Ann Surg Treat Res.
2022 Oct;103(4):205-216. 10.4174/astr.2022.103.4.205.
Is craniocaudal dissection of recurrent laryngeal nerve safer than lateral approach: a prospective randomized study comparing both techniques by using continuous intraoperative nerve monitoring
- Affiliations
-
- 1Division of Endocrine Surgery, Department of General Surgery, Istanbul Faculty of Medicine, Istanbul University, Istanbul, Turkey
- 2Division of Endocrine Surgery, Department of General Surgery, Sisli Hamidiye Etfal Training and Research Hospital, University of Health Sciences Turkey, Istanbul, Turkey
- KMID: 2534123
- DOI: http://doi.org/10.4174/astr.2022.103.4.205
Abstract
- Purpose
This study was performed to compare the real-time electromyographic (EMG) changes and the rate of recurrent laryngeal nerve (RLN) injury in craniocaudal and lateral approaches for RLN during thyroidectomy.
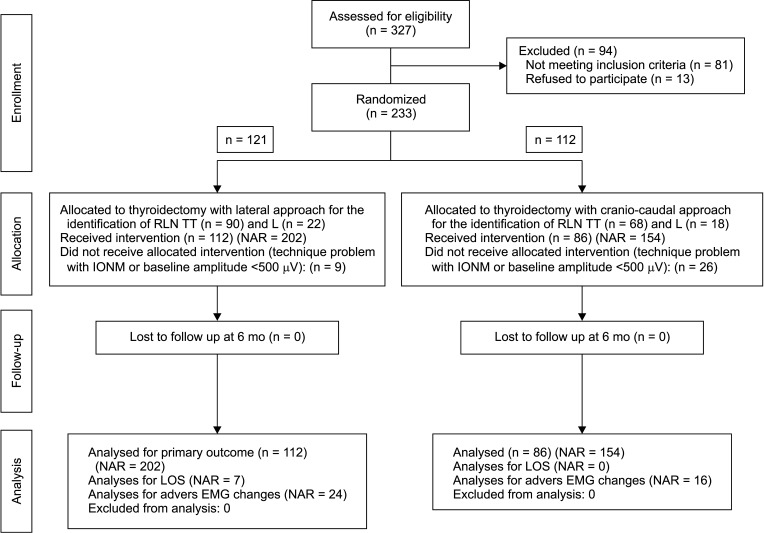
Methods
One hundred twelve and 86 patients were prospectively randomized to receive lateral (group 1) or craniocaudal (group 2) approach to RLN, respectively, under continuous intraoperative nerve monitoring.
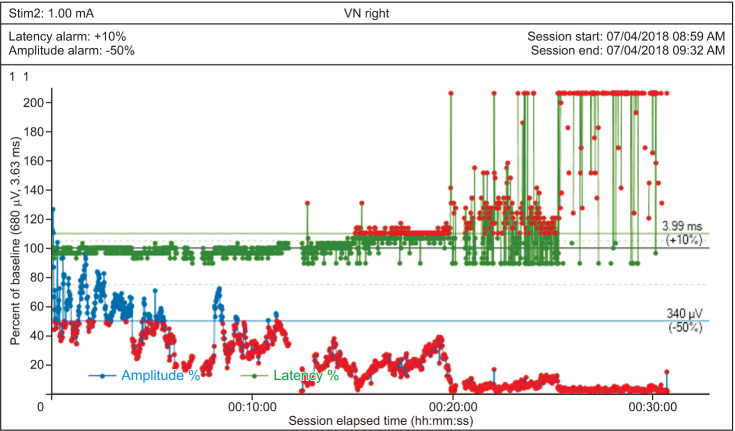
Results
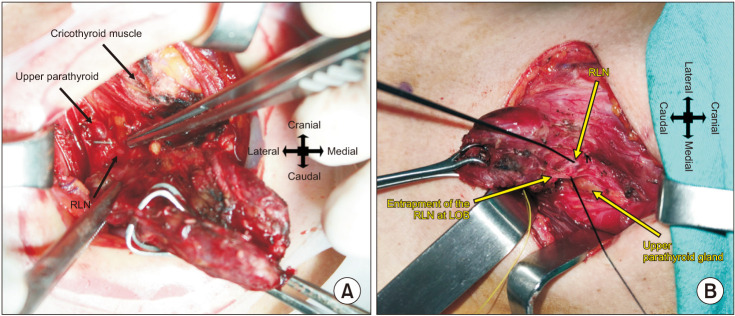
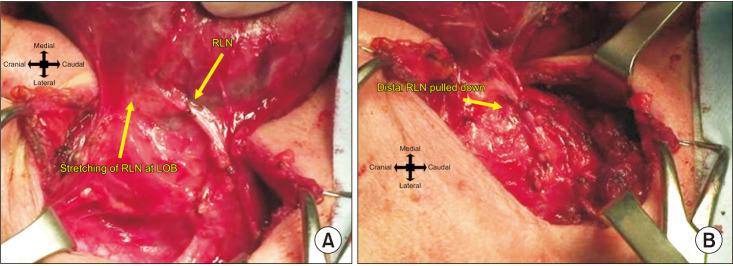
Loss of signal (LOS) occurred in 7 (2.0%) of 356 nerves at risk (NAR). LOS was significantly associated with repeated adverse EMG changes and presence of RLN entrapment at the ligament of Berry (LOB), which was accompanied by other clinicopathological or anatomical features, such as tubercle of Zuckerkandl (TZ), extralaryngeal branching, hyperthyroidism, autoimmune thyroid disease (ATD), or thyroid lobe volume of >29 cm 3 (P = 0.001 and P = 0.030, respectively). The rate of repeated adverse EMG changes and LOS in the NARs with LOB entrapment accompanied by other clinicopathological and anatomical features was higher in group 1 vs. group 2 (11.1% vs. 2.2%, respectively and 9.7% vs. 0%, respectively; P = 0.070). The total rate of vocal cord palsy (VCP) was significantly higher in group 1 than in group 2 (P = 0.005). The rate of permanent VCP showed no significant difference between the 2 groups.
Conclusion
The craniocaudal approach to the RLN is safer than the lateral approach in the RLNs with entrapment at the LOB accompanied by other features, such as TZ, extralaryngeal branching, hyperthyroidism, ATD, or high thyroid lobe volume.
Keyword
Figure
Reference
-
1. Angelos P. Recurrent laryngeal nerve monitoring: state of the art, ethical and legal issues. Surg Clin North Am. 2009; 89:1157–1169. PMID: 19836490.
Article2. Randolph GW, Dralle H, Abdullah H, Barczynski M, Bellantone R, et al. International Intraoperative Monitoring Study Group. Electrophysiologic recurrent laryngeal nerve monitoring during thyroid and parathyroid surgery: international standards guideline statement. Laryngoscope. 2011; 121 Suppl 1:S1–S16. PMID: 21181860.
Article3. Jatzko GR, Lisborg PH, Müller MG, Wette VM. Recurrent nerve palsy after thyroid operations--principal nerve identification and a literature review. Surgery. 1994; 115:139–144. PMID: 8310401.4. Dralle H, Sekulla C, Lorenz K, Brauckhoff M, Machens A. German IONM Study Group. Intraoperative monitoring of the recurrent laryngeal nerve in thyroid surgery. World J Surg. 2008; 32:1358–1366. PMID: 18305996.
Article5. Barczyński M, Konturek A, Cichoń S. Randomized clinical trial of visualization versus neuromonitoring of recurrent laryngeal nerves during thyroidectomy. Br J Surg. 2009; 96:240–246. PMID: 19177420.
Article6. Phelan E, Schneider R, Lorenz K, Dralle H, Kamani D, Potenza A, et al. Continuous vagal IONM prevents recurrent laryngeal nerve paralysis by revealing initial EMG changes of impending neuropraxic injury: a prospective, multicenter study. Laryngoscope. 2014; 124:1498–1505. PMID: 24307596.
Article7. Schneider R, Randolph GW, Sekulla C, Phelan E, Thanh PN, Bucher M, et al. Continuous intraoperative vagus nerve stimulation for identification of imminent recurrent laryngeal nerve injury. Head Neck. 2013; 35:1591–1598. PMID: 23169450.
Article8. Anuwong A. Transoral endoscopic thyroidectomy vestibular approach: a series of the first 60 human cases. World J Surg. 2016; 40:491–497. PMID: 26546193.
Article9. Shindo ML, Wu JC, Park EE. Surgical anatomy of the recurrent laryngeal nerve revisited. Otolaryngol Head Neck Surg. 2005; 133:514–519. PMID: 16213921.
Article10. Veyseller B, Aksoy F, Yildirim YS, Karatas A, Ozturan O. Effect of recurrent laryngeal nerve identification technique in thyroidectomy on recurrent laryngeal nerve paralysis and hypoparathyroidism. Arch Otolaryngol Head Neck Surg. 2011; 137:897–900. PMID: 21844405.
Article11. Sykes RF, Moorthy R, Olaleye O, Black IM. Identification of the recurrent laryngeal nerve at the cricothyroid joint: our experience of 181 thyroid procedures. Clin Otolaryngol. 2014; 39:174–177. PMID: 24801664.
Article12. Butskiy O, Chang BA, Luu K, McKenzie RM, Anderson DW. A systemat ic approach to the recurrent laryngeal nerve dissection at the cricothyroid junction. J Otolaryngol Head Neck Surg. 2018; 47:57. PMID: 30223884.
Article13. Fatogoma Issa K, Sidiki D, Naouma C, Kassim D, N’Faly K, Djibril S, et al. Superior approach of recurrent laryngeal nerve: review of the literature. J Thyroid Res. 2019; 2019:5671816. PMID: 31949891.
Article14. Knudsen N, Bols B, Bülow I, Jørgensen T, Perrild H, Ovesen L, et al. Validation of ultrasonography of the thyroid gland for epidemiological purposes. Thyroid. 1999; 9:1069–1074. PMID: 10595454.
Article15. Dozois RR, Beahrs OH. Surgical anatomy and technique of thyroid and parathyroid surgery. Surg Clin North Am. 1977; 57:647–661. PMID: 897961.
Article16. Schneider R, Sekulla C, Machens A, Lorenz K, Thanh PN, Dralle H. Dynamics of loss and recovery of the nerve monitoring signal during thyroidectomy predict early postoperative vocal fold function. Head Neck. 2016; 38 Suppl 1:E1144–E1151. PMID: 26331940.
Article17. Fundakowski CE, Hales NW, Agrawal N, Barczyński M, Camacho PM, Hartl DM, et al. Surgical management of the recurrent laryngeal nerve in thyroidectomy: American Head and Neck Society Consensus Statement. Head Neck. 2018; 40:663–675. PMID: 29461666.
Article18. Anuwong A, Ketwong K, Jitpratoom P, Sasanakietkul T, Duh QY. Safety and outcomes of the transoral endoscopic thyroidectomy vestibular approach. JAMA Surg. 2018; 153:21–27. PMID: 28877292.
Article19. Minuto MN, Reina S, Monti E, Ansaldo GL, Varaldo E. Morbidity following thyroid surgery: acceptable rates and how to manage complicated patients. J Endocrinol Invest. 2019; 42:1291–1297. PMID: 31124043.
Article20. Page C, Peltier J, Charlet L, Laude M, Strunski V. Superior approach to the inferior laryngeal nerve in thyroid surgery: anatomy, surgical technique and indications. Surg Radiol Anat. 2006; 28:631–636. PMID: 16937027.
Article21. Schneider R, Randolph G, Dionigi G, Barczyński M, Chiang FY, Triponez F, et al. Prospective study of vocal fold function after loss of the neuromonitoring signal in thyroid surgery: the International Neural Monitoring Study Group’s POLT study. Laryngoscope. 2016; 126:1260–1266. PMID: 26667156.
Article22. Chiang FY, Lu IC, Kuo WR, Lee KW, Chang NC, Wu CW. The mechanism of recurrent laryngeal nerve injury during thyroid surgery: the application of intraoperative neuromonitoring. Surgery. 2008; 143:743–749. PMID: 18549890.
Article23. Dionigi G, Wu CW, Kim HY, Rausei S, Boni L, Chiang FY. Severity of recurrent laryngeal ner ve ınjuries in thyroid surgery. World J Surg. 2016; 40:1373–1381. PMID: 26817650.
Article24. Dionigi G, Snyder SK, Chiang FY, Liddy W, Kamani D, Kyriazidis N. Mechanism of injury. Randolph GW, editor. The recurrent and superior laryngeal nerves. Springer Int;2016. p. 223–238.25. Wu CW, Dionigi G, Sun H, Liu X, Kim HY, Hsiao PJ, et al. Intraoperative neuromonitoring for the early detection and prevention of RLN traction injury in thyroid surgery: a porcine model. Surgery. 2014; 155:329–339. PMID: 24084598.
Article26. Reeve T, Thompson NW. Complications of thyroid surgery: how to avoid them, how to manage them, and observations on their possible effect on the whole patient. World J Surg. 2000; 24:971–975. PMID: 10865043.
Article27. Loré JM Jr, Banyas JB, Niemiec ER. Complications of total thyroidectomy. Arch Otolaryngol Head Neck Surg. 1987; 113:1238.28. Randolph GW. Surgery of the thyroid and parathyroid glands. Philadelphia: Saunders;2003.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Concurrent Ipsilateral Recurrent and Nonrecurrent Laryngeal Nerve During Thyroidectomy: A Case Report
- Intraoperative Recurrent Laryngeal Nerve Monitoring in a Patient with Contralateral Vocal Fold Palsy
- Precision and protection: advancements and future of neuromonitoring techniques for laryngeal surgery
- The Present and Future of Intraoperative Neuromonitoring in Thyroid Surgery
- Preservation of the superior laryngeal nerve without neuromonitoring during thyroid surgery