Anesth Pain Med.
2022 Oct;17(4):361-370. 10.17085/apm.22237.
Percutaneous epidural balloon neuroplasty: a narrative review of current evidence
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2535334
- DOI: http://doi.org/10.17085/apm.22237
Abstract
- Percutaneous epidural balloon neuroplasty (PEBN) can be used to perform balloon decompression combined with percutaneous epidural neuroplasty (PEN), leading to significant pain relief and functional improvement in patients with lumbar spinal stenosis. Several studies have demonstrated the effectiveness of PEBN and supported its relatively long-term outcomes (at least 6 months, sustained for up to 12 months). Balloon neuroplasty appears to be superior to conventional PEN. Moreover, it has been shown to be effective in patients unresponsive to conventional PEN or in those with post lumbar surgery syndrome. In addition, balloon neuroplasty achieved successful outcomes regardless of the approach used, such as retrodiscal, transforaminal, contralateral interlaminar, or caudal. Chronic lumbar radicular pain without back pain, neurogenic claudication, and minimal neuropathic component were favorable predictors of successful PEBN from a symptomatic perspective. A short duration of pain after lumbar surgery, lumbar foraminal stenosis caused primarily by degenerative disc, mild foraminal stenosis, and perineural adhesion by degenerative discs were associated with successful outcomes of PEBN from pathological aspects. Ballooning ≥ 50% of the target sites and complete contrast dispersion after ballooning seemed to be crucial for successful outcomes from a technical perspective. In addition, PEBN was effective regardless of the accompanying redundant nerve roots or a mild degree of spondylolisthesis. Studies on balloon neuroplasty have reported occasional minor and self-limiting complications; however, no PEBN-related significant complications have been reported. Given the present evidence, balloon neuroplasty appears to be a safe and effective procedure with minimal complications for the treatment of lumbar spinal stenosis.
Keyword
Figure
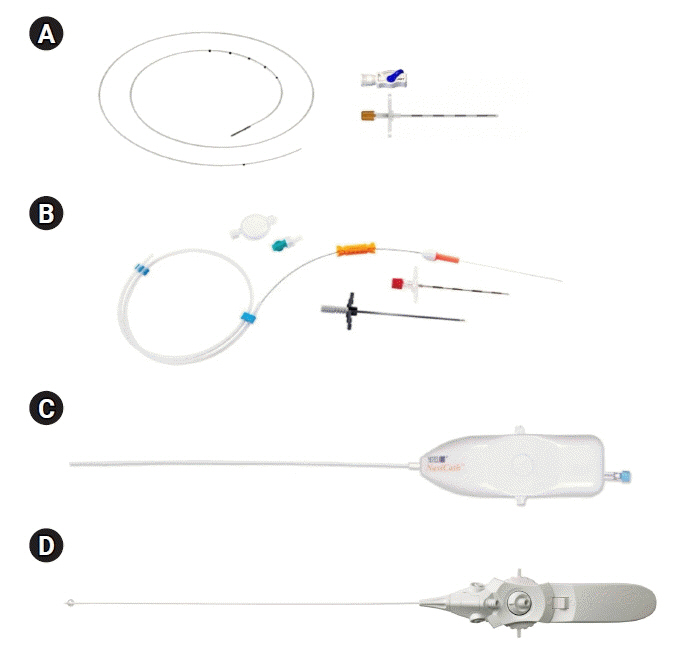
Reference
-
1. Helm S, Knezevic NN. A review of the role of epidural percutaneous neuroplasty. Pain Manag. 2019; 9:53–62.
Article2. Racz GB, Heavner JE, Noe CE, Al-Kaisy A, Matsumoto T, Lee SC, et al. Epidural lysis of adhesions and percutaneous neuroplasty. In: Techniques of neurolysis. Edited by Racz G, Noe C: Cham, Springer. 2016, pp 119-43.3. Bosscher HA, Heavner JE, Grozdanov P, Warraich IA, Wachtel MS, Dertien J. The peridural membrane of the human spine is well innervated. Anat Rec (Hoboken). 2016; 299:484–91.
Article4. Bosscher HA, Heavner JE. Treatment of common low back pain: a new approach to an old problem. Pain Pract. 2015; 15:509–17.
Article5. Yıldırım HU, Akbas M. Percutaneous and endoscopic adhesiolysis. Agri. 2021; 33:129–41.
Article6. Helm S 2nd, Racz GB, Gerdesmeyer L, Justiz R, Hayek SM, Kaplan ED, et al. Percutaneous and endoscopic adhesiolysis in managing low back and lower extremity pain: a systematic review and meta-analysis. Pain Physician. 2016; 19:E245–82.7. Manchikanti L, Boswell MV, Datta S, Fellows B, Abdi S, Singh V, et al. Comprehensive review of therapeutic interventions in managing chronic spinal pain. Pain Physician. 2009; 12:E123–98.8. Racz GB, Haynsworth RF, Lipton S. Experiences with an improved epidural catheter. Pain Clin. 1986; 1:21–7.9. Racz GB, Sabonghy M, Gintautas J, Kline WM. Intractable pain therapy using a new epidural catheter. JAMA. 1982; 248:579–81.
Article10. Kim SH, Choi SS. Epidural neuroplasty/epidural adhesiolysis. Anesth Pain Med. 2016; 11:14–22.
Article11. Lee JH, Lee SH. Clinical effectiveness of percutaneous adhesiolysis and predictive factors of treatment efficacy in patients with lumbosacral spinal stenosis. Pain Med. 2013; 14:1497–504.
Article12. Choi SS, Joo EY, Hwang BS, Lee JH, Lee G, Suh JH, et al. A novel balloon-inflatable catheter for percutaneous epidural adhesiolysis and decompression. Korean J Pain. 2014; 27:178–85.
Article13. Kim HJ, Rim BC, Lim JW, Park NK, Kang TW, Sohn MK, et al. Efficacy of epidural neuroplasty versus transforaminal epidural steroid injection for the radiating pain caused by a herniated lumbar disc. Ann Rehabil Med. 2013; 37:824–31.
Article14. Manchikanti L, Abdi S, Atluri S, Benyamin RM, Boswell MV, Buenaventura RM, et al. An update of comprehensive evidence-based guidelines for interventional techniques in chronic spinal pain. Part II: guidance and recommendations. Pain Physician. 2013; 16(2 Suppl):S49–283.15. Choi SS, Lee JH, Kim D, Kim HK, Lee S, Song KJ, et al. Effectiveness and factors associated with epidural decompression and adhesiolysis using a balloon-inflatable catheter in chronic lumbar spinal stenosis: 1-year follow-up. Pain Med. 2016; 17:476–87.
Article16. Kim SH, Koh WU, Park SJ, Choi WJ, Suh JH, Leem JG, et al. Clinical experiences of transforaminal balloon decompression for patients with spinal stenosis. Korean J Pain. 2012; 25:55–9.
Article17. Kim SH, Choi WJ, Suh JH, Jeon SR, Hwang CJ, Koh WU, et al. Effects of transforaminal balloon treatment in patients with lumbar foraminal stenosis: a randomized, controlled, double-blind trial. Pain Physician. 2013; 16:213–24.18. Kim DH, Ji GY, Kwon HJ, Na T, Shin JW, Shin DA, et al. Contrast dispersion on epidurography may be associated with clinical outcomes after percutaneous epidural neuroplasty using an inflatable balloon catheter. Pain Med. 2020; 21:677–85.
Article19. Karm MH, Yoon SH, Seo DK, Lee S, Lee Y, Cho SS, et al. Combined epidural adhesiolysis and balloon decompression can be effective in intractable lumbar spinal stenosis patients unresponsive to previous epidural adhesiolysis. Medicine (Baltimore). 2019; 98:e15114.
Article20. Song SO, Lim HJ. Clinical experience of epidural adhesiolysis in patients with failed back surgery syndrome. Korean J Anesthesiol. 2004; 47:547–52.
Article21. Park JY, Ji GY, Lee SW, Park JK, Ha D, Park Y, et al. Relationship of success rate for balloon adhesiolysis with clinical outcomes in chronic intractable lumbar radicular pain: a multicenter prospective study. J Clin Med. 2019; 8:606.
Article22. Karm MH, Choi SS, Kim DH, Park JY, Lee S, Park JK, et al. Percutaneous epidural adhesiolysis using inflatable balloon catheter and balloon-less catheter in central lumbar spinal stenosis with neurogenic claudication: a randomized controlled trial. Pain Physician. 2018; 21:593–606.23. Oh Y, Shin DA, Kim DJ, Cho W, Na T, Leem JG, et al. Effectiveness of and factors associated with balloon adhesiolysis in patients with lumbar post-laminectomy syndrome: a retrospective study. J Clin Med. 2020; 9:1144.
Article24. Seo DK, Lee S, Lee G, Lee MS, Yoon SH, Choi SS, et al. Retrodiscal epidural balloon adhesiolysis through Kambin's triangle in chronic lumbar spinal stenosis: a retrospective analysis and technical considerations. Medicine (Baltimore). 2018; 97:e12791.25. Gil HY, Jeong S, Cho H, Choi E, Nahm FS, Lee PB. Kambin's triangle approach versus traditional safe triangle approach for percutaneous transforaminal epidural adhesiolysis using an inflatable balloon catheter: a pilot study. J Clin Med. 2019; 8:1996.
Article26. Kim CS, Moon YJ, Kim JW, Hyun DM, Son SL, Shin JW, et al. Transforaminal epidural balloon adhesiolysis via a contralateral interlaminar retrograde foraminal approach: a retrospective analysis and technical considerations. J Clin Med. 2020; 9:981.
Article27. Hsu E, Atanelov L, Plunkett AR, Chai N, Chen Y, Cohen SP. Epidural lysis of adhesions for failed back surgery and spinal stenosis: factors associated with treatment outcome. Anesth Analg. 2014; 118:215–24.28. Lee S, Lee JW, Yeom JS, Kim KJ, Kim HJ, Chung SK, et al. A practical MRI grading system for lumbar foraminal stenosis. AJR Am J Roentgenol. 2010; 194:1095–8.
Article29. Kim DH, Cho SS, Moon YJ, Kwon K, Lee K, Leem JG, et al. Factors associated with successful responses to transforaminal balloon adhesiolysis for chronic lumbar foraminal stenosis: retrospective study. Pain Physician. 2017; 20:E841–8.30. Oh Y, Kim DH, Park JY, Ji GY, Shin DA, Lee SW, et al. Factors associated with successful response to balloon decompressive adhesiolysis neuroplasty in patients with chronic lumbar foraminal stenosis. J Clin Med. 2019; 8:1766.
Article31. Sim JH, Sim KC, Kim Y, Kim DH, Lee I, Shin JW, et al. Effectiveness of epidural balloon neuroplasty in patients with chronic spinal stenosis accompanied by redundant nerve roots: a longitudinal cohort study. Pain Physician. 2022; 25:E841–50.32. Karm MH, Kim CS, Kim DH, Lee D, Kim Y, Shin JW, et al. Effectiveness of percutaneous epidural neuroplasty using balloon catheter in patients with chronic spinal stenosis accompanying mild spondylolisthesis: a longitudinal cohort study. Korean J Pain. Forthcoming 2022.33. Lee F, Jamison DE, Hurley RW, Cohen SP. Epidural lysis of adhesions. Korean J Pain. 2014; 27:3–15.
Article34. Manchikanti L, Malla Y, Wargo BW, Cash KA, Pampati V, Fellows B. A prospective evaluation of complications of 10,000 fluoroscopically directed epidural injections. Pain Physician. 2012; 15:131–40.35. Talu GK, Erdine S. Complications of epidural neuroplasty: a retrospective evaluation. Neuromodulation. 2003; 6:237–47.
Article36. Fishchenko I, Piontkovskyi V, Zlativ V. Complications of epidural adhesiolysis. J Educ Health Sport. 2016; 6:183–9.37. Kim JY, Lee YH, Yoo S, Kim JY, Joo M, Park HJ. Factors predicting the success of adhesiolysis using a steerable catheter in lumbar failed back surgery syndrome: a retrospective study. J Clin Med. 2021; 10:913.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Unintended Complication of Intracranial Subdural Hematoma after Percutaneous Epidural Neuroplasty
- Cerebellar Infarction Following Epidural Abscess after Epidural Neuroplasty
- Effectiveness of percutaneous epidural neuroplasty using a balloon catheter in patients with chronic spinal stenosis accompanying mild spondylolisthesis: a longitudinal cohort study
- Percutaneous Epidural Neuroplasty
- Massive Epidural Hematoma Caused by Percutaneous Epidural Neuroplasty: A Case Report