Anesth Pain Med.
2022 Jul;17(3):320-326. 10.17085/apm.22139.
Comparison of postoperative back pain between paramedian and midline approach for thoracic epidural anesthesia
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Keimyung University Dongsan Hospital, Daegu, Korea
- KMID: 2535326
- DOI: http://doi.org/10.17085/apm.22139
Abstract
- Background
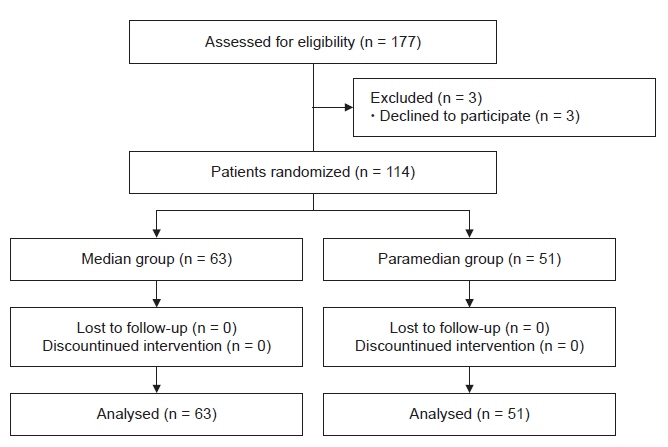
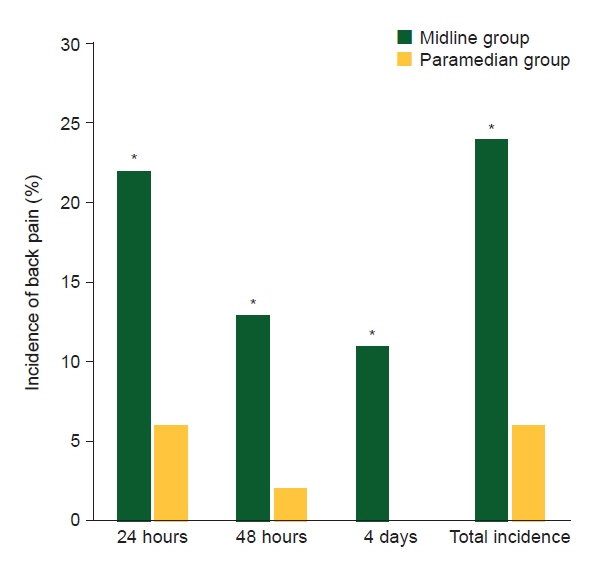
The development of back pain following epidural analgesia is one reason for patient refusal of neuraxial analgesia. The primary endpoint of this study was to compare the incidence and severity of back pain following midline and paramedian epidural technique. The secondary endpoint was to identify the risk factors associated with the occurrence of back pain. Methods: This prospective randomized study included 114 patients receiving thoracic epidural catheterization for pain management following upper abdominal or thoracic surgery. Patients were allocated to either the midline or the paramedian group by computer-generated randomization. An investigator who was blinded to the patient group interviewed patients at 24, and 48 h, and 3–5 days after surgery about the existence of back pain and its severity. Results: The total incidence of back pain following epidural anesthesia was 23.8% in the midline group and 7.8% in the paramedian group. The numerical rating scale of back pain was not different between the two groups at 24 h and 4 days after surgery. The paramdian technique was associated with a lower incidence of back pain than the midline technique (95% confidence interval 0.05–0.74, odds ratio 0.2, P < 0.01). However, the number of attempts, surgical position, body mass index, and duration of surgery were not associated with back pain. Conclusions: This study showed that the midline group of thoracic epidural analgesia demonstrated higher incidence of back pain than the paramedian group. However, the pain was mild in intensity and decreased with time in both groups.
Keyword
Figure
Reference
-
1. Benzon HT, Asher YG, Hartrick CT. Back pain and neuraxial anesthesia. Anesth Analg. 2016; 122:2047–58.
Article2. Lee JH, Yoon DH, Heo BH. Incidence of newly developed postoperative low back pain with median versus paramedian approach for spinal anesthesia. Korean J Anesthesiol. 2020; 73:518–24.
Article3. Bailey JG, Morgan CW, Christie R, Ke JXC, Kwofie MK, Uppal V. Continuous peripheral nerve blocks compared to thoracic epidurals or multimodal analgesia for midline laparotomy: a systematic review and meta-analysis. Korean J Anesthesiol. 2021; 74:394–408.
Article4. Yi JW, Choi SE, Chung JY. Laparoscopic cholecystectomy performed under regional anesthesia in patient who had undergone pneumonectomy: a case report. Korean J Anesthesiol. 2009; 56:330–3.
Article5. Tekgül ZT, Pektaş S, Turan M, Karaman Y, Çakmak M, Gönüllü M. Acute back pain following surgery under spinal anesthesia. Pain Pract. 2015; 15:706–11.
Article6. Hakim SM, Narouze S, Shaker NN, Mahran MA. Risk factors for new-onset persistent low-back pain following nonobstetric surgery performed with epidural anesthesia. Reg Anesth Pain Med. 2012; 37:175–82.
Article7. Chan ST. Incidence of back pain after lumbar epidural anaesthesia for non-obstetric surgery--a preliminary report. Med J Malaysia. 1995; 50:241–5.8. Rabinowitz A, Bourdet B, Minville V, Chassery C, Pianezza A, Colombani A, et al. The paramedian technique: a superior initial approach to continuous spinal anesthesia in the elderly. Anesth Analg. 2007; 105:1855–7.
Article9. Singh B, Sohal AS, Singh I, Goyal S, Kaur P, Attri JP. Incidence of postspinal headache and low backache following the median and paramedian approaches in spinal anesthesia. Anesth Essays Res. 2018; 12:186–9.
Article10. Kopp SL, Peters SM, Rose PS, Hebl JR, Horlocker TT. Worsening of neurologic symptoms after spinal anesthesia in two patients with spinal stenosis. Reg Anesth Pain Med. 2015; 40:502–5.
Article11. Trindle MR, McKay WR. Dorsal primary ramus nerve block for treatment of low back pain after epidural analgesia. Anesth Analg. 1992; 75:1038–40.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Difference of Success Rate between the Midline Approach and the Paramedian Approach of Spinal Anesthesia in each of Flexed Patients and Straightened Patients
- Comparison of Depth of Puncture Needle and Difficulty of Puncture in Spinal Anesthesia by Midline or Paramedian Approach in Korean Adults
- Predicting Factors for the Distance from Skin to the Epidural Space with the Paramedian Epidural Approach
- Incidence of newly developed postoperative low back pain with median versus paramedian approach for spinal anesthesia
- Accidental intrapleural positioning of an epidural catheter in a patient undergoing a right pneumonectomy: A case report