Korean J Gastroenterol.
2022 Jul;80(1):34-37. 10.4166/kjg.2022.043.
Paneth Cell Carcinoma of the Stomach
- Affiliations
-
- 1Division of Gastroenterology, Pusan National University Hospital, Busan, Korea
- 2Department of Internal Medicine, Pusan National University College of Medicine, Busan, Korea
- 3Biomedical Research Institute, Pusan National University Hospital, Busan, Korea
- 4Department of Pathology, Pusan National University Hospital, Busan, Korea
- KMID: 2532165
- DOI: http://doi.org/10.4166/kjg.2022.043
Abstract
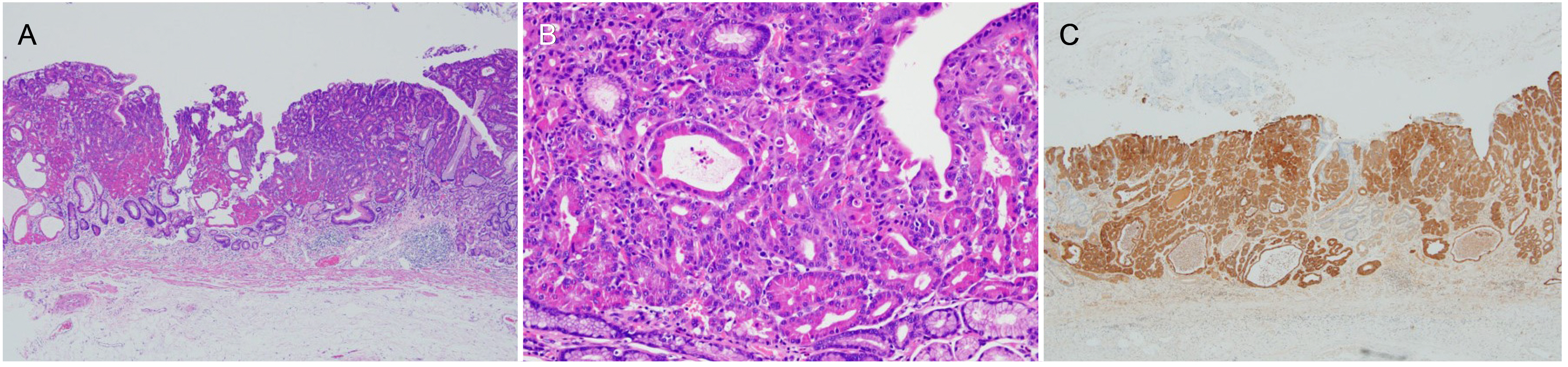
- Paneth cell carcinoma is a rare carcinoma composed predominantly or purely of malignant Paneth cells. An 83-year-old woman presented for evaluation of an elevated lesion in the stomach. On endoscopy, a 15 mm, discolored, elevated lesion with a central depression was found on the greater curvature of the gastric lower body. Endoscopic forceps biopsy revealed chronic gastritis with intestinal metaplasia. Magnifying endoscopy revealed an irregularly oval/tubular microsurface pattern and an irregular loop microvascular pattern with a demarcation line, suggestive of early gastric cancer. Therefore, endoscopic submucosal dissection was performed. Histopathological examination revealed a well-differentiated tubular adenocarcinoma limited to the muscularis mucosae and the tumor cells contained coarse eosinophilic granules in the cytoplasm. These tumor cells were diffusely and strongly stained for lysozyme, confirming the tumor diagnosis as Paneth cell carcinoma. Herein, we report a rare case of Paneth cell carcinoma and its endoscopic and histopathologic findings.
Figure
Reference
-
1. Lauren P. 1965; The two histological main types of gastric carcinoma: diffuse and so-called intestinal-type carcinoma. An attempt at a histo-clinical classification. Acta Pathol Microbiol Scand. 64:31–49. DOI: 10.1111/apm.1965.64.1.31. PMID: 14320675.2. Sugano H, Nakamura K, Kato Y. 1982; Pathological studies of human gastric cancer. Acta Pathol Jpn. 32(Suppl 2):329–347. PMID: 6765003.3. Chang JI, Kim TJ, Hwang NY, et al. 2022; Clinical outcomes and adverse events of gastric endoscopic submucosal dissection of the mid to upper stomach under general anesthesia and monitored anesthetic care. Clin Endosc. 55:77–85. DOI: 10.5946/ce.2021.002. PMID: 34224661. PMCID: PMC8831404.4. Park CH, Yang DH, Kim JW, et al. 2020; Clinical practice guideline for endoscopic resection of early gastrointestinal cancer. Clin Endosc. 53:142–166. DOI: 10.5946/ce.2020.032. PMID: 32252507. PMCID: PMC7137564.5. Nakamura K, Sakuragi N, Takakuwa A, Ayabe T. 2016; Paneth cell α-defensins and enteric microbiota in health and disease. Biosci Microbiota Food Health. 35:57–67. DOI: 10.12938/bmfh.2015-019. PMID: 27200259. PMCID: PMC4858879.6. Simmonds N, Furman M, Karanika E, Phillips A, Bates AW. 2014; Paneth cell metaplasia in newly diagnosed inflammatory bowel disease in children. BMC Gastroenterol. 14:93. DOI: 10.1186/1471-230X-14-93. PMID: 24885054. PMCID: PMC4037749.7. Luo W, Hofstetter WL, Tan D. 2019; Gastroesophageal junction Paneth cell carcinoma with extensive cystic and secretory features - case report and literature review. Diagn Pathol. 14:1. DOI: 10.1186/s13000-018-0775-z. PMID: 30621725. PMCID: PMC6323739.8. Geller SA, Thung SN. 1983; Morphologic unity of Paneth cells. Arch Pathol Lab Med. 107:476–479. PMID: 6192791.9. Symonds DA. 1974; Paneth cell metaplasia in diseases of the colon and rectum. Arch Pathol. 97:343–347. PMID: 4363393.10. Iwama T, Utsunomiya J, Hamaguchi E. 1975; The Paneth cell in the adenoma of familial polyposis coli. Bull Tokyo Med Dent Univ. 22:151–154. PMID: 1064485.11. Rubio CA. 2003; Colorectal adenomas produce lysozyme. Anticancer Res. 23:5165–5171. PMID: 14981984.12. Wada R, Yamaguchi T, Tadokoro K. 2005; Colonic Paneth cell metaplasia is pre-neoplastic condition of colonic cancer or not? J Carcinog. 4:5. DOI: 10.1186/1477-3163-4-5. PMID: 15707498. PMCID: PMC549518.13. Chen W, Frankel WL, Cronley KM, Yu L, Zhou X, Yearsley MM. 2015; Significance of paneth cell metaplasia in Barrett esophagus: a morphologic and clinicopathologic study. Am J Clin Pathol. 143:665–671. DOI: 10.1309/AJCPVUJMCVBC9PKM. PMID: 25873500. PMCID: PMC4504017.14. Mahon M, Xu J, Yi X, Liu X, Gao N, Zhang L. 2016; Paneth cell in adenomas of the distal colorectum is inversely associated with synchronous advanced adenoma and carcinoma. Sci Rep. 6:26129. DOI: 10.1038/srep26129. PMID: 27188450. PMCID: PMC4870568.15. Fukasawa T, Suzuki S, Fujii H. 2006; A case report of early gastric cancer with Paneth-like tumor cells. Nihon Shokakibyo Gakkai Zasshi. 103:1251–1256. DOI: 10.11641/pde.58.2_64. PMID: 17085906.16. Lee W. 2021; Application of current image-enhanced endoscopy in gastric diseases. Clin Endosc. 54:477–487. DOI: 10.5946/ce.2021.160. PMID: 34315196. PMCID: PMC8357595.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Paneth Cell-rich Carcinoma of the Stomach: A case report
- Neoplastic Paneth cells in the experimental murine carcinoma of the small intestine
- CT Findings of Primary Squamous Cell Carcinoma of the Stomach: A Case Report
- Ultrastructural Study of Crypt Cells in the Ileum of Mouse after Salmonella typhimurium Infection
- Lysozyme immunoreactivity of paneth cells of human, rat and mouse