J Cerebrovasc Endovasc Neurosurg.
2022 Sep;24(3):221-231. 10.7461/jcen.2022.E2021.10.003.
Prognostic significance of platelet-to-lymphocyte and platelet-to-neutrophil ratios in patients with mechanical thrombectomy for acute ischemic stroke
- Affiliations
-
- 1Department of Neurosurgery, Soonchunhyang University Bucheon Hospital, Bucheon, Korea
- 2Department of Neurosurgery, St. Vincent’s Hospital, the Catholic University of Korea, Seoul, Korea
- KMID: 2533673
- DOI: http://doi.org/10.7461/jcen.2022.E2021.10.003
Abstract
Objective
The present study aimed to analyze the correlation between platelet-to-lymphocyte ratio (PLR) and platelet-to-neutrophil ratio (PNR) with prognosis of patients who underwent mechanical thrombectomy (MT).
Methods
A total of 432 patients was included, PLR and PNR were calculated from laboratory data on admission. Prognosis was evaluated with a modified Rankin Scale at 3 months after MT. Using receiver operating characteristic (ROC) analysis, optimal cutoff values of PLR and PNR were identified to predict the prognosis after MT. Multivariate analyses were performed to identify the relationship of PLR and PLR with prognosis of MT.
Results
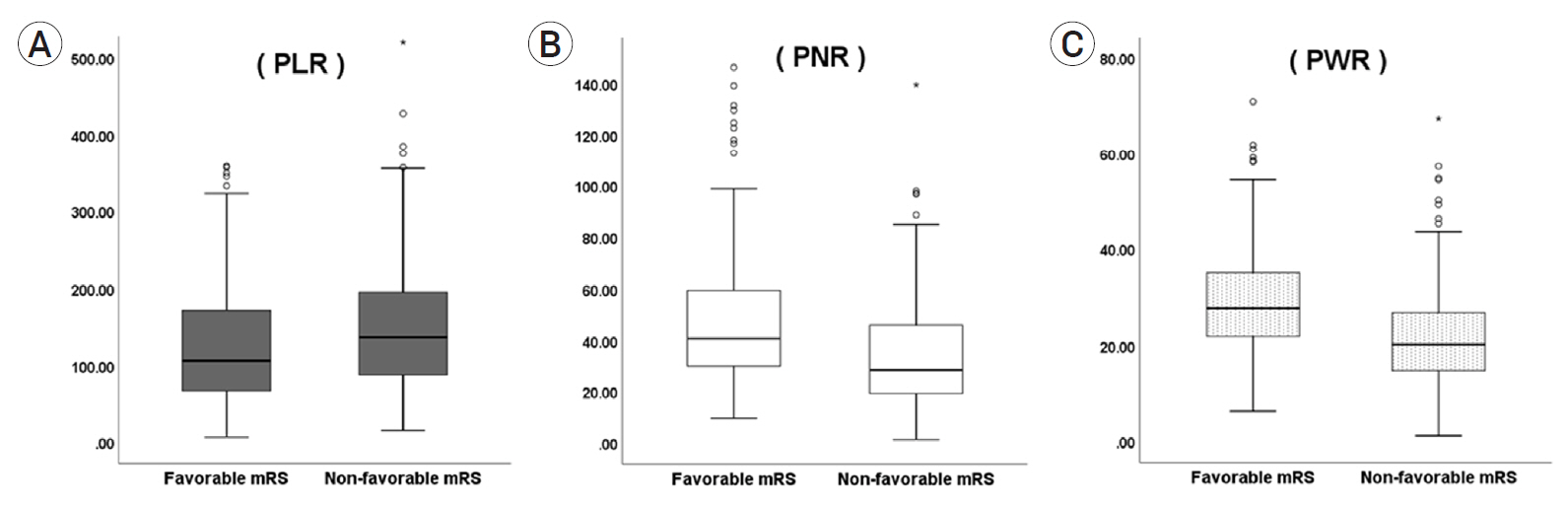
Patients with favorable outcomes had a lower mean PLR (135.0, standard deviation [SD] 120.3) with a higher mean PNR (47.1 [SD] 24.6) compared with patients with unfavorable outcomes (167.6 [SD] 139.3 and 35.4 [SD] 22.4) (p<0.001 and <0.001, respectively). In ROC analyses, the optimal cutoff value of PLR and PNR to predict the 3 months prognosis were 145 and 41, respectively (p=<0.001 and p=0.006). In multivariate analysis, PLR less than 145 (odds ratio [OR] 1.29, 95% confidence interval [CI] 1.06–2.06; p=0.016) and PNR greater than 41 (OR 1.22, 95% CI 1.10–1.62; p=0.022) were predictors of favorable outcome at 3 months.
Conclusions
In patients with MT, PLR and PNR on admission could be predictive factors of prognosis and mortality at 3 months. Decreased PLR and increased PNR were associated with favorable clinical outcome 3 months after MT.
Keyword
Figure
Reference
-
1. Altintas O, Altintas MO, Tasal A, Kucukdagli OT, Asil T. The relationship of platelet-to-lymphocyte ratio with clinical outcome and final infarct core in acute ischemic stroke patients who have undergone endovascular therapy. Neurol Res. 2016; Sep. 38(9):759–65.
Article2. Amarenco P, Bogousslavsky J, Caplan LR, Donnan GA, Hennerici MG. Classification of stroke subtypes. Cerebrovasc Dis. 2009; 27(5):493–501.
Article3. Buck BH, Liebeskind DS, Saver JL, Bang OY, Yun SW, Starkman S, et al. Early neutrophilia is associated with volume of ischemic tissue in acute stroke. Stroke. 2008; Feb. 39(2):355–60.
Article4. Chen Z, Huang Y, Li S, Lin J, Liu W, Ding Z, et al. Platelet-to-white blood cell ratio: a prognostic predictor for 90-day outcomes in ischemic stroke patients with intravenous thrombolysis. J Stroke Cerebrovasc Dis. 2016; Oct. 25(10):2430–8.
Article5. Deser SB, Yucel SM, Demirag MK, Guclu MM, Kolbakir F, Keceligil HT. The association between platelet/lymphocyte ratio, neutrophil/lymphocyte ratio, and carotid artery stenosis and stroke following carotid endarterectomy. Vascular. 2019; Dec. 27(6):604–11.
Article6. Deshaies EM. Tri-axial system using the Solitaire-FR and Penumbra Aspiration Microcatheter for acute mechanical thrombectomy. J Clin Neurosci. 2013; Sep. 20(9):1303–5.
Article7. Duan Z, Wang H, Wang Z, Hao Y, Zi W, Yang D, et al. Neutrophil-lymphocyte ratio predicts functional and safety outcomes after endovascular treatment for acute ischemic stroke. Cerebrovasc Dis. 2018; 45(5-6):221–7.
Article8. Franks ZG, Campbell RA, Weyrich AS, Rondina MT. Platelet-leukocyte interactions link inflammatory and thromboembolic events in ischemic stroke. Ann N Y Acad Sci. 2010; Oct. 1207:11–7.
Article9. GBD 2015 Chronic Respiratory Disease Collaborators. Global, regional, and national deaths, prevalence, disability-adjusted life years, and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Respir Med. 2017; Sep. 5(9):691–706.10. Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016; Apr. 387(10029):1723–31.
Article11. Grau AJ, Boddy AW, Dukovic DA, Buggle F, Lichy C, Brandt T, et al. Leukocyte count as an independent predictor of recurrent ischemic events. Stroke. 2004; May. 35(5):1147–52.
Article12. Hacke W, Donnan G, Fieschi C, Kaste M, von Kummer R, Broderick JP, et al. Association of outcome with early stroke treatment: pooled analysis of ATLANTIS, ECASS, and NINDS rt-PA stroke trials. Lancet. 2004; Mar. 363(9411):768–74.
Article13. Hacke W, Kaste M, Bluhmki E, Brozman M, Davalos A, Guidetti D. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008; Sep. 359(13):1317–29.
Article14. Herz J, Sabellek P, Lane TE, Gunzer M, Hermann DM, Doeppner TR. Role of neutrophils in exacerbation of brain injury after focal cerebral ischemia in hyperlipidemic mice. Stroke. 2015; Oct. 46(10):2916–25.
Article15. Horne BD, Anderson JL, John JM, Weaver A, Bair TL, Jensen KR, et al. Which white blood cell subtypes predict increased cardiovascular risk? J Am Coll Cardiol. 2005; May. 45(10):1638–43.
Article16. Huo Y, Ley KF. Role of platelets in the development of atherosclerosis. Trends Cardiovasc Med. 2004; Jan. 14(1):18–22.
Article17. Idil Soylu A, Arikan Cortcu S, Uzunkaya F, Atalay YO, Bekci T, Gungor L, et al. The correlation of the platelet-to-lymphocyte ratio with the severity of stenosis and stroke in patients with carotid arterial disease. Vascular. 2017; Jun. 25(3):299–306.
Article18. Ishikawa T, Shimizu M, Kohara S, Takizawa S, Kitagawa Y, Takagi S. Appearance of WBC-platelet complex in acute ischemic stroke, predominantly in atherothrombotic infarction. J Atheroscler Thromb. 2012; 19(5):494–501.
Article19. Jennings LK. Mechanisms of platelet activation: need for new strategies to protect against platelet-mediated atherothrombosis. Thromb Haemost. 2009; Aug. 102(2):248–57.
Article20. Jin P, Li X, Chen J, Zhang Z, Hu W, Chen L, et al. Platelet-to-neutrophil ratio is a prognostic marker for 90-days outcome in acute ischemic stroke. J Clin Neurosci. 2019; May. 63:110–5.
Article21. Kaplan ZS, Jackson SP. The role of platelets in atherothrombosis. Hematology Am Soc Hematol Educ Program. 2011; 2011:51–61.
Article22. Kim JY, Park J, Chang JY, Kim SH, Lee JE. Inflammation after ischemic stroke: the role of leukocytes and glial cells. Exp Neurobiol. 2016; Oct. 25(5):241–51.
Article23. Krenn-Pilko S, Langsenlehner U, Thurner EM, Stojakovic T, Pichler M, Gerger A, et al. The elevated preoperative platelet-to-lymphocyte ratio predicts poor prognosis in breast cancer patients. Br J Cancer. 2014; May. 110(10):2524–30.
Article24. Kurtul A, Ornek E. Platelet to lymphocyte ratio in cardiovascular diseases: a systematic review. Angiology. 2019; Oct. 70(9):802–18.
Article25. Langer HF, Gawaz M. Platelet-vessel wall interactions in atherosclerotic disease. Thromb Haemost. 2008; Mar. 99(3):480–6.
Article26. Lopez HV, Vivas MF, Ruiz RN, Martinez JR, Navaridas BG, Villa MG, et al. Association between post-procedural hyperoxia and poor functional outcome after mechanical thrombectomy for ischemic stroke: an observational study. Ann Intensive Care. 2019; May. 9(1):59.27. Marquardt L, Anders C, Buggle F, Palm F, Hellstern P, Grau AJ. Leukocyte-platelet aggregates in acute and subacute ischemic stroke. Cerebrovasc Dis. 2009; 28(3):276–82.
Article28. Maus V, Brehm A, Tsogkas I, Henkel S, Psychogios MN. Stent retriever placement in embolectomy: the choice of the post-bifurcational trunk influences the first-pass reperfusion result in M1 occlusions. J Neurointerv Surg. 2019; Mar. 11(3):237–40.
Article29. Oh SW, Yi HJ, Lee DH, Sung JH. Prognostic significance of various inflammation based scores in patients with mechanical thrombectomy for acute ischemic stroke. World Neurosurg. 2020; Sep. 141:e710–717.30. Otxoa-de-Amezaga A, Gallizioli M, Pedragosa J, Justicia C, Miro-Mur F, Salas-Perdomo A, et al. Location of neutrophils in different compartments of the damaged mouse brain after severe ischemia/reperfusion. Stroke. 2019; Jun. 50(6):1548–57.
Article31. Perez-de-Puig I, Miro-Mur F, Ferrer-Ferrer M, Gelpi E, Pedragosa J, Justicia C, et al. Neutrophil recruitment to the brain in mouse and human ischemic stroke. Acta Neuropathol. 2015; Feb. 129(2):239–57.
Article32. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019; Dec. 50(12):e344–418.
Article33. Qin B, Ma N, Tang Q, Wei T, Yang M, Fu H, et al. Neutrophil to lymphocyte ratio (NLR) and platelet to lymphocyte ratio (PLR) were useful markers in assessment of inflammatory response and disease activity in SLE patients. Mod Rheumatol. 2016; 26(3):372–6.
Article34. Ringer AJ, Guterman LR, Hopkins LN. Site-specific thromboembolism: a novel animal model for stroke. AJNR Am J Neuroradiol. 2004; Feb. 25(2):329–32.35. Rudilosso S, Laredo C, Amaro S, Renu A, Llull L, Obach V, et al. Clinical improvement within 24 hours from mechanical thrombectomy as a predictor of long-term functional outcome in a multicenter population-based cohort of patients with ischemic stroke. J Neurointerv Surg. 2021; Feb. 13(2):119–23.
Article36. Tao C, Wang J, Hu X, Ma J, Li H, You C. Clinical value of neutrophil to lymphocyte and platelet to lymphocyte ratio after aneurysmal subarachnoid hemorrhage. Neurocrit Care. 2017; Jun. 26(3):393–401.
Article37. Walsh TG, Metharom P, Berndt MC. The functional role of platelets in the regulation of angiogenesis. Platelets. 2015; 26(3):199–211.
Article38. Wirtz MM, Hendrix P, Goren O, Beckett LA, Dicristina HR, Schirmer CM, et al. Predictor of 90-day functional outcome after mechanical thrombectomy for large vessel occlusion stroke: NIHSS score of 10 or less at 24 hours. J Neurosurg. 2019; Dec. 1–7.
Article39. Zaidat OO, Yoo AJ, Khatri P, Tomsick TA, von Kummer R, Saver JL, et al. Recommendations on angiographic revascularization grading standards for acute ischemic stroke: a consensus statement. Stroke. 2013; Sep. 44(9):2650–63.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Acute Ischemic Stroke Associated with Essential Thrombocythemia and Suspected Platelet Aggregation in Intracranial Artery
- Mean Platelet Component Change according to Stage in Stroke Patients
- A Case of Platelet Satellitism with Platelet Phagocytosis by Neutrophils and Platelet-neutrophil Agglutination
- The Change of Platelet Aggregation with Acute Ischemic Stroke
- Forced Arterial Suction Thrombectomy Using Distal Access Catheter in Acute Ischemic Stroke