Korean J Orthod.
2022 Sep;52(5):324-333. 10.4041/kjod21.280.
Common dental anomalies in Korean orthodontic patients: An update
- Affiliations
-
- 1Department of Orthodontics, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Graduate School of Clinical Dental Science, The Catholic University of Korea, Seoul, Korea
- KMID: 2533257
- DOI: http://doi.org/10.4041/kjod21.280
Abstract
Objective
The aim of this study was 1) to investigate the prevalence and pattern of dental anomalies (DAs), 2) to compare DAs according to the type of malocclusion, and 3) to investigate the correlation between tooth impaction and other DAs in the Korean orthodontic population.
Methods
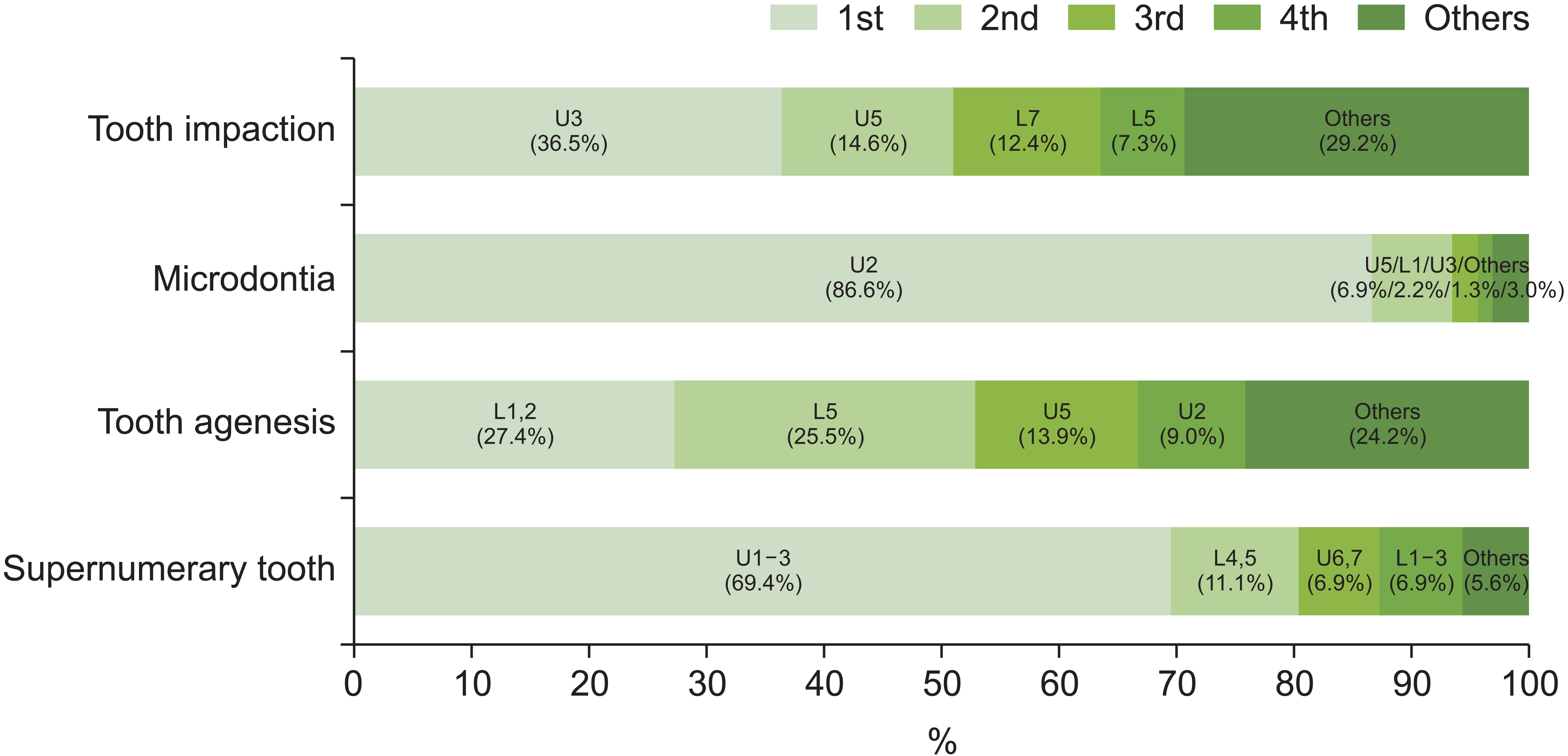
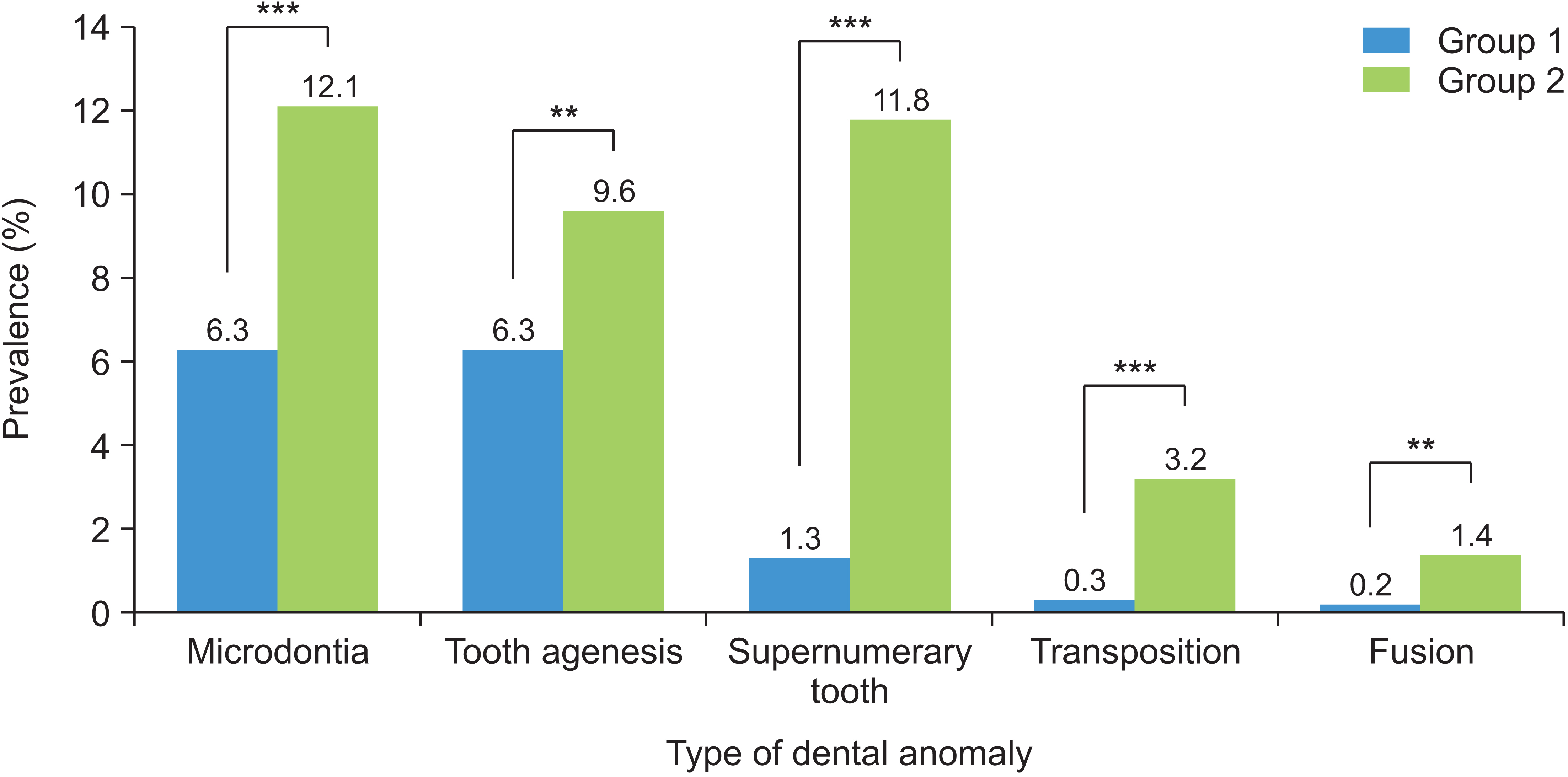
A total of 3,240 orthodontic patients were classified as Class I, Class II, or Class III malocclusion groups. The presence and location of common DAs, including impaction, microdontia, agenesis, supernumerary tooth, transposition, and fusion, were identified by examining diagnostic records. Furthermore, samples were classified as Group 1 without impaction or Group 2 with impaction. The prevalence of other DAs concurrent with impaction was investigated and compared to Group 1.
Results
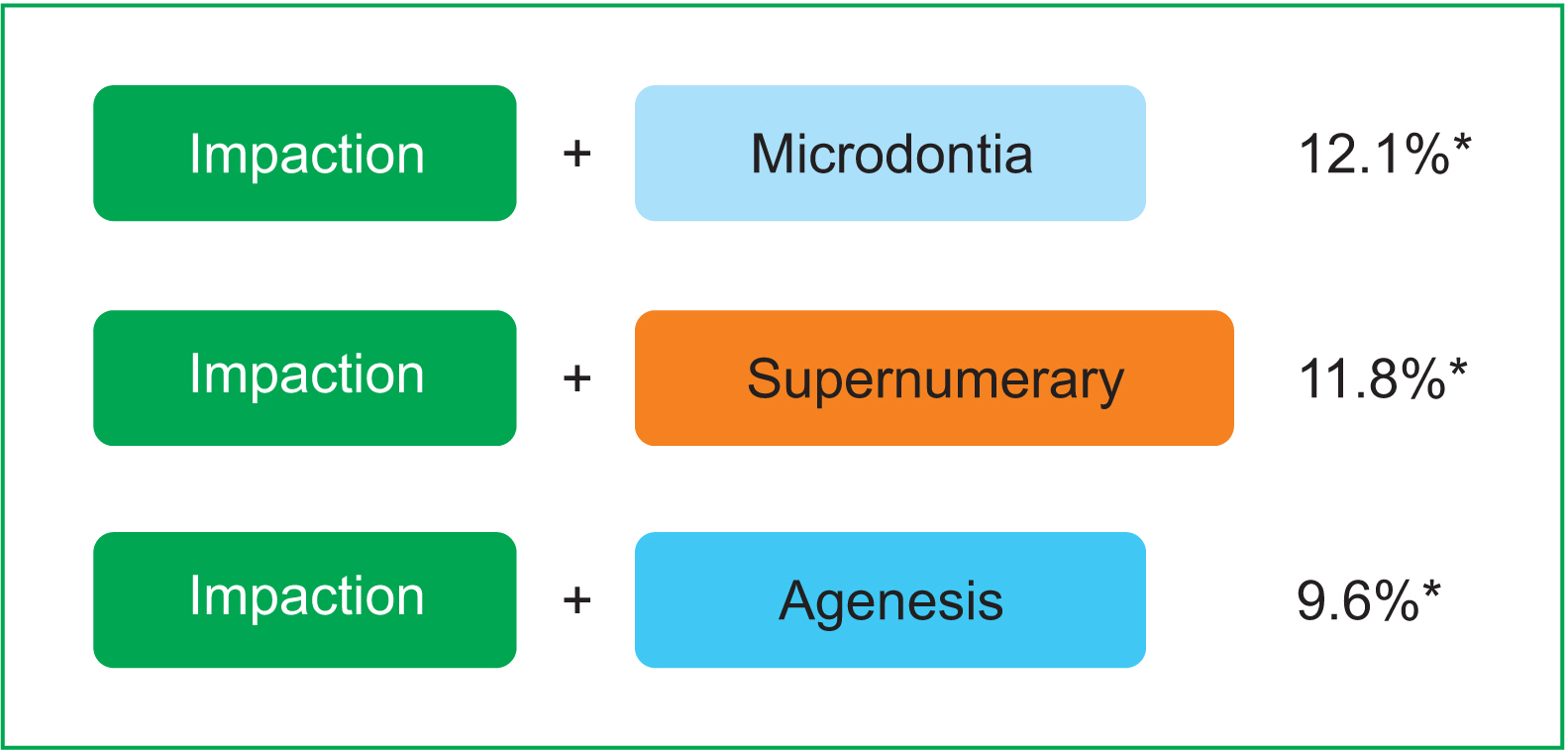
Impaction was the most prevalent DA, followed by microdontia, agenesis, and supernumerary. Class I and Class III groups showed the same order of prevalence, but agenesis was more frequent than microdontia in the Class II group. The prevalence of the four DAs was lowest in the Class III group. Overall, 8.6% of patients were classified into Group 2. The incidence of DAs other than impaction and the prevalence of multiple concurrent DAs were significantly higher in Group 2. Impaction showed a significant relationship with supernumerary tooth, transposition, and fusion.
Conclusions
The prevalence and pattern of DAs varied depending on the type of malocclusion. As there was a higher risk of other DAs in patients with impacted teeth, early detection of the impacted tooth and a detailed diagnosis of other possible DAs may be essential.
Figure
Reference
-
1. Brook AH. 2009; Multilevel complex interactions between genetic, epigenetic and environmental factors in the aetiology of anomalies of dental development. Arch Oral Biol. 54(Suppl 1):S3–17. DOI: 10.1016/j.archoralbio.2009.09.005. PMID: 19913215. PMCID: PMC2981858. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=71549118817&origin=inward.2. Baron C, Houchmand-Cuny M, Enkel B, Lopez-Cazaux S. 2018; Prevalence of dental anomalies in French orthodontic patients: a retrospective study. Arch Pediatr. 25:426–30. DOI: 10.1016/j.arcped.2018.07.002. PMID: 30249487. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85053683621&origin=inward.3. Patil S, Doni B, Kaswan S, Rahman F. 2013; Prevalence of dental anomalies in Indian population. J Clin Exp Dent. 5:e183–6. DOI: 10.4317/jced.51119. PMID: 24455078. PMCID: PMC3892239. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=84885168141&origin=inward.4. Lee JH, Yang BH, Lee SM, Kim YH, Shim HW, Chung HS. 2011; A study on the prevalence of dental anomalies in Korean dental-patients. Korean J Orthod. 41:346–53. DOI: 10.4041/kjod.2011.41.5.346. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=80055057248&origin=inward.5. Guttal KS, Naikmasur VG, Bhargava P, Bathi RJ. 2010; Frequency of developmental dental anomalies in the Indian population. Eur J Dent. 4:263–9. DOI: 10.1055/s-0039-1697838. PMID: 20613914. PMCID: PMC2897859.6. Thongudomporn U, Freer TJ. 1998; Prevalence of dental anomalies in orthodontic patients. Aust Dent J. 43:395–8. PMID: 9973708. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=0032233633&origin=inward.7. Al-Jabaa AH, Aldrees AM. 2013; Prevalence of dental anomalies in Saudi orthodontic patients. J Contemp Dent Pract. 14:724–30. DOI: 10.5005/jp-journals-10024-1391. PMID: 24309355. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=84893407069&origin=inward.8. Laganà G, Venza N, Borzabadi-Farahani A, Fabi F, Danesi C, Cozza P. 2017; Dental anomalies: prevalence and associations between them in a large sample of non-orthodontic subjects, a cross-sectional study. BMC Oral Health. 17:62. DOI: 10.1186/s12903-017-0352-y. PMID: 28284207. PMCID: PMC5346249. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85014841562&origin=inward.9. Altug-Atac AT, Erdem D. 2007; Prevalence and distribution of dental anomalies in orthodontic patients. Am J Orthod Dentofacial Orthop. 131:510–4. DOI: 10.1016/j.ajodo.2005.06.027. PMID: 17418718. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=34047127502&origin=inward.10. Fernandez CCA, Pereira CVCA, Luiz RR, Vieira AR, De Castro Costa M. 2018; Dental anomalies in different growth and skeletal malocclusion patterns. Angle Orthod. 88:195–201. DOI: 10.2319/071917-482.1. PMID: 29215300. PMCID: PMC8312537. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85043574845&origin=inward.11. Basdra EK, Kiokpasoglou MN, Komposch G. 2001; Congenital tooth anomalies and malocclusions: a genetic link? Eur J Orthod. 23:145–51. DOI: 10.1093/ejo/23.2.145. PMID: 11398552. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=0035317373&origin=inward.12. Uslu O, Akcam MO, Evirgen S, Cebeci I. 2009; Prevalence of dental anomalies in various malocclusions. Am J Orthod Dentofacial Orthop. 135:328–35. DOI: 10.1016/j.ajodo.2007.03.030. PMID: 19268831. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=61349115073&origin=inward.13. Dang HQ, Constantine S, Anderson PJ. 2017; The prevalence of dental anomalies in an Australian population. Aust Dent J. 62:161–4. DOI: 10.1111/adj.12443. PMID: 27471093. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85013042356&origin=inward.14. Chung CJ, Han JH, Kim KH. 2008; The pattern and prevalence of hypodontia in Koreans. Oral Dis. 14:620–5. DOI: 10.1111/j.1601-0825.2007.01434.x. PMID: 18248591. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=53149132810&origin=inward.15. Kim YH. 2011; Investigation of hypodontia as clinically related dental anomaly: prevalence and characteristics. ISRN Dent. 2011:246135. DOI: 10.5402/2011/246135. PMID: 21991459. PMCID: PMC3170076.16. Fardi A, Kondylidou-Sidira A, Bachour Z, Parisis N, Tsirlis A. 2011; Incidence of impacted and supernumerary teeth-a radiographic study in a North Greek population. Med Oral Patol Oral Cir Bucal. 16:e56–61. DOI: 10.4317/medoral.16.e56. PMID: 20711166. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=78751662159&origin=inward.17. Baccetti T. 1998; A controlled study of associated dental anomalies. Angle Orthod. 68:267–74. DOI: 10.1043/0003-3219(1998)068<0267:ACSOAD>2.3.CO;2. PMID: 9622764.18. Peck S, Peck L, Kataja M. 1996; Prevalence of tooth agenesis and peg-shaped maxillary lateral incisor associated with palatally displaced canine (PDC) anomaly. Am J Orthod Dentofacial Orthop. 110:441–3. DOI: 10.1016/S0889-5406(96)70048-3. PMID: 8876497. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=0030265939&origin=inward.19. Sigler LM, Baccetti T, McNamara JA Jr. 2011; Effect of rapid maxillary expansion and transpalatal arch treatment associated with deciduous canine extraction on the eruption of palatally displaced canines: a 2-center prospective study. Am J Orthod Dentofacial Orthop. 139:e235–44. DOI: 10.1016/j.ajodo.2009.07.015. PMID: 21392667. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=79952468852&origin=inward.20. Peck S, Peck L, Kataja M. 2002; Concomitant occurrence of canine malposition and tooth agenesis: evidence of orofacial genetic fields. Am J Orthod Dentofacial Orthop. 122:657–60. DOI: 10.1067/mod.2002.129915. PMID: 12490878. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=0036884421&origin=inward.21. Patil S, Maheshwari S. 2014; Prevalence of impacted and supernumerary teeth in the North Indian population. J Clin Exp Dent. 6:e116–20. DOI: 10.4317/jced.51284. PMID: 24790709. PMCID: PMC4002339. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=84909595776&origin=inward.22. Agurto-S P, Nicholson C, del Sol M. 2019; Proposal of anatomical terms for alterations in tooth size: "Microdontia and macrodontia.". Int J Morphol. 37:375–8. DOI: 10.4067/S0717-95022019000100375.23. Al-Ani AH, Antoun JS, Thomson WM, Merriman TR, Farella M. 2017; Hypodontia: an update on its etiology, classification, and clinical management. Biomed Res Int. 2017:9378325. DOI: 10.1155/2017/9378325. PMID: 28401166. PMCID: PMC5376450. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85017171204&origin=inward.24. Tailor M. 2012; Tooth fusion- a rare dental anomaly: analysis of six cases. Int J Oral Maxillofac Pathol. 4:50–3. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=0030265939&origin=inward.25. Schulze C. Gorlin RJ, Goldman HM, editors. 1970. Developmental abnormalities of the teeth and jaws. Thoma's oral pathology. 6th ed. CV Mosby;St Louis: PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=0030265939&origin=inward.26. Silverman NE, Ackerman JL. 1979; Oligodontia: a study of its prevalence and variation in 4032 children. ASDC J Dent Child. 46:470–7. PMID: 290641. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=0018546853&origin=inward.27. Garvey MT, Barry HJ, Blake M. 1999; Supernumerary teeth--an overview of classification, diagnosis and management. J Can Dent Assoc. 65:612–6. PMID: 10658390. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=0033253662&origin=inward.28. Kinirons MJ. 1982; Unerupted premaxillary supernumerary teeth. A study of their occurrence in males and females. Br Dent J. 153:110. DOI: 10.1038/sj.bdj.4804863. PMID: 6957208. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=0020474191&origin=inward.29. Celikoglu M, Kazanci F, Miloglu O, Oztek O, Kamak H, Ceylan I. 2010; Frequency and characteristics of tooth agenesis among an orthodontic patient population. Med Oral Patol Oral Cir Bucal. 15:e797–801. DOI: 10.4317/medoral.15.e797. PMID: 20383097. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=77956405148&origin=inward.30. Bedoya MM, Park JH. 2009; A review of the diagnosis and management of impacted maxillary canines. J Am Dent Assoc. 140:1485–93. DOI: 10.14219/jada.archive.2009.0099. PMID: 19955066. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=75249101074&origin=inward.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparing locus of control in orthodontic patients of a university dental hospital with those of a private dental clinic
- Reader's Forum
- A study on changes in the form and dimensions of dental arches resulting from orthodontic treatment
- Prevalence of dental anomalies among 7- to 35-year-old people in Hamadan, Iran in 2012-2013 as observed using panoramic radiographs
- Prevalence of Dental Anomalies in Patients with Non-syndromic Cleft Lip with or without Cleft Palate