Obstet Gynecol Sci.
2022 Sep;65(5):430-440. 10.5468/ogs.22053.
Endometrial thickness and uterine artery Doppler parameters as soft markers for prediction of endometrial cancer in postmenopausal bleeding women: a cross-sectional study at tertiary referral hospitals from Vietnam
- Affiliations
-
- 1Department of High-risk Pregnancy, Tu Du Hospital, Ho Chi Minh, Vietnam
- 2Department of Obstetrics and Gynecology, Hue Medical College, Hue University, Thua Thien Hue, Vietnam
- KMID: 2533816
- DOI: http://doi.org/10.5468/ogs.22053
Abstract
Objective
To determine the value of endometrial thickness (ET) and Doppler indices of uterine artery (UtA) as sonographic markers in predicting endometrial cancer (EC) among postmenopausal bleeding (PMB) women in low-resource settings as Vietnam.
Methods
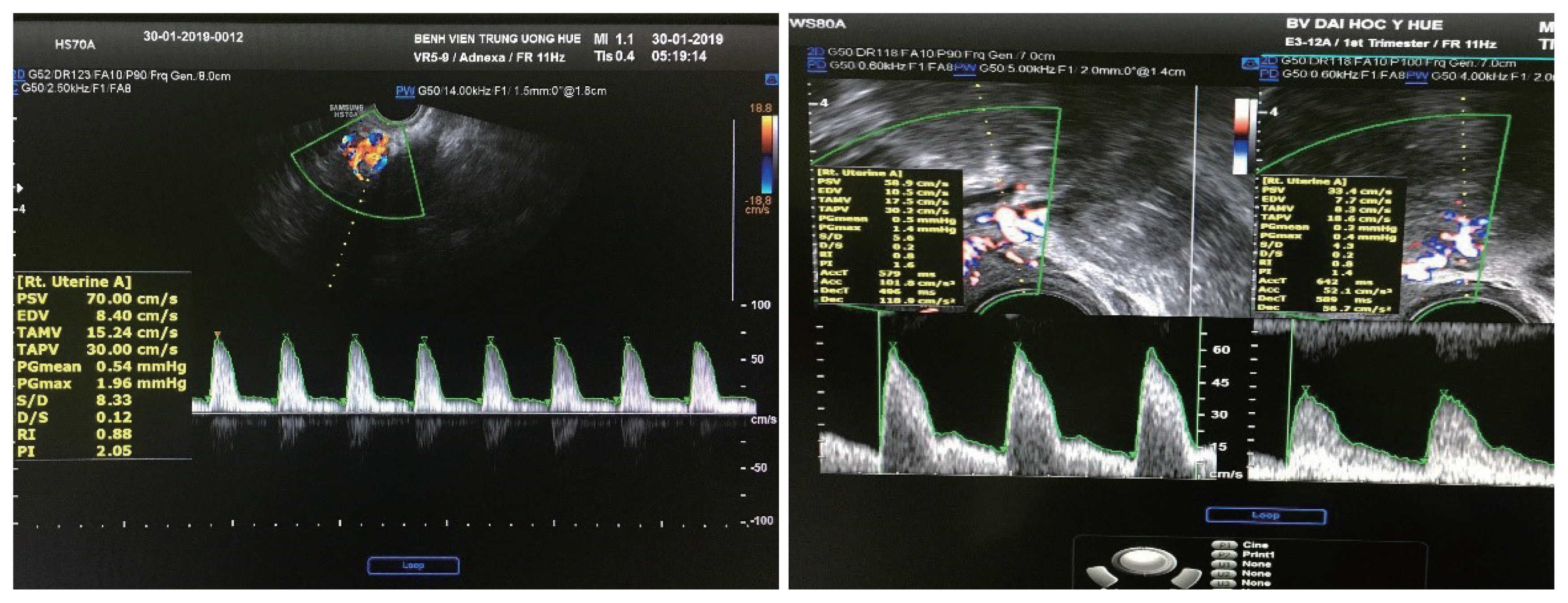
This cross-sectional study was conducted at the Hue University Hospital and Hue Central Hospital between June 2016 and June 2019. The study enrolled all women who complained of PMB and were followed by transvaginal Doppler ultrasound. Their definitive histopathological examination was the gold standard for comparison.
Results
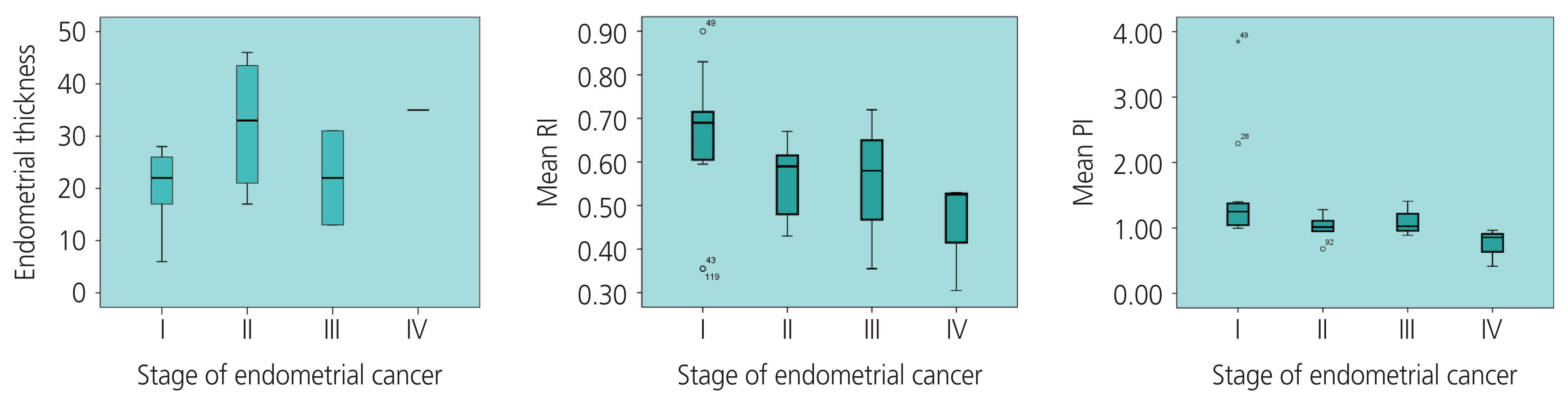
The UtA Doppler indices, including resistance index (RI), pulsatility index (PI), and peak systolic velocity (PSV), were significantly lower in the malignant group than in the benign group. The threshold values of the UtA, RI ≤0.73 and PI ≤1.42, were found with an area under receiver operating characteristic curve (AUC) of 0.85-0.88, and the sensitivity and specificity were 91.3% and 83.3%, respectively. Unlike PSV, the diagnostic value was the lowest, with an AUC of 0.72. ET was a good predictor for the diagnosis of EC, with an AUC of 0.89. In women with PMB, when using the cutoff value of EC more than 12.5 mm, the sensitivity and specificity were 93.8% and 77.8%, respectively. In addition, the higher the stage of EC, the lower the RI and PI and the greater the EC.
Conclusion
ET, and RI, PI, and PSV of the UtA could help in differentiating malignant from benign endometrial changes. Pulsed ultrasonic Doppler velocimetry seems to play a role in predicting the higher stages of EC. Further studies are needed to confirm these findings.
Keyword
Figure
Reference
-
References
1. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021; 71:209–49.
Article2. Bengtsen MB, Veres K, Nørgaard M. First-time postmenopausal bleeding as a clinical marker of long-term cancer risk: a Danish nationwide cohort study. Br J Cancer. 2020; 122:445–51.
Article3. Jones ER, O’Flynn H, Njoku K, Crosbie EJ. Detecting endometrial cancer. Obstet Gynaecol. 2021; 23:103–12.
Article4. Menzies R, Wallace S, Ennis M, Bennett A, Jacobson M, Yip G, et al. Significance of abnormal sonographic findings in postmenopausal women with and without bleeding. J Obstet Gynaecol Can. 2011; 33:944–51.
Article5. Khazaei Z, Dehkordi AH, Amiri M, Adineh HA, Sohrabivafa M, Darvishi I. The incidence and mortality of endometrial cancer and its association with body mass index and human development index in asian population. World Cancer Res J. 2018; 5:11.6. Hoffman BL, Schorge JO, Schaffer JI, Halvorson LM, Bradshaw KD, Cunningham FG. Williams gynecology. 2nd ed. New York (NY): McGraw-Hill Medical;2012.7. Ha HI, Chang HK, Park SJ, Lim J, Won YJ, Lim MC. The incidence and survival of cervical, ovarian, and endometrial cancer in Korea, 1999–2017: Korea central cancer registry. Obstet Gynecol Sci. 2021; 64:444–53.
Article8. Emoto M, Tamura R, Shirota K, Hachisuga T, Kawarabayashi T. Clinical usefulness of color Doppler ultrasound in patients with endometrial hyperplasia and carcinoma. Cancer. 2002; 94:700–6.
Article9. Khurana I, Satia MN. Preoperative evaluation of ovarian masses with color Doppler and its correlation with pathological fnding. Int J Reprod Contracept Obstet Gynecol. 2016; 5:2084–93.10. Nasheeha N, Gk P. Diagnostic accuracy of uterine artery and spiral artery Doppler for evaluation of endometrial pathology in postmenopausal bleeding. J Gynecol Obstet Hum Reprod. 2021; 50:102209.
Article11. Ahmadzade A, Gharibvand MM, Azhine S. Correlation of color Doppler ultrasound and pathological grading in endometrial carcinoma. J Family Med Prim Care. 2020; 9:5188–92.
Article12. Kumari P, Gaikwad HS, Nath B. Endometrial cut off thickness as predictor of endometrial pathology in perimenopausal women with abnormal uterine bleeding: a cross-sectional study. Obstet Gynecol Int. 2022; 2022:5073944.
Article13. Grangé G, Bargy F. Guide pratique de l’échographie obstétricale et gynécologie. 2nd ed. Paris: Elsevier Masson;2016.14. Leone FP, Timmerman D, Bourne T, Valentin L, Epstein E, Goldstein SR, et al. Terms, defnitions and measurements to describe the sonographic features of the endometrium and intrauterine lesions: a consensus opinion from the International Endometrial Tumor Analysis (IETA) group. Ultrasound Obstet Gynecol. 2010; 35:103–12.
Article15. Potier A. Apports pratiques du doppler en gynécologie. Paris: Collège National des Gynécologues et Obstétriciens français;1997.16. Bhide A, Acharya G, Bilardo CM, Brezinka C, Cafci D, Hernandez-Andrade E, et al. ISUOG practice guidelines: use of Doppler ultrasonography in obstetrics. Ultrasound Obstetet Gynecol. 2013; 41:233–9.17. Sobczuk K, Sobczuk A. New classifcation system of endometrial hyperplasia WHO 2014 and its clinical implications. Prz Menopauzalny. 2017; 16:107–11.18. Soslow RA, Tornos C, Park KJ, Malpica A, Matias-Guiu X, Oliva E, et al. Endometrial carcinoma diagnosis: use of FIGO grading and genomic subcategories in clinical practice: recommendations of the International Society of Gynecological Pathologists. Int J Gynecol Pathol. 2019; 38(Suppl 1(Iss 1 Suppl 1)):S64–74.19. Abu-Rustum NR, Zhou Q, Iasonos A, Alektiar KM, Leitao MM Jr, Chi DS, et al. The revised 2009 FIGO staging system for endometrial cancer: should the 1988 FIGO stages IA and IB be altered? Int J Gynecol Cancer. 2011; 21:511–6.
Article20. Mayuri M, Abha S, Narula MK. Role of transvaginal sonography, power doppler and hysteroscopy in women with abnormal uterine bleeding: a comparative study. IOSR J Dent Med Sci. 2014; 13:82–9.
Article21. Develioglu OH, Bilgin T, Yalcin OT, Ozalp S. Transvaginal ultrasonography and uterine artery Doppler in diagnosing endometrial pathologies and carcinoma in postmenopausal bleeding. Arch Gynecol Obstet. 2003; 268:175–80.
Article22. Aboul-Fotouh ME-M, Mosbeh MH, El-Gebaly AF, Mohammed AN. Transvaginal power Doppler sonography can discriminate between benign and malignant endometrial conditions in women with postmenopausal bleeding. Middle East Fertil Soc J. 2012; 17:22–9.
Article23. Li Z, Li L. Risk of malignancies among asymptomatic postmenopausal women with thickened endometrium: a cohort study. Medicine (Baltimore). 2019; 98:e14464.24. Ahmed S, Ahmed RMR, Rania MZ. Study of endometrial volume and vascularity by 3D power doppler ultrasound in women with perimenopausal bleeding. Invest Gynecol Res Women’s Health. 2017; 1:15–22.25. AbdelMaboud NM, Elsaid HH. Role of transvaginal ultrasonography and colour Doppler in the evaluation of postmenopausal bleeding. EJRNM. 2015; 46:235–43.
Article26. Ferrazzi E, Torri V, Trio D, Zannoni E, Filiberto S, Dordoni D. Sonographic endometrial thickness: a useful test to predict atrophy in patients with postmenopausal bleeding. An Italian multicenter study. Ultrasound Obstet Gynecol. 1996; 7:315–21.
Article27. Bano I, Nishat Akhtar, Mittal G, Arshad Z, Khalid M. A study of endometrial pathology by transvaginal color doppler ultrasonography and its correlation with histopathology in post-menopausal women. Indian Medical Gazette. 2013; 147:134–139.28. Arslan M, Erdem A, Erdem M, Yazici G, Himmetoglu O, Gursoy R. Transvaginal color Doppler ultrasonography for prediction of pre-cancerous endometrial lesions. Int J Gynaecol Obstet. 2003; 80:299–306.
Article29. Sladkevicius P, Valentin L, Marsál K. Endometrial thickness and Doppler velocimetry of the uterine arteries as discriminators of endometrial status in women with postmenopausal bleeding: a comparative study. Am J Obstet Gynecol. 1994; 171:722–8.30. Park YR, Lee SW, Kim Y, Bae IY, Kim HK, Choe J, et al. Endometrial thickness cut-off value by transvaginal ultrasonography for screening of endometrial pathology in premenopausal and postmenopausal women. Obstet Gynecol Sci. 2019; 62:445–53.
Article31. ACOG Committee Opinion No. 734: the role of transvaginal ultrasonography in evaluating the endometrium of women with postmenopausal bleeding. Obstet Gynecol. 2018; 131:e124–9.32. Breijer MC, Timmermans A, van Doorn HC, Mol BW, Opmeer BC. Diagnostic strategies for postmenopausal bleeding. Obstet Gynecol Int. 2010; 2010:850812.
Article33. Choudhary S, Ahmad SN, Agarwal S. To compare transvaginal ultrasound colour Doppler (TUCD) with hysteroscopy and guided endometrial biopsy in diagnosing abnormal uterine bleeding. Int J Reprod Contracept Obstet Gynecol. 2017; 6:3035–40.
Article34. Fakhr I, Hasheesh N, Marzouk A, Abou-Salem N, Tabakh S. The impact of two & three dimensions transvaginal ultrasonography and color Doppler on the surgical management of endometrial carcinoma. Kasr El Aini Journal of Surgery. 2009; 10:57–68.35. Razik MA, Walid A, Maksoud MA. Transvaginal and color doppler ultrasound assessment of endometrial pathology in patients with postmenopausal bleeding. J Egypt Soc Gynaecol Obstet. 2012; 38:709–14.36. De Smet F, De Brabanter J, Van den Bosch T, Pochet N, Amant F, Van Holsbeke C, et al. New models to predict depth of infltration in endometrial carcinoma based on transvaginal sonography. Ultrasound Obstet Gynecol. 2006; 27:664–71.
Article37. Bezircioglu I, Baloglu A, Cetinkaya B, Yigit S, Oziz E. The diagnostic value of the Doppler ultrasonography in distinguishing the endometrial malignancies in women with postmenopausal bleeding. Arch Gynecol Obstet. 2012; 285:1369–74.
Article38. Yilmaz Baran Ş, Alemdaroğlu S, Doğan Durdağ G, Yüksel Şimşek S, Bolat F, Köse F, et al. What is the predictive value of preoperative CA 125 level on the survival rate of type 1 endometrial cancer? Turk J Med Sci. 2021; 51:335–41.
Article39. Quan Q, Liao Q, Yin W, Zhou S, Gong S, Mu X. Serum HE4 and CA125 combined to predict and monitor recurrence of type II endometrial carcinoma. Sci Rep. 2021; 11:21694.
Article40. Jiang T, Huang L, Zhang S. Preoperative serum CA125: a useful marker for surgical management of endometrial cancer. BMC Cancer. 2015; 15:396.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Usefulness of Vaginal Sonography in Evaluation of Endometrium in Postmenopausal Women
- The Correlation between the Endometrial Cancer and Postmenopausal Uterine Bleeding
- The diagnostic role of hysteroscopy in postmenopausal bleeding
- Risk Factors Associated with Endometrial Pathology in Premenopausal Breast Cancer Patients Treated with Tamoxifen
- The Change of Endometrial Thickness in Tamoxifen-treated Postmenopausal Breast Cancer Patients