–1294. https://doi.org/10.1111/sms.13710.
Article40. Suh DH, Nam SM, Um HS, Kim MJ. Physical activity and psychological state of adolescents experiencing the spread of coronavirus disease 19 (COVID-19). Korean J Growth Develop. 2022; 30(2):207–218. https://doi.org/10.34284/kjgd.2022.05.30.2.207.
Article41. Cellini N, Canale N, Mioni G, Costa S. Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J Sleep Res. 2020; 29(4):e13074. https://doi.org/10.1111/jsr.13074.
Article42. Gao C, Scullin MK. Sleep health early in the coronavirus disease 2019 (COVID-19) outbreak in the United States: integrating longitudinal, cross-sectional, and retrospective recall data. Sleep Med. 2020; 73:1–10. https://doi.org/10.1016/j.sleep.2020.06.032.
Article43. Kim OJ. Effects of physical activity levels on subjective health・body type recognition and mental health status・sleep fatigue recovery for Korean adolescents: evidence from before and after COVID-19. J Converg Sports Exerc Sci. 2022; 20(1):29–40. https://doi.org/10.22997/jcses.2022.20.1.29.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Changes in the management of hypertension, diabetes mellitus, and hypercholesterolemia in Korean adults before and during the COVID-19 pandemic: data from the 2010-2020 Korea National Health and Nutrition Examination Survey
- Changes in food and nutrient intakes in Korean adults before and during the COVID-19 pandemic: data from the 2011-2020 Korea National Health and Nutrition Examination Survey
- Mental health of Korean adults before and during the COVID-19 pandemic: a special report of the 2020 Korea National Health and Nutrition Examination Survey
- Obesity, hypertension, diabetes mellitus, and hypercholesterolemia in Korean adults before and during the COVID-19 pandemic: a special report of the 2020 Korea National Health and Nutrition Examination Survey
- Changes in eating behaviors according to household income in adolescents during the COVID-19 pandemic: findings from the Korea National Health and Nutrition Examination Survey