J Korean Med Sci.
2022 Nov;37(44):e317. 10.3346/jkms.2022.37.e317.
National Surveillance of Pediatric Outof-Hospital Cardiac Arrest in Korea: The 10-Year Trend From 2009 to 2018
- Affiliations
-
- 1Department of Emergency Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Department of Digital Health, Samsung Advanced Institute for Health Science & Technology (SAIHST), Sungkyunkwan University, Seoul, Korea
- 3Digital and Smart Health Office, Tan Tock Seng Hospital (TTSH), Singapore
- 4Health Information and Strategy Center, Samsung Medical Center, Seoul, Korea
- KMID: 2535181
- DOI: http://doi.org/10.3346/jkms.2022.37.e317
Abstract
- Background
This study reports trends in pediatric out-of-hospital cardiac arrest (OHCA) and factors affecting clinical outcomes by age group.
Methods
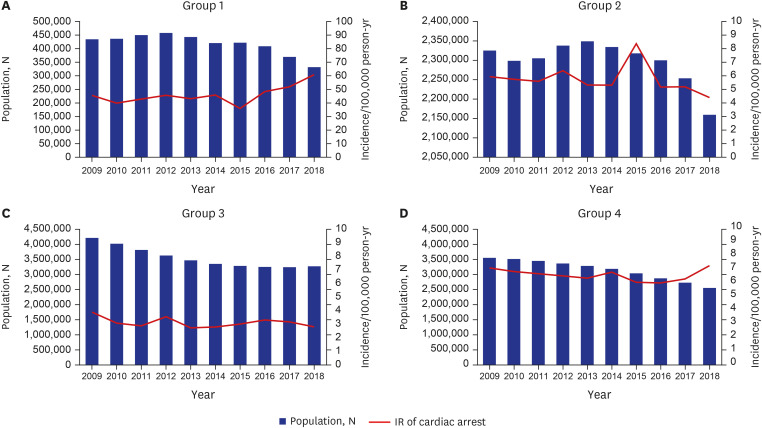
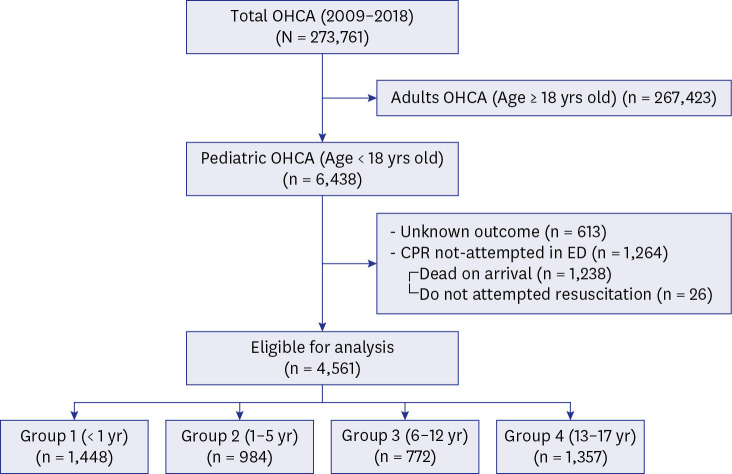
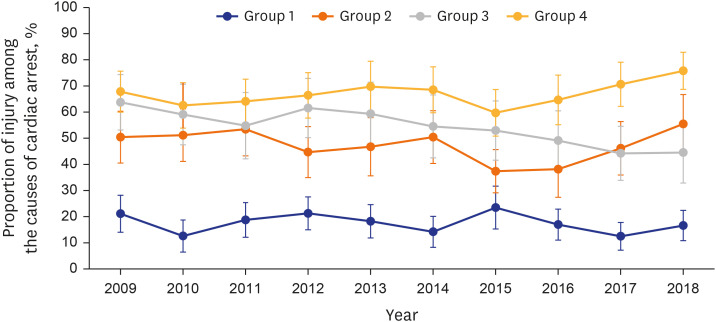
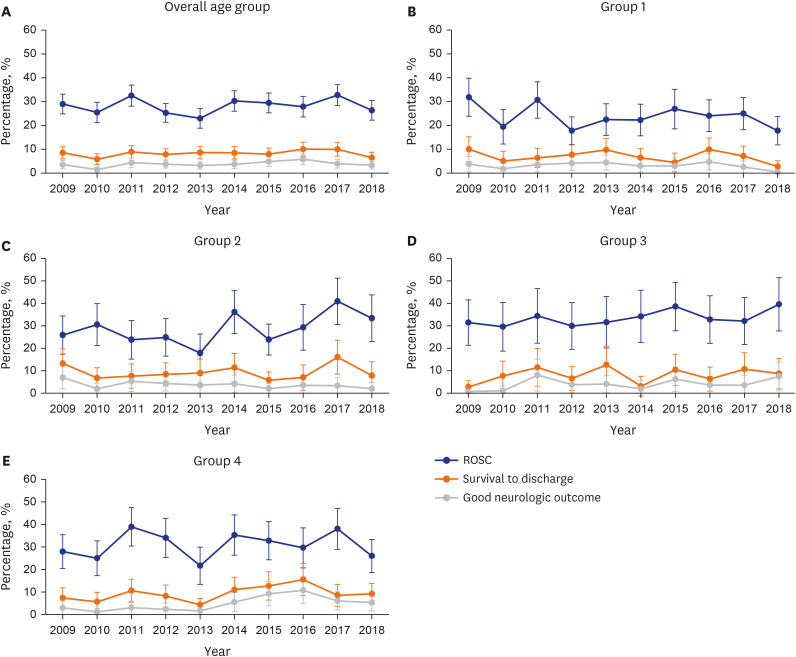
We identified 4,561 OHCA patients younger than 18 years between January 2009 and December 2018 in the Korean OHCA Registry. The patients were divided into four groups: group 1 (1 year or younger), group 2 (1 to 5 years), group 3 (6 to 12 years), and group 4 (13 to 17 years). The primary outcome was survival to hospital discharge, and the secondary outcomes were return of spontaneous circulation (ROSC) at the emergency department (ED) and good neurological status at discharge. Multivariate logistic analyses were performed.
Results
The incidence rate of pediatric OHCA in group 1 increased from 45.57 to 60.89 per 100,000 person-years, while that of the overall population decreased over the 10 years. The rates of ROSC at the ED, survival to hospital discharge, and good neurologic outcome were highest in group 4 (37.9%, 9.7%, 4.9%, respectively) and lowest in group 1 (28.3%, 7.1%, 3.2%). The positive factors for survival to discharge were event location of a public/commercial building or place of recreation, type of first responder, prehospital delivery of automated external defibrillator shock, initial shockable rhythm at the ED. The factors affecting survival outcomes differed by age group.
Conclusion
This study reports comprehensive trends in pediatric OHCA in the Republic of Korea. Our findings imply that preventive methods for the targeted population should be customized by age group.
Keyword
Figure
Reference
-
1. Wong CX, Brown A, Lau DH, Chugh SS, Albert CM, Kalman JM, et al. Epidemiology of sudden cardiac death: global and regional perspectives. Heart Lung Circ. 2019; 28(1):6–14. PMID: 30482683.2. Engdahl J, Axelsson A, Bång A, Karlson BW, Herlitz J. The epidemiology of cardiac arrest in children and young adults. Resuscitation. 2003; 58(2):131–138. PMID: 12909374.3. Fink EL, Prince DK, Kaltman JR, Atkins DL, Austin M, Warden C, et al. Unchanged pediatric out-of-hospital cardiac arrest incidence and survival rates with regional variation in North America. Resuscitation. 2016; 107:121–128. PMID: 27565862.4. Herlitz J, Svensson L, Engdahl J, Gelberg J, Silfverstolpe J, Wisten A, et al. Characteristics of cardiac arrest and resuscitation by age group: an analysis from the Swedish Cardiac Arrest Registry. Am J Emerg Med. 2007; 25(9):1025–1031. PMID: 18022497.5. Nichol G, Thomas E, Callaway CW, Hedges J, Powell JL, Aufderheide TP, et al. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008; 300(12):1423–1431. PMID: 18812533.6. Park CB, Shin SD, Suh GJ, Ahn KO, Cha WC, Song KJ, et al. Pediatric out-of-hospital cardiac arrest in Korea: a nationwide population-based study. Resuscitation. 2010; 81(5):512–517. PMID: 20172641.7. Young KD, Gausche-Hill M, McClung CD, Lewis RJ. A prospective, population-based study of the epidemiology and outcome of out-of-hospital pediatric cardiopulmonary arrest. Pediatrics. 2004; 114(1):157–164. PMID: 15231922.8. Richman PB, Nashed AH. The etiology of cardiac arrest in children and young adults: special considerations for ED management. Am J Emerg Med. 1999; 17(3):264–270. PMID: 10337887.9. Ronco R, King W, Donley DK, Tilden SJ. Outcome and cost at a children’s hospital following resuscitation for out-of-hospital cardiopulmonary arrest. Arch Pediatr Adolesc Med. 1995; 149(2):210–214. PMID: 7849887.10. Schindler MB, Bohn D, Cox PN, McCrindle BW, Jarvis A, Edmonds J, et al. Outcome of out-of-hospital cardiac or respiratory arrest in children. N Engl J Med. 1996; 335(20):1473–1479. PMID: 8890097.11. Atkins DL, Everson-Stewart S, Sears GK, Daya M, Osmond MH, Warden CR, et al. Epidemiology and outcomes from out-of-hospital cardiac arrest in children: the Resuscitation Outcomes Consortium Epistry-Cardiac Arrest. Circulation. 2009; 119(11):1484–1491. PMID: 19273724.12. Kim YT, Shin SD, Hong SO, Ahn KO, Ro YS, Song KJ, et al. Effect of national implementation of utstein recommendation from the global resuscitation alliance on ten steps to improve outcomes from Out-of-Hospital cardiac arrest: a ten-year observational study in Korea. BMJ Open. 2017; 7(8):e016925.13. Hwang SO, Cha KC, Jung WJ, Roh YI, Kim TY, Chung SP, et al. 2020 Korean guidelines for cardiopulmonary resuscitation. Part 2. Environment for cardiac arrest survival and the chain of survival. Clin Exp Emerg Med. 2021; 8(S):S8–14. PMID: 34034446.14. Ahn JY, Lee MJ, Kim H, Yoon HD, Jang HY. Epidemiological and survival trends of pediatric cardiac arrests in emergency departments in Korea: a cross-sectional, nationwide report. J Korean Med Sci. 2015; 30(9):1354–1360. PMID: 26339179.15. Yoon H, Kwon Y, An J, Hong S, Kim YT. Main outcomes of the sudden cardiac arrest survey 2006 to 2016. Clin Exp Emerg Med. 2019; 6(2):183–188. PMID: 31261487.16. McNally B, Stokes A, Crouch A, Kellermann AL. CARES Surveillance Group. CARES: Cardiac Arrest Registry to Enhance Survival. Ann Emerg Med. 2009; 54(5):674–683.e2. PMID: 19394110.17. Tanner R, Masterson S, Galvin J, Wright P, Hennelly D, Murphy A, et al. Out-of-hospital cardiac arrests in the young population; a 6-year review of the Irish out-of-hospital cardiac arrest register. Postgrad Med J. 2021; 97(1147):280–285. PMID: 32371406.18. Donohoe RT, Innes J, Gadd S, Whitbread M, Moore F. Out-of-hospital cardiac arrest in patients aged 35 years and under: a 4-year study of frequency and survival in London. Resuscitation. 2010; 81(1):36–41. PMID: 19913971.19. Deasy C, Bernard SA, Cameron P, Jaison A, Smith K, Harriss L, et al. Epidemiology of paediatric out-of-hospital cardiac arrest in Melbourne, Australia. Resuscitation. 2010; 81(9):1095–1100. PMID: 20627518.20. Matsui S, Kitamura T, Sado J, Kiyohara K, Kobayashi D, Kiguchi T, et al. Location of arrest and survival from out-of-hospital cardiac arrest among children in the public-access defibrillation era in Japan. Resuscitation. 2019; 140:150–158. PMID: 31075289.21. Marijianowski MM, van der Loos CM, Mohrschladt MF, Becker AE. The neonatal heart has a relatively high content of total collagen and type I collagen, a condition that may explain the less compliant state. J Am Coll Cardiol. 1994; 23(5):1204–1208. PMID: 8144790.22. Vrancken SL, van Heijst AF, de Boode WP. Neonatal hemodynamics: from developmental physiology to comprehensive monitoring. Front Pediatr. 2018; 6:87. PMID: 29675404.23. Rowland DG, Gutgesell HP. Noninvasive assessment of myocardial contractility, preload, and afterload in healthy newborn infants. Am J Cardiol. 1995; 75(12):818–821. PMID: 7717287.24. Figaji AA. Anatomical and physiological differences between children and adults relevant to traumatic brain injury and the implications for clinical assessment and care. Front Neurol. 2017; 8:685. PMID: 29312119.25. McNally B, Robb R, Mehta M, Vellano K, Valderrama AL, Yoon PW, et al. Out-of-hospital cardiac arrest surveillance --- Cardiac Arrest Registry to Enhance Survival (CARES), United States, October 1, 2005--December 31, 2010. MMWR Surveill Summ. 2011; 60(8):1–19.26. Okamoto Y, Iwami T, Kitamura T, Nitta M, Hiraide A, Morishima T, et al. Regional variation in survival following pediatric out-of-hospital cardiac arrest. Circ J. 2013; 77(10):2596–2603. PMID: 23823852.27. Korean Statistical Information Service. Population, households and housing units 2021. Updated 2021. Accessed July 20, 2022. https://kosis.kr/statHtml/statHtml.do?orgId=116&tblId=DT_MLTM_448&vw_cd=MT_ETITLE&list_id=I2_1&scrId=&language=en&seqNo=&lang_mode=en&obj_var_id=&itm_id=&conn_path=MT_ETITLE&path=%252Feng%252FstatisticsList%252FstatisticsListIndex.do .28. Korean Statistical Information Service. Cadastral statistics 2021. Updated 2021. Accessed July 20, 2022. https://kosis.kr/statHtml/statHtml.do?orgId=116&tblId=DT_MLTM_448&conn_path=I2&language=en .29. National Fire Agency (KR). Statistical Yearbook of Emergency Services 2022. Sejong, Korea: National Fire Agency;2022.30. Korean Statistical Information Service. Summary of census population 2021. Updated 2021. Accessed February 7, 2022. https://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1B040M1&conn_path=I2 .31. Korean Statistical Information Service. Statistical information report of Korea OHCA Registry 2018. Updated 2019. Accessed July 20, 2022. https://kostat.go.kr/portal/korea/kor_pi/8/7/index.board?bmode=read&aSeq=372579&pageNo=24&rowNum=10&amSeq=&sTarget=&sTxt= .32. Ro YS, Shin SD, Song KJ, Lee EJ, Kim JY, Ahn KO, et al. A trend in epidemiology and outcomes of out-of-hospital cardiac arrest by urbanization level: a nationwide observational study from 2006 to 2010 in South Korea. Resuscitation. 2013; 84(5):547–557. PMID: 23313428.33. Tham LP, Wah W, Phillips R, Shahidah N, Ng YY, Shin SD, et al. Epidemiology and outcome of paediatric out-of-hospital cardiac arrests: a paediatric sub-study of the Pan-Asian resuscitation outcomes study (PAROS). Resuscitation. 2018; 125:111–117. PMID: 29421664.34. Rajan S, Wissenberg M, Folke F, Hansen CM, Lippert FK, Weeke P, et al. Out-of-hospital cardiac arrests in children and adolescents: incidences, outcomes, and household socioeconomic status. Resuscitation. 2015; 88:12–19. PMID: 25500748.35. Wissenberg M, Lippert FK, Folke F, Weeke P, Hansen CM, Christensen EF, et al. Association of national initiatives to improve cardiac arrest management with rates of bystander intervention and patient survival after out-of-hospital cardiac arrest. JAMA. 2013; 310(13):1377–1384. PMID: 24084923.36. Choi YH, Kim DK, Kang EK, Kim JT, Na JY, Park B, et al. 2020 Korean guidelines for cardiopulmonary resuscitation. Part 7. Pediatric advanced life support. Clin Exp Emerg Med. 2021; 8(S):S81–S95. PMID: 34034451.37. Heo JS, Kim SY, Park HW, Choi YS, Park CW, Cho GJ, et al. 2020 Korean guidelines for cardiopulmonary resuscitation. Part 8. Neonatal resuscitation. Clin Exp Emerg Med. 2021; 8(S):S96–115. PMID: 34034452.38. Moon RY. Task Force on Sudden Infant Death Syndrome. SIDS and other sleep-related infant deaths: updated 2016 recommendations for a safe infant sleeping environment. Pediatrics. 2016; 138(5):e20162940. PMID: 27940805.39. Athanasakis E, Karavasiliadou S, Styliadis I. The factors contributing to the risk of sudden infant death syndrome. Hippokratia. 2011; 15(2):127–131. PMID: 22110293.40. Yun SH, Lee KM, Kim JH, Kim JS, Paik JH, Kim H, et al. Outcome of pediatric out-of-hospital cardiac arrest. J Korean Soc Emerg Med. 2007; 18(3):202–210.41. Kiyohara K, Sakai T, Nishiyama C, Nishiuchi T, Hayashi Y, Iwami T, et al. Epidemiology of out-of-hospital cardiac arrest due to suffocation focusing on suffocation due to Japanese rice cake: a population-based observational study from the Utstein Osaka Project. J Epidemiol. 2018; 28(2):67–74. PMID: 29093354.42. Statistics Korea. Causes of death statistics 2019. Updated 2019. Accessed July 22, 2022. https://kostat.go.kr/portal/korea/kor_nw/1/6/2/index.board?bmode=read&bSeq=&aSeq=377606&pageNo=1&rowNum=10&navCount=10&currPg=&searchInfo=&sTarget=title&sTxt= .43. Statistics Korea. Early childhood education enrollment rate 2022. Updated 2022. Accessed July 22, 2022. https://www.index.go.kr/unify/idx-info.do?idxCd=8023 .44. Sasson C, Rogers MA, Dahl J, Kellermann AL. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2010; 3(1):63–81. PMID: 20123673.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- In-hospital Pediatric Cardiopulmonary Resuscitation According to Pediatric Utstein Template
- Cardiac Arrest During Pediatric Anesthesia
- A Case of Cardiac Arrest due to Oculoeardiac Reflex: A Case Report
- Cardiac Arrest During General Anesthesia - Report of 10 cases
- Pediatric out-of-hospital cardiac arrest: incidence and outcomes in an urban city