Arch Hand Microsurg.
2022 Sep;27(3):247-257. 10.12790/ahm.21.0137.
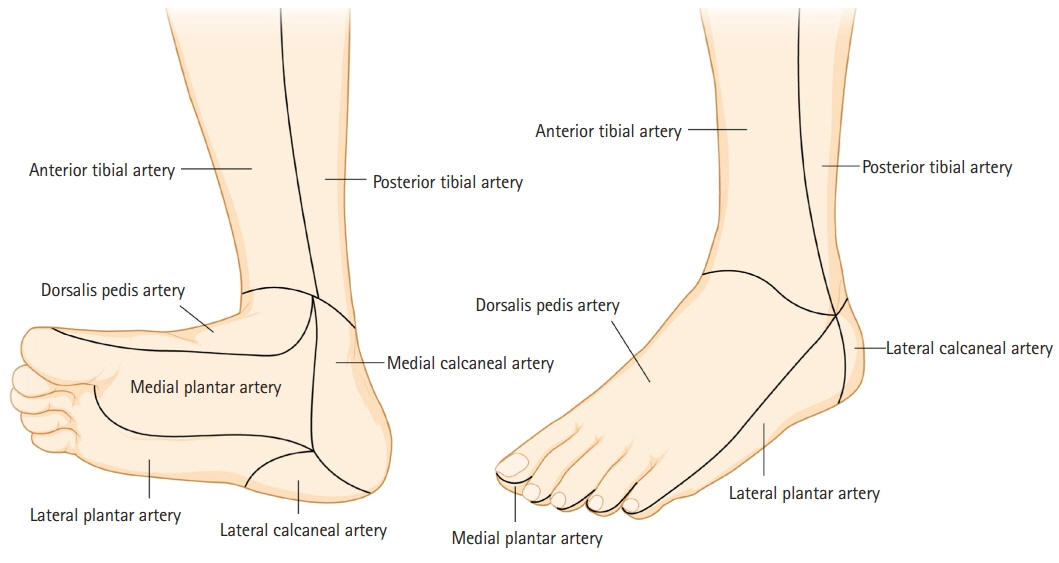
Clinical analysis of the communicating artery between the dorsal and plantar aspects of the foot
- Affiliations
-
- 1Department of Plastic and Reconstructive Surgery, Soonchunhyang University College of Medicine, Cheonan, Korea
- 2Department of Cardiology, Soonchunhyang University College of Medicine, Cheonan, Korea
- 3Institute of Tissue Regeneration, Soonchunhyang University College of Medicine, Cheonan, Korea
- KMID: 2532742
- DOI: http://doi.org/10.12790/ahm.21.0137
Abstract
- Purpose
One of the treatment methods for critical limb ischemia is percutaneous transluminal angioplasty (PTA). In severe cases, however, multiple vessels are blocked, including the main vessels of the lower extremities. This study aimed to determine whether wound healing and symptom relief occurred depending on whether the communicating artery was patent after PTA.
Methods
In total, 120 patients (120 lower extremities) who underwent PTA from January 2016 to February 2018 were followed up for 6 months.
Results
Out of 87 patients who had wounds, 34 had a patent communicating artery and 53 had a non-patent communicating artery. Out of 34 patients who had wounds but a patent communicating artery, 29 completely healed within 6 months. Among the 53 patients who had wounds and a non-patent communicating artery, 16 totally healed within 6 months, and 37 did not heal within 6 months. In the indirect revascularization group, 18 of 21 patients with complete wound healing within 6 months in the indirect revascularization group had a patent communicating artery.
Conclusion
If only indirect revascularization is possible, it is important to ensure the patency of the communicating vessels that link the pedal and plantar arterial systems.
Keyword
Figure
Reference
-
References
1. Fowkes FG, Rudan D, Rudan I, et al. Comparison of global estimates of prevalence and risk factors for peripheral artery disease in 2000 and 2010: a systematic review and analysis. Lancet. 2013; 382:1329–40.2. Norgren L, Hiatt WR, Dormandy JA, et al. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). J Vasc Surg. 2007; 45 Suppl S:S5–67.3. Hirsch AT, Haskal ZJ, Hertzer NR, et al. ACC/AHA 2005 guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): executive summary a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease) endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; and Vascular Disease Foundation. J Am Coll Cardiol. 2006; 47:1239–312.4. Rutherford RB, Baker JD, Ernst C, et al. Recommended standards for reports dealing with lower extremity ischemia: revised version. J Vasc Surg. 1997; 26:517–38.5. Bosanquet DC, Glasbey JC, Williams IM, Twine CP. Systematic review and meta-analysis of direct versus indirect angiosomal revascularisation of infrapopliteal arteries. Eur J Vasc Endovasc Surg. 2014; 48:88–97.6. Biancari F, Juvonen T. Angiosome-targeted lower limb revascularization for ischemic foot wounds: systematic review and meta-analysis. Eur J Vasc Endovasc Surg. 2014; 47:517–22.7. Attinger CE, Evans KK, Bulan E, Blume P, Cooper P. Angiosomes of the foot and ankle and clinical implications for limb salvage: reconstruction, incisions, and revascularization. Plast Reconstr Surg. 2006; 117(7 Suppl):261S–293S.8. Taylor GI, Palmer JH. The vascular territories (angiosomes) of the body: experimental study and clinical applications. Br J Plast Surg. 1987; 40:113–41.9. Neville RF, Attinger CE, Bulan EJ, Ducic I, Thomassen M, Sidawy AN. Revascularization of a specific angiosome for limb salvage: does the target artery matter? Ann Vasc Surg. 2009; 23:367–73.10. Alson MD, Lang EV, Kaufman JA. Pedal arterial imaging. J Vasc Interv Radiol. 1997; 8(1 Pt 1):9–18.11. Manzi M, Fusaro M, Ceccacci T, Erente G, Dalla Paola L, Brocco E. Clinical results of below-the knee intervention using pedal-plantar loop technique for the revascularization of foot arteries. J Cardiovasc Surg (Torino). 2009; 50:331–7.12. Corson JD, Karmody AM, Shah DM, Naraynsingh V, Young HL, Leather RP. In situ vein bypasses to distal tibial and limited outflow tracts for limb salvage. Surgery. 1984; 96:756–63.13. Fusaro M, Dalla Paola L, Brigato C, et al. Plantar to dorsalis pedis artery subintimal angioplasty in a patient with critical foot ischemia: a novel technique in the armamentarium of the peripheral interventionist. J Cardiovasc Med (Hagerstown). 2007; 8:977–80.14. Jung H, Ahn CM, Ko YG, Choi D. Immediate and late outcomes of pedal-plantar loop technique for revascularization of below-the-knee arteries in patients with critical limb ischemia. Circulation. 2017; 136(Suppl 1):A19554.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect of Ballet Shoes on Plantar Foot during Ambulation
- Hinged multiperforator-based extended dorsalis pedis adipofascial flap for dorsal foot defects
- Plantar Fibromatosis: A Case Report
- Microsurgical anatomy of the Anterior Cerebral-anterior Communicating Artery
- Isolated Dorsal Dislocation of Intermediate Cuneiform: A Case Report