Ann Rehabil Med.
2022 Aug;46(4):209-218. 10.5535/arm.22050.
Accuracy and Validity of Commercial Smart Bands for Heart Rate Measurements During Cardiopulmonary Exercise Test
- Affiliations
-
- 1Department of Rehabilitation Medicine, Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea
- 2Department of Rehabilitation Medicine, Sanggye Paik Hospital, Seoul, Korea
- KMID: 2532954
- DOI: http://doi.org/10.5535/arm.22050
Abstract
Objective
To assess the accuracies and validities of popular smart bands for heart rate (HR) measurement in cardiovascular disease (CVD) patients during a graded exercise test (GXT).
Methods
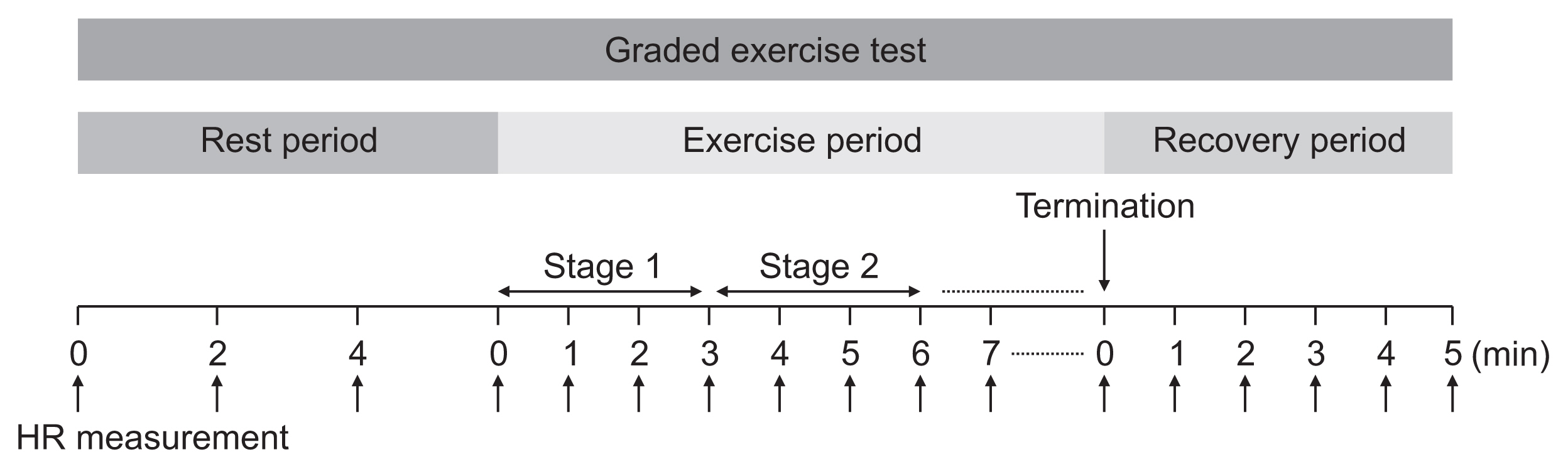
Seventy-eight patients were randomly assigned to wear two different smart bands out of three possible choices: Samsung Galaxy Fit 2, Xiaomi Mi Band 5, or Partron PWB-250 on each wrist. A 12-lead exercise electrocardiogram (ECG) and patch-type single-lead ECG were used to assess the comparative HR accuracy of the smart bands. The HR was recorded during the GXT using the modified Bruce protocol.
Results
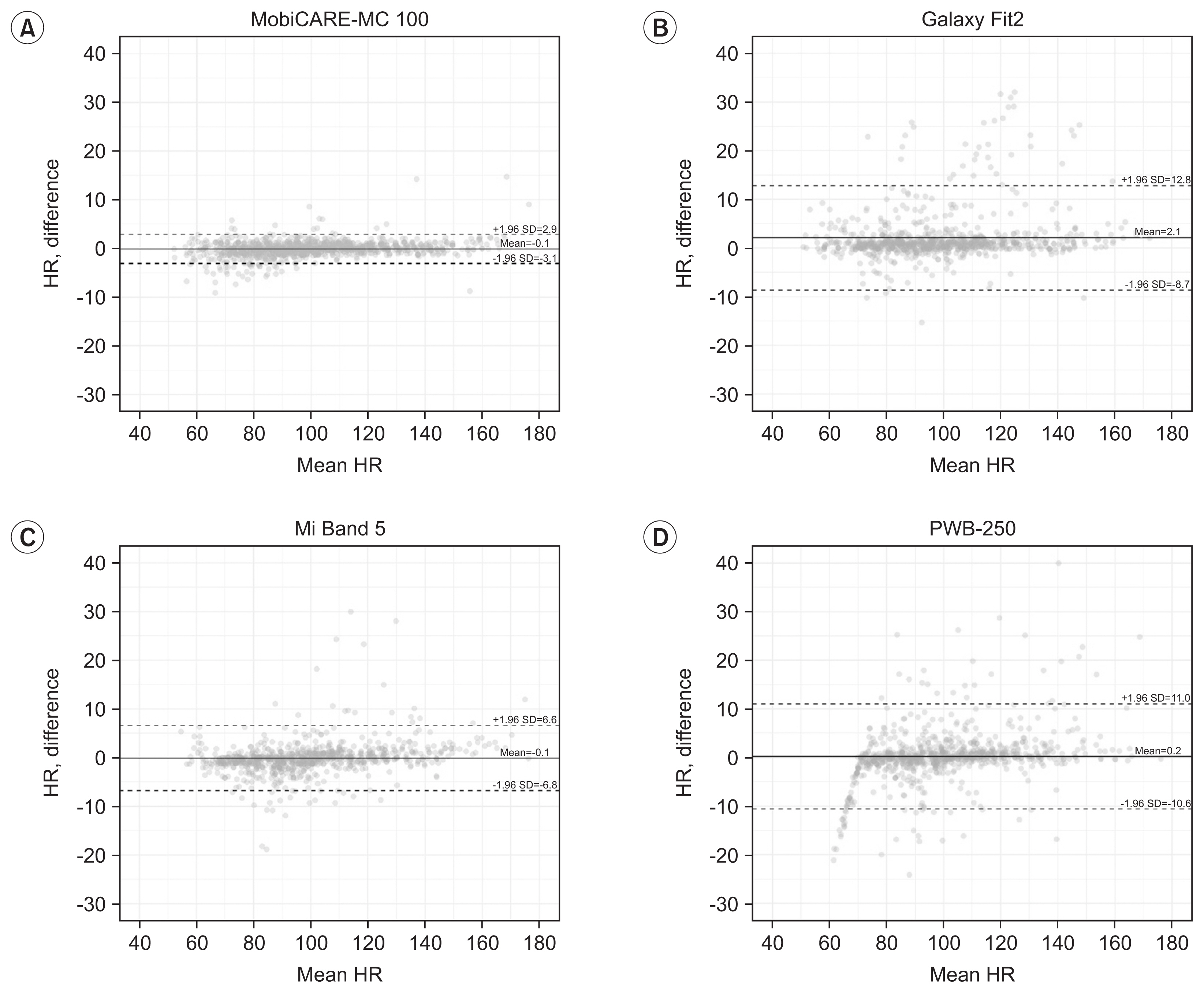
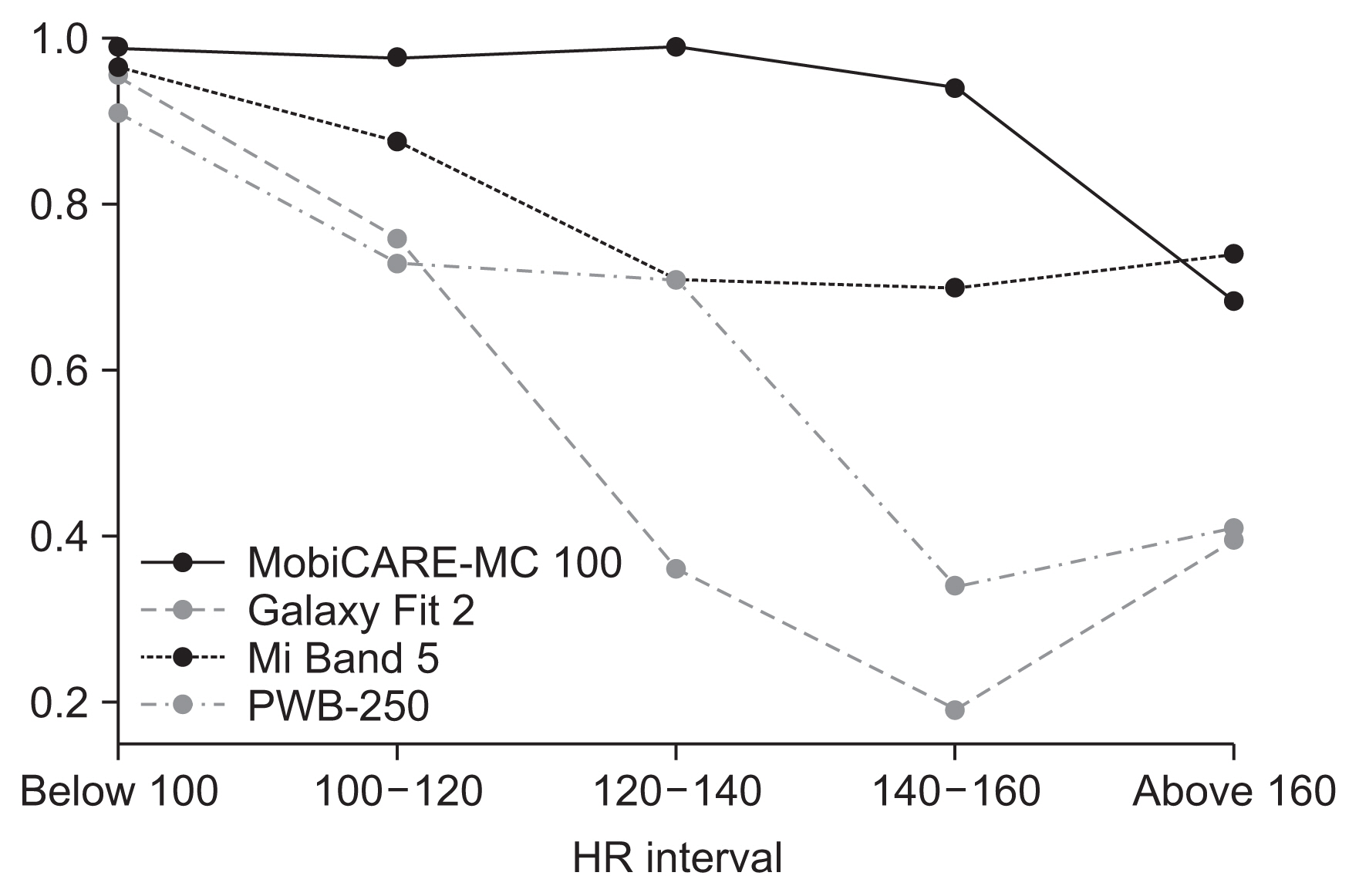
The concordance correlation coefficients (rc) were calculated to provide a measure of agreement between each device and the ECG. In all conditions, the Mi Band 5 and Galaxy Fit 2’ correlations were rc>0.90, while the PWB-250 correlation was rc=0.58 at rest. When evaluating the accuracy according to the magnitude of HR, all smart bands performed well (rc>0.90) when the HR was below 100 but accuracy tended to decrease with higher HR values.
Conclusion
This study showed that the three smart bands had a high level of accuracy for HR measurements during low-intensity exercise. However, during moderate-intensity and high-intensity exercise, all the three smart bands performed less accurately. Further studies are needed to find a more optimal smart band for HR measurement that can be used for precise HR monitoring during formal cardiac rehabilitation exercise training, including at high and maximal intensity (Clinical Trial Registration No. cris.nih.go.kr/KCT0007036).
Keyword
Figure
Reference
-
1. Taylor RS, Brown A, Ebrahim S, Jolliffe J, Noorani H, Rees K, et al. Exercise-based rehabilitation for patients with coronary heart disease: systematic review and meta-analysis of randomized controlled trials. Am J Med. 2004; 116:682–92.
Article2. Clark AM, Hartling L, Vandermeer B, McAlister FA. Meta-analysis: secondary prevention programs for patients with coronary artery disease. Ann Intern Med. 2005; 143:659–72.
Article3. McMahon SR, Ades PA, Thompson PD. The role of cardiac rehabilitation in patients with heart disease. Trends Cardiovasc Med. 2017; 27:420–5.
Article4. Smith SC Jr, Benjamin EJ, Bonow RO, Braun LT, Creager MA, Franklin BA, et al. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation endorsed by the World Heart Federation and the Preventive Cardiovascular Nurses Association. J Am Coll Cardiol. 2011; 58:2432–46.5. Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018; 39:119–77.6. American Association of Cardiovascular and Pulmonary Rehabilitation. Guidelines for cardiac rehabilitation and secondary prevention programs. 5th ed. Champaign, IL: Human Kinetics;2013.7. Clark RA, Conway A, Poulsen V, Keech W, Tirimacco R, Tideman P. Alternative models of cardiac rehabilitation: a systematic review. Eur J Prev Cardiol. 2015; 22:35–74.
Article8. Im HW, Baek S, Jee S, Ahn JM, Park MW, Kim WS. Barriers to outpatient hospital-based cardiac rehabilitation in Korean patients with acute coronary syndrome. Ann Rehabil Med. 2018; 42:154–65.
Article9. Dalal HM, Zawada A, Jolly K, Moxham T, Taylor RS. Home based versus centre based cardiac rehabilitation: Cochrane systematic review and meta-analysis. BMJ. 2010; 340:b5631.
Article10. Ruano-Ravina A, Pena-Gil C, Abu-Assi E, Raposeiras S, van’t Hof A, Meindersma E, et al. Participation and adherence to cardiac rehabilitation programs: a systematic review. Int J Cardiol. 2016; 223:436–43.
Article11. Kraal JJ, Peek N, van den Akker-Van Marle ME, Kemps HM. Effects and costs of home-based training with telemonitoring guidance in low to moderate risk patients entering cardiac rehabilitation: The FIT@Home study. BMC Cardiovasc Disord. 2013; 13:82.
Article12. Bidargaddi NP, Sarela A. Activity and heart rate-based measures for outpatient cardiac rehabilitation. Methods Inf Med. 2008; 47:208–16.
Article13. Brouwers RW, van Exel HJ, van Hal JM, Jorstad HT, de Kluiver EP, Kraaijenhagen RA, et al. Cardiac telerehabilitation as an alternative to centre-based cardiac rehabilitation. Neth Heart J. 2020; 28:443–51.
Article14. Gillinov S, Etiwy M, Wang R, Blackburn G, Phelan D, Gillinov AM, et al. Variable accuracy of wearable heart rate monitors during aerobic exercise. Med Sci Sports Exerc. 2017; 49:1697–703.
Article15. Chow HW, Yang CC. Accuracy of optical heart rate sensing technology in wearable fitness trackers for young and older adults: validation and comparison study. JMIR Mhealth Uhealth. 2020; 8:e14707.
Article16. Pasadyn SR, Soudan M, Gillinov M, Houghtaling P, Phelan D, Gillinov N, et al. Accuracy of commercially available heart rate monitors in athletes: a prospective study. Cardiovasc Diagn Ther. 2019; 9:379–85.
Article17. Dooley EE, Golaszewski NM, Bartholomew JB. Estimating accuracy at exercise intensities: a comparative study of self-monitoring heart rate and physical activity wearable devices. JMIR Mhealth Uhealth. 2017; 5:e34.
Article18. Thiebaud RS, Funk MD, Patton JC, Massey BL, Shay TE, Schmidt MG, et al. Validity of wrist-worn consumer products to measure heart rate and energy expenditure. Digit Health. 2018; 4:2055207618770322.
Article19. Etiwy M, Akhrass Z, Gillinov L, Alashi A, Wang R, Blackburn G, et al. Accuracy of wearable heart rate monitors in cardiac rehabilitation. Cardiovasc Diagn Ther. 2019; 9:262–71.
Article20. Falter M, Budts W, Goetschalckx K, Cornelissen V, Buys R. Accuracy of Apple Watch measurements for heart rate and energy expenditure in patients with cardiovascular disease: cross-sectional study. JMIR Mhealth Uhealth. 2019; 7:e11889.
Article21. Heyken M, Horstmann H, Kerling A, Albrecht K, Kedia G, Kuck M, et al. Comparison of wearables for self-monitoring of heart rate in coronary rehabilitation patients. Georgian Med News. 2021; 31(5):78–85.22. Albouaini K, Egred M, Alahmar A, Wright DJ. Cardiopulmonary exercise testing and its application. Postgrad Med J. 2007; 83:675–82.
Article23. Fletcher GF, Balady GJ, Amsterdam EA, Chaitman B, Eckel R, Fleg J, et al. Exercise standards for testing and training: a statement for healthcare professionals from the American Heart Association. Circulation. 2001; 104:1694–740.24. McBride GB. A proposal for strength-of-agreement criteria for Lin’s concordance correlation coefficient (NIWA Client Report No. HAM2005-062). Hamilton, New Zealand: National Institute of Water and Atmospheric Research;2005.25. Garber CE, Blissmer B, Deschenes MR, Franklin BA, Lamonte MJ, Lee IM, et al. American College of Sports Medicine position stand: quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011; 43:1334–59.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Correction: Accuracy and Validity of Commercial Smart Bands for Heart Rate Measurements During Cardiopulmonary Exercise Test
- Cardiopulmonary Exercise Testing and Interpretation of the Major Related Variables in Patients with Congenital Heart Disease
- Reliability of 6-Minute Walk Test in Stroke Patients
- Comparison of Exercise Pulmonary Function test Using by Treadmill and Bicycle Ergometer in Patients with Respiratory Diseases
- The Effect of a Self Exercise Program in Cardiac Rehabilitation for Patients with Coronary Artery Disease