Diabetes Metab J.
2022 Sep;46(5):677-688. 10.4093/dmj.2021.0202.
Differentiation of Microencapsulated Neonatal Porcine Pancreatic Cell Clusters in Vitro Improves Transplant Efficacy in Type 1 Diabetes Mellitus Mice
- Affiliations
-
- 1Department of Endocrinology and Metabolism, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Biomedicine & Health Sciences, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 3Division of Intractable Diseases, Department of Chronic Diseases Convergence Research, Korea National Institute of Health, Cheongju, Korea
- 4Recombinant Protein Products Division, National Institute of Food and Drug Safety Evaluation, Ministry of Food and Drug Safety, Cheongju, Korea
- KMID: 2533637
- DOI: http://doi.org/10.4093/dmj.2021.0202
Abstract
- Background
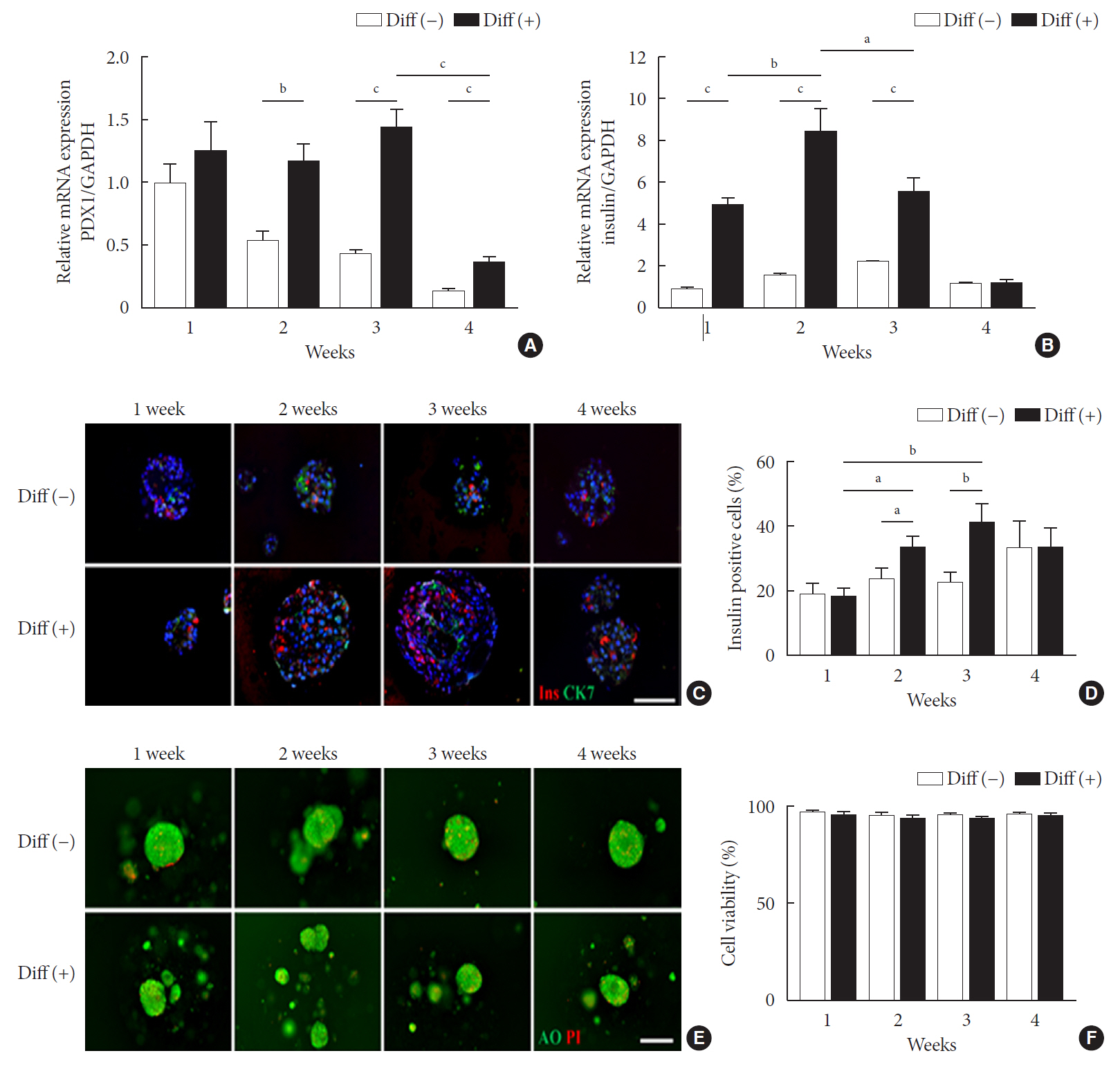
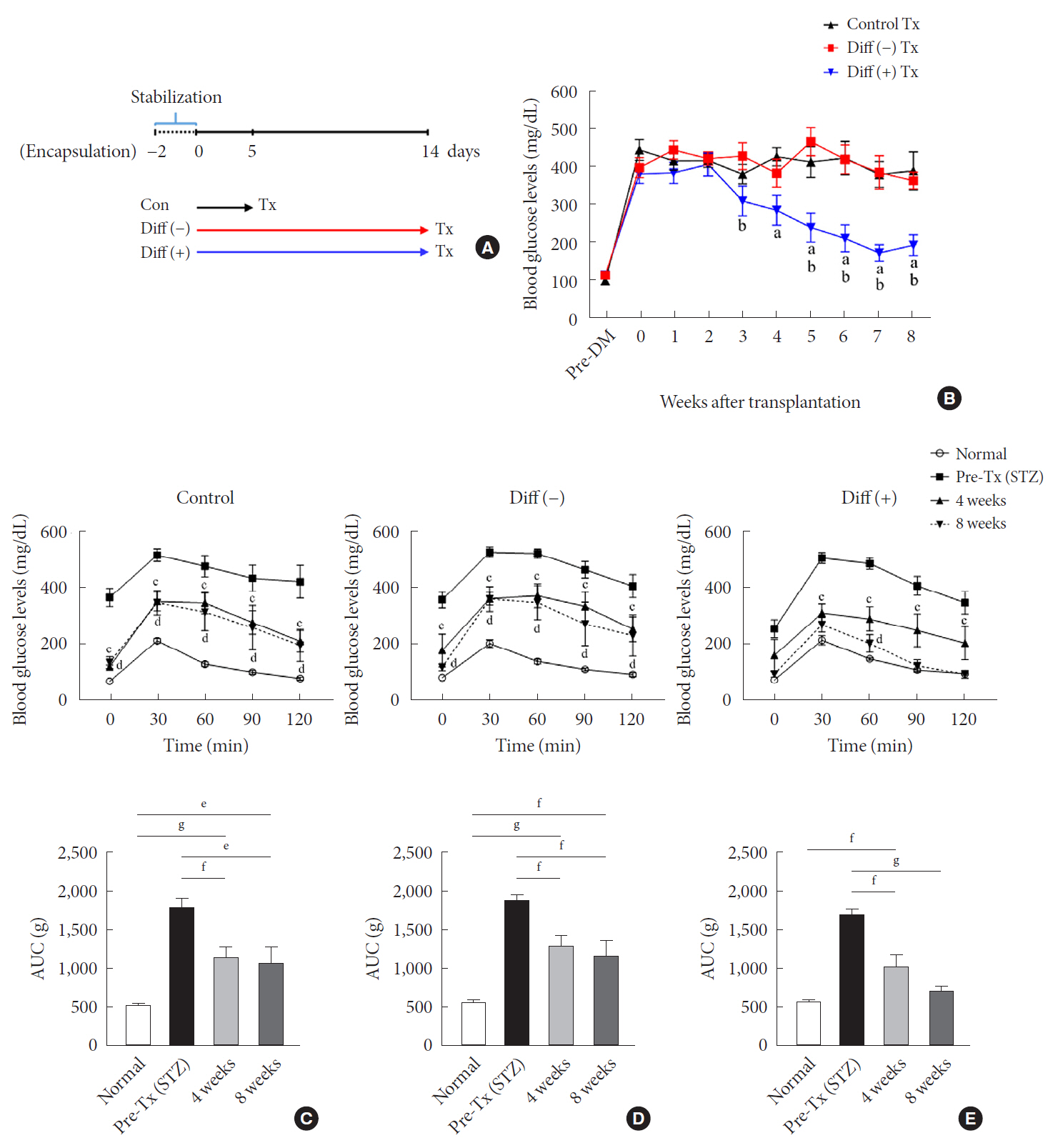
Neonatal porcine pancreatic cell clusters (NPCCs) have been proposed as an alternative source of β cells for islet transplantation because of their low cost and growth potential after transplantation. However, the delayed glucose lowering effect due to the immaturity of NPCCs and immunologic rejection remain as a barrier to NPCC’s clinical application. Here, we demonstrate accelerated differentiation and immune-tolerant NPCCs by in vitro chemical treatment and microencapsulation.
Methods
NPCCs isolated from 3-day-old piglets were cultured in F-10 media and then microencapsulated with alginate on day 5. Differentiation of NPCCs is facilitated by media supplemented with activin receptor-like kinase 5 inhibitor II, triiodothyronine and exendin-4 for 2 weeks. Marginal number of microencapsulated NPCCs to cure diabetes with and without differentiation were transplanted into diabetic mice and observed for 8 weeks.
Results
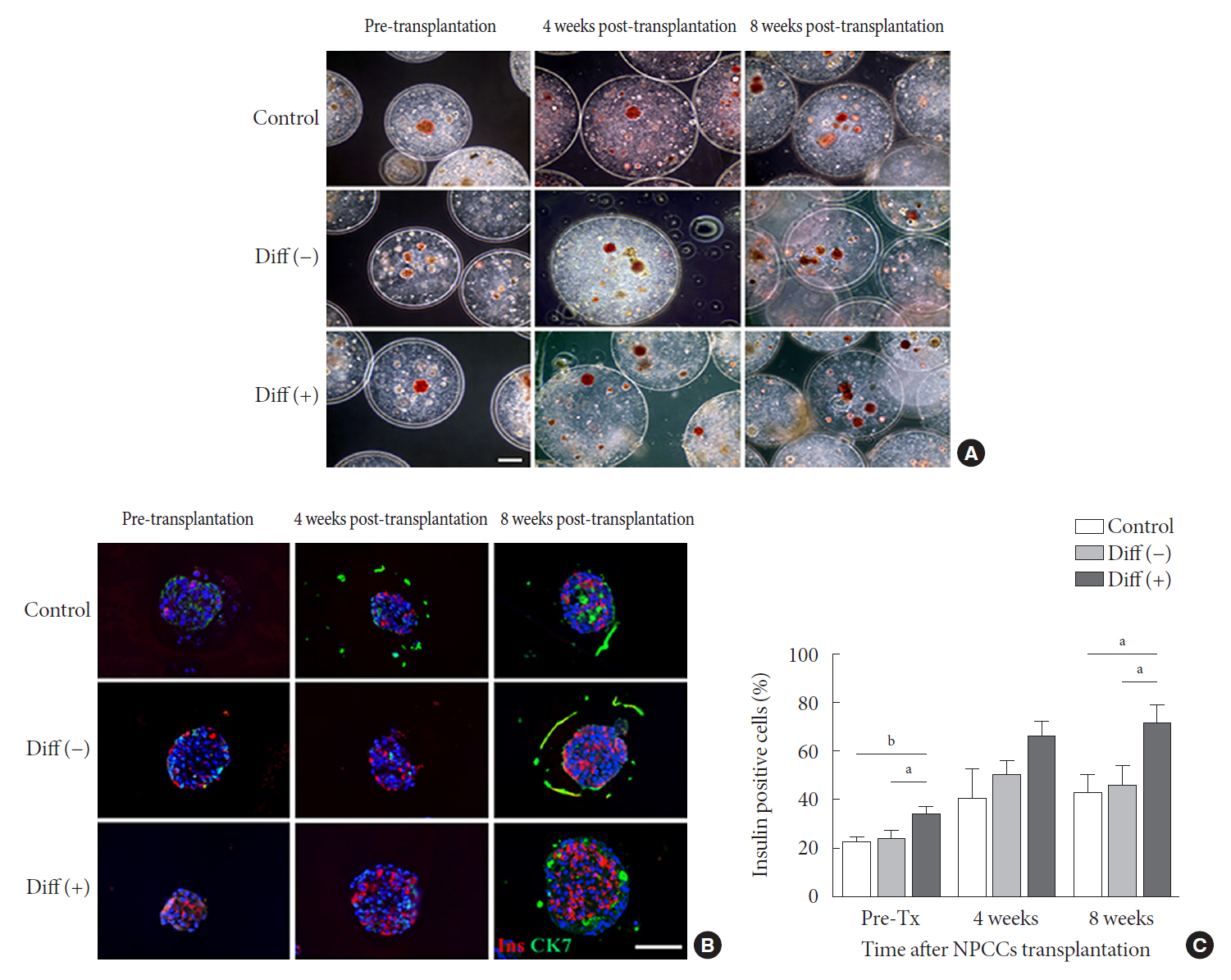
The proportion of insulin-positive cells and insulin mRNA levels of NPCCs were significantly increased in vitro in the differentiated group compared with the undifferentiated group. Blood glucose levels decreased eventually after transplantation of microencapsulated NPCCs in diabetic mice and normalized after 7 weeks in the differentiated group. In addition, the differentiated group showed nearly normal glucose tolerance at 8 weeks after transplantation. In contrast, neither blood glucose levels nor glucose tolerance were improved in the undifferentiated group. Retrieved graft in the differentiated group showed greater insulin response to high glucose compared with the undifferentiated group.
Conclusion
in vitro differentiation of microencapsulated immature NPCCs increased the proportion of insulin-positive cells and improved transplant efficacy in diabetic mice without immune rejection.
Keyword
Figure
Reference
-
1. Senior PA, Pettus JH. Stem cell therapies for type 1 diabetes: current status and proposed road map to guide successful clinical trials. Diabet Med. 2019; 36:297–307.
Article2. Cryer PE. Mechanisms of hypoglycemia-associated autonomic failure in diabetes. N Engl J Med. 2013; 369:362–72.
Article3. Bellin MD, Dunn TB. Transplant strategies for type 1 diabetes: whole pancreas, islet and porcine beta cell therapies. Diabetologia. 2020; 63:2049–56.
Article4. Ellis C, Lyon JG, Korbutt GS. Optimization and scale-up isolation and culture of neonatal porcine islets: potential for clinical application. Cell Transplant. 2016; 25:539–47.
Article5. Elliott RB, Escobar L, Tan PL, Muzina M, Zwain S, Buchanan C. Live encapsulated porcine islets from a type 1 diabetic patient 9.5 yr after xenotransplantation. Xenotransplantation. 2007; 14:157–61.6. Korbutt GS, Elliott JF, Ao Z, Smith DK, Warnock GL, Rajotte RV. Large scale isolation, growth, and function of porcine neonatal islet cells. J Clin Invest. 1996; 97:2119–29.
Article7. Dufrane D, Gianello P. Pig islets for clinical islet xenotransplantation. Curr Opin Nephrol Hypertens. 2009; 18:495–500.
Article8. Kuppan P, Seeberger K, Kelly S, Rosko M, Adesida A, Pepper AR, et al. Co-transplantation of human adipose-derived mesenchymal stem cells with neonatal porcine islets within a prevascularized subcutaneous space augments the xenograft function. Xenotransplantation. 2020; 27:e12581.
Article9. Hayward JA, Ellis CE, Seeberger K, Lee T, Salama B, Mulet-Sierra A, et al. Cotransplantation of mesenchymal stem cells with neonatal porcine islets improve graft function in diabetic mice. Diabetes. 2017; 66:1312–21.
Article10. Hassouna T, Seeberger KL, Salama B, Korbutt GS. Functional maturation and in vitro differentiation of neonatal porcine islet grafts. Transplantation. 2018; 102:e413–23.
Article11. van der Windt DJ, Bottino R, Kumar G, Wijkstrom M, Hara H, Ezzelarab M, et al. Clinical islet xenotransplantation: how close are we? Diabetes. 2012; 61:3046–55.12. Zhang N, Su D, Qu S, Tse T, Bottino R, Balamurugan AN, et al. Sirolimus is associated with reduced islet engraftment and impaired beta-cell function. Diabetes. 2006; 55:2429–36.13. Sun CL, Ham DS, Park HS, Kim JW, Cho JH, Song KH, et al. Rapamycin suppresses the expansion and differentiation of porcine neonatal pancreas cell clusters. Transplantation. 2010; 90:717–24.
Article14. Yang HK, Ham DS, Park HS, Rhee M, You YH, Kim MJ, et al. Long-term efficacy and biocompatibility of encapsulated islet transplantation with chitosan-coated alginate capsules in mice and canine models of diabetes. Transplantation. 2016; 100:334–43.
Article15. Yoon KH, Quickel RR, Tatarkiewicz K, Ulrich TR, HollisterLock J, Trivedi N, et al. Differentiation and expansion of beta cell mass in porcine neonatal pancreatic cell clusters transplanted into nude mice. Cell Transplant. 1999; 8:673–89.
Article16. Park HS, Ham DS, You YH, Shin J, Kim JW, Jo JH, et al. Successful xenogenic islet transplantation with Ba2+-alginate encapsulation. Tissue Eng Regen Med. 2010; 7:523–30.17. Nagaya M, Hayashi A, Nakano K, Honda M, Hasegawa K, Okamoto K, et al. Distributions of endocrine cell clusters during porcine pancreatic development. PLoS One. 2019; 14:e0216254.
Article18. Kim S, Whitener RL, Peiris H, Gu X, Chang CA, Lam JY, et al. Molecular and genetic regulation of pig pancreatic islet cell development. Development. 2020; 147:dev186213.
Article19. Trivedi N, Hollister-Lock J, Lopez-Avalos MD, O’Neil JJ, Keegan M, Bonner-Weir S, et al. Increase in beta-cell mass in transplanted porcine neonatal pancreatic cell clusters is due to proliferation of beta-cells and differentiation of duct cells. Endocrinology. 2001; 142:2115–22.20. Lopez-Avalos MD, Tatarkiewicz K, Sharma A, Bonner-Weir S, Weir GC. Enhanced maturation of porcine neonatal pancreatic cell clusters with growth factors fails to improve transplantation outcome. Transplantation. 2001; 71:1154–62.
Article21. Luca G, Nastruzzi C, Calvitti M, Becchetti E, Baroni T, Neri LM, et al. Accelerated functional maturation of isolated neonatal porcine cell clusters: in vitro and in vivo results in NOD mice. Cell Transplant. 2005; 14:249–61.
Article22. Lau H, Corrales N, Alexander M, Mohammadi MR, Li S, Smink AM, et al. Necrostatin-1 supplementation enhances young porcine islet maturation and in vitro function. Xenotransplantation. 2020; 27:e12555.
Article23. Blum B, Roose AN, Barrandon O, Maehr R, Arvanites AC, Davidow LS, et al. Reversal of β cell de-differentiation by a small molecule inhibitor of the TGFβ pathway. Elife. 2014; 3:e02809.
Article24. Aguayo-Mazzucato C, Zavacki AM, Marinelarena A, HollisterLock J, El Khattabi I, Marsili A, et al. Thyroid hormone promotes postnatal rat pancreatic β-cell development and glucoseresponsive insulin secretion through MAFA. Diabetes. 2013; 62:1569–80.25. Rezania A, Bruin JE, Arora P, Rubin A, Batushansky I, Asadi A, et al. Reversal of diabetes with insulin-producing cells derived in vitro from human pluripotent stem cells. Nat Biotechnol. 2014; 32:1121–33.
Article26. Pagliuca FW, Millman JR, Gurtler M, Segel M, Van Dervort A, Ryu JH, et al. Generation of functional human pancreatic β cells in vitro. Cell. 2014; 159:428–39.
Article27. Xu G, Stoffers DA, Habener JF, Bonner-Weir S. Exendin-4 stimulates both beta-cell replication and neogenesis, resulting in increased beta-cell mass and improved glucose tolerance in diabetic rats. Diabetes. 1999; 48:2270–6.
Article28. Buteau J, Foisy S, Joly E, Prentki M. Glucagon-like peptide 1 induces pancreatic beta-cell proliferation via transactivation of the epidermal growth factor receptor. Diabetes. 2003; 52:124–32.29. Lau H, Corrales N, Lee S, Heng J, Zhang K, Alexander M, et al. Exendin-4 improves yield and function of isolated pre-weaned porcine islets. J Endocrinol Diabetes. 2018; 5:1–7.30. Zhang J, Liu F. The de-, re-, and trans-differentiation of β-cells: regulation and function. Semin Cell Dev Biol. 2020; 103:68–75.
Article31. Montanari E, Szabo L, Balaphas A, Meyer J, Perriraz-Mayer N, Pimenta J, et al. Multipotent mesenchymal stromal cells derived from porcine exocrine pancreas improve insulin secretion from juvenile porcine islet cell clusters. Xenotransplantation. 2021; 28:e12666.
Article32. Miyagawa S. Xenotransplantation: comprehensive study. London: IntechOpen;2020. Chapter 3, Porcine islet cell xenotransplantation [cited 2021 Dec 5]. Available from: https://www.intechopen.com/chapters/70850.33. Gazda LS, Vinerean HV, Laramore MA, Diehl CH, Hall RD, Rubin AL, et al. Encapsulation of porcine islets permits extended culture time and insulin independence in spontaneously diabetic BB rats. Cell Transplant. 2007; 16:609–20.
Article34. Omer A, Duvivier-Kali VF, Trivedi N, Wilmot K, Bonner-Weir S, Weir GC. Survival and maturation of microencapsulated porcine neonatal pancreatic cell clusters transplanted into immunocompetent diabetic mice. Diabetes. 2003; 52:69–75.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Repeated Gene Transfection Impairs the Engraftment of Transplanted Porcine Neonatal Pancreatic Cells
- Adenoviruses Expressing PDX-1, BETA2/NeuroD and MafA Induces the Transdifferentiation of Porcine Neonatal Pancreas Cell Clusters and Adult Pig Pancreatic Cells into Beta-Cells
- Expression of Gal alpha1,3 Gal Antigen and Galactosyl Transferase mRNA in Porcine Neonatal Pancreatic Tissue
- In Vitro Expansion and Differentiation of Islet Precursor Cells from Cultured Neonatal Porcine Pancreatic Tissue
- Pancreas transplant in type 1 diabetes mellitus: the emerging role of islet cell transplant