J Liver Cancer.
2022 Sep;22(2):146-157. 10.17998/jlc.2022.08.22.
Indications for open hepatectomy in the era of laparoscopic liver resection: a high volume single institutional study
- Affiliations
-
- 1Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2534241
- DOI: http://doi.org/10.17998/jlc.2022.08.22
Abstract
- Background
/Aim: Since the introduction of laparoscopy for liver resection in the 1990s, the performance of laparoscopic liver resection (LLR) has been steadily increasing. However, there is currently no data on the extent to which laparoscopy is used for liver resection. Herein, we investigated the extent to which laparoscopy is performed in liver resection and sought to determine whether surgeons prefer laparoscopy or laparotomy in the posterosuperior (PS) segment.
Methods
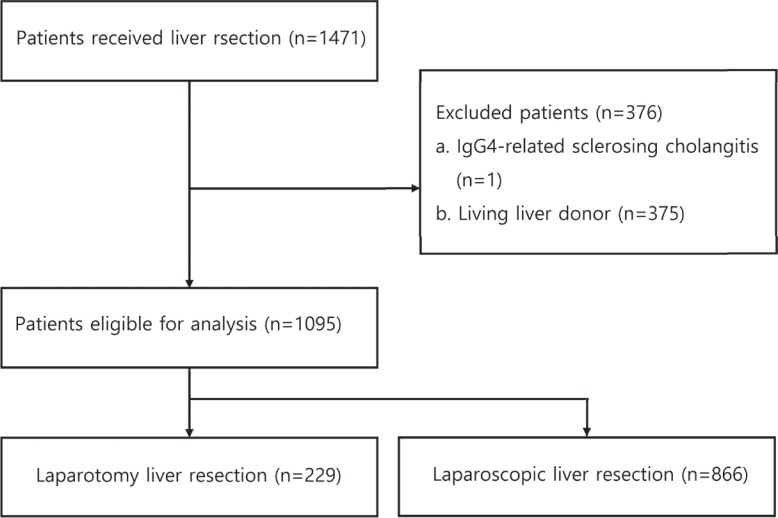
For this retrospective observational study, we enrolled patients who had undergone liver resection at the Samsung Medical Center between January 2020 and December 2021. The proportion of LLR in liver resection was calculated, and the incidence and causes of open conversion were investigated.
Results
A total of 1,095 patients were included in this study. LLR accounted for 79% of the total liver resections. The percentage of previous hepatectomy (16.2% vs. 5.9%, P<0.001) and maximum tumor size (median 4.8 vs. 2.8, P<0.001) were higher in the open liver resection (OLR) group. Subgroup analysis revealed that tumor size (median 6.3 vs. 2.9, P<0.001) and surgical extent (P<0.001) in the OLR group were larger than those in the LLR group. The most common cause of open conversion (OC) was adhesion (57%), and all OC patients had tumors in the PS.
Conclusions
We investigated the recent preference of practical surgeons in liver resection, and found that surgeons preferred OLR to LLR when treating a large tumor located in the PS.
Figure
Cited by 1 articles
-
A systematic review and meta-analysis of blood transfusion rates during liver resection by country
Seonju Kim, Yun Kyung Jung, Kyeong Geun Lee, Kyeong Sik Kim, Hanjun Kim, Dongho Choi, Sumi Lee, Boyoung Park
Ann Surg Treat Res. 2023;105(6):404-416. doi: 10.4174/astr.2023.105.6.404.
Reference
-
1. Buell JF, Cherqui D, Geller DA, O'Rourke N, Iannitti D, Dagher I, et al. The international position on laparoscopic liver surgery: the Louisville Statement, 2008. Ann Surg. 2009; 250:825–830.2. Troisi RI, Montalti R, Van Limmen JG, Cavaniglia D, Reyntjens K, Rogiers X, et al. Risk factors and management of conversions to an open approach in laparoscopic liver resection: analysis of 265 consecutive cases. HPB (Oxford). 2014; 16:75–82.3. Nguyen KT, Gamblin TC, Geller DA. World review of laparoscopic liver resection-2,804 patients. Ann Surg. 2009; 250:831–841.4. Reich H, McGlynn F, DeCaprio J, Budin R. Laparoscopic excision of benign liver lesions. Obstet Gynecol. 1991; 78:956–958.5. Kwon CHD, Choi GS, Joh JW. Laparoscopic right hepatectomy for living donor. Curr Opin Organ Transplant. 2019; 24:167–174.6. Wakabayashi G, Cherqui D, Geller DA, Buell JF, Kaneko H, Han HS, et al. Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in Morioka. Ann Surg. 2015; 261:619–629.7. Ban D, Tanabe M, Ito H, Otsuka Y, Nitta H, Abe Y, et al. A novel difficulty scoring system for laparoscopic liver resection. J Hepatobiliary Pancreat Sci. 2014; 21:745–753.8. Teo JY, Kam JH, Chan CY, Goh BK, Wong JS, Lee VT, et al. Laparoscopic liver resection for posterosuperior and anterolateral lesionsa comparison experience in an Asian centre. Hepatobiliary Surg Nutr. 2015; 4:379–390.9. Zheng B, Zhao R, Li X, Li B. Comparison of laparoscopic liver resection for lesions located in anterolateral and posterosuperior segments: a meta-analysis. Surg Endosc. 2017; 31:4641–4648.10. Liu F, Li Q, Wei Y, Li B. Laparoscopic versus open liver resection for difficult lesions: a meta-analysis. J Laparoendosc Adv Surg Tech A. 2018; 28:1428–1436.11. Cho W, Kwon CHD, Choi JY, Lee SH, Kim JM, Choi GS, et al. Impact of technical innovation on surgical outcome of laparoscopic major liver resection: 10 years' experience at a large-volume center. Ann Surg Treat Res. 2019; 96:14–18.12. Pugh RN, Murray-Lyon IM, Dawson JL, Pietroni MC, Williams R. Transection of the oesophagus for bleeding oesophageal varices. Br J Surg. 1973; 60:646–649.13. Kim JM, Kim S, Rhu J, Choi GS, Kwon CHD, Joh JW. Elderly hepatocellular carcinoma patients: open or laparoscopic approach? Cancers (Basel). 2020; 12:2281.14. Orcutt ST, Anaya DA. Liver resection and surgical strategies for management of primary liver cancer. Cancer Control. 2018; 25:1073274817744621.15. Hasegawa Y, Wakabayashi G, Nitta H, Takahara T, Katagiri H, Umemura A, et al. A novel model for prediction of pure laparoscopic liver resection surgical difficulty. Surg Endosc. 2017; 31:5356–5363.16. Ciria R, Cherqui D, Geller DA, Briceno J, Wakabayashi G. Comparative short-term benefits of laparoscopic liver resection: 9000 cases and climbing. Ann Surg. 2016; 263:761–777.17. Scuderi V, Barkhatov L, Montalti R, Ratti F, Cipriani F, Pardo F, et al. Outcome after laparoscopic and open resections of posterosuperior segments of the liver. Br J Surg. 2017; 104:751–759.18. Guro H, Cho JY, Han HS, Yoon YS, Choi Y, Jang JS, et al. Laparoscopic liver resection of hepatocellular carcinoma located in segments 7 or 8. Surg Endosc. 2018; 32:872–878.19. Tzanis D, Shivathirthan N, Laurent A, Abu Hilal M, Soubrane O, Kazaryan AM, et al. European experience of laparoscopic major hepatectomy. J Hepatobiliary Pancreat Sci. 2013; 20:120–124.20. Li L, Xu L, Wang P, Zhang M, Li B. The risk factors of intraoperative conversion during laparoscopic hepatectomy: a systematic review and meta-analysis. Langenbecks Arch Surg. 2022; 407:469–478.21. Goh BK, Chan CY, Wong JS, Lee SY, Lee VT, Cheow PC, et al. Factors associated with and outcomes of open conversion after laparoscopic minor hepatectomy: initial experience at a single institution. Surg Endosc. 2015; 29:2636–2642.22. Cauchy F, Fuks D, Nomi T, Schwarz L, Barbier L, Dokmak S, et al. Risk factors and consequences of conversion in laparoscopic major liver resection. Br J Surg. 2015; 102:785–795.23. Levi Sandri GB, Ettorre GM, Aldrighetti L, Cillo U, Dalla Valle R, Guglielmi A, et al. Laparoscopic liver resection of hepatocellular carcinoma located in unfavorable segments: a propensity score-matched analysis from the I Go MILS (Italian Group of Minimally Invasive Liver Surgery) Registry. Surg Endosc. 2019; 33:1451–1458.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Early experience of laparoscopic liver resection: A single institution experience with 37 consecutive cases
- A Single Center Experience for a Feasibility of Totally Laparoscopic Living Donor Right Hepatectomy
- Robotic-assisted right hepatectomy via anterior approach for intrahepatic cholangiocarcinoma
- How to minimize conversion to open surgery during laparoscopic liver resection: the point of view of hemostasis
- The usefulness of the totally intra-corporeal pringle maneuver with Penrose drain tube during laparoscopic left side liver resection