J Yeungnam Med Sci.
2022 Jul;39(3):235-243. 10.12701/yujm.2021.01550.
Preemptive pyloroplasty for iatrogenic vagus nerve injury in intrahepatic cholangiocarcinoma patients undergoing extensive left-sided lymph node dissection: a retrospective observational study
- Affiliations
-
- 1Division of Hepatobiliary Surgery, Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2532077
- DOI: http://doi.org/10.12701/yujm.2021.01550
Abstract
- Background
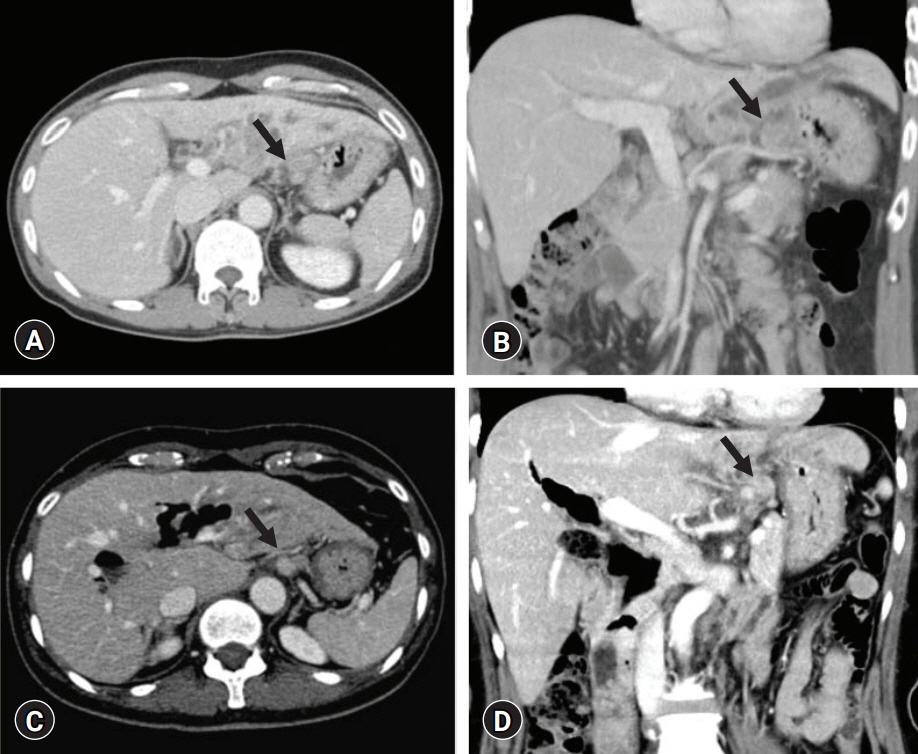
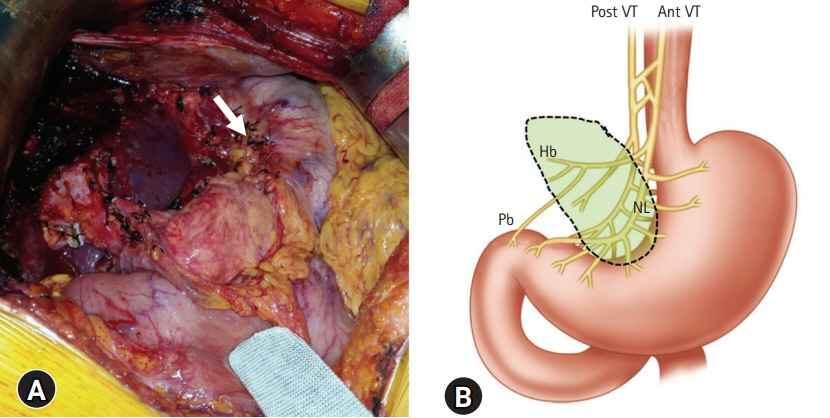
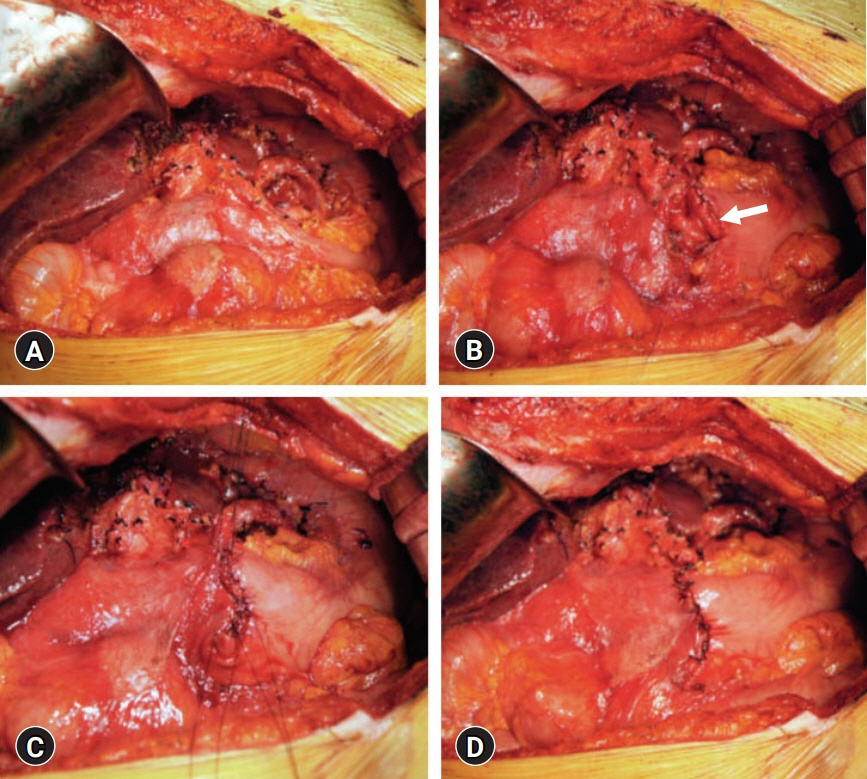
Intrahepatic cholangiocarcinoma (ICC) of the left liver often shows left-sided lymph node (LN) metastasis. If gastric lesser curvature is extensively dissected, it can induce an iatrogenic injury to the extragastric vagus nerve branches that control motility of the pyloric sphincter and lead to gastric stasis. To cope with such LN dissection-associated gastric stasis, we performed pyloroplasty preemptively. The objective of this study was to analyze our 20-year experience of preemptive pyloroplasty performed in 10 patients.
Methods
We investigated clinical sequences of 10 patients with ICC who underwent preemptive pyloroplasty following left hepatectomy and extended left-sided LN dissection. Incidence of gastric stasis and oncological survival outcomes were analyzed.
Results
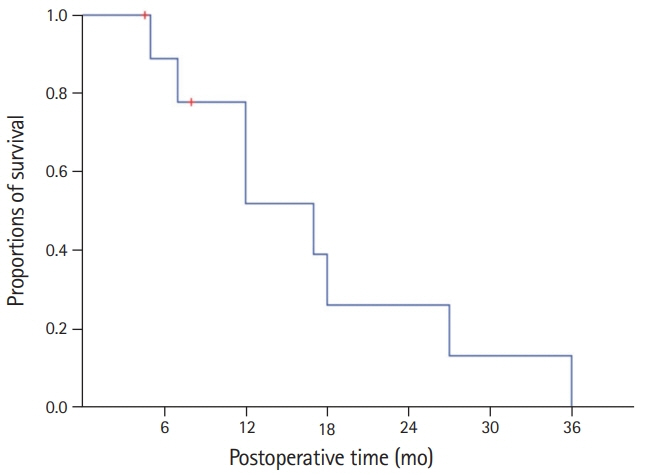
All 10 patients were classified as stage IIIB due to T1-3N1M0 stage according to the 8th edition of American Joint Committee on Cancer staging system. The overall patient survival rate was 51.9% at 1 year, 25.9% at 2 years, and 0% at 3 years. Seven patients showed uneventful postoperative recovery after surgery. Two patients suffered from gastric stasis, which was successfully managed with supportive care. One patient suffered from overt gastric paresis, which was successfully managed with azithromycin administration for 1 month.
Conclusion
We believe that preemptive pyloroplasty is an effective surgical option to prevent gastric stasis in patients undergoing extensive left-sided LN dissection. Azithromycin appears to be a potent prokinetic agent in gastroparesis.
Keyword
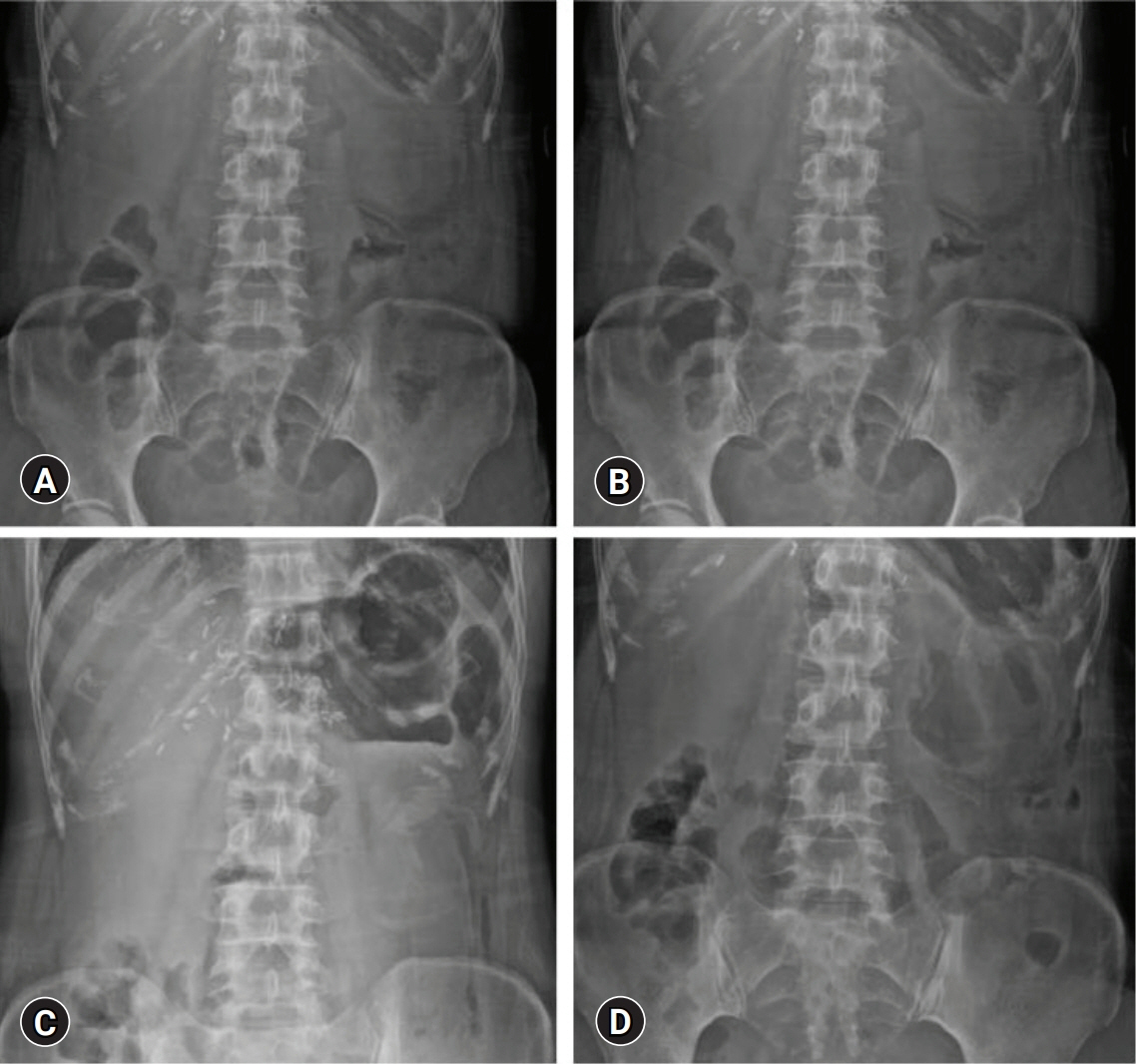
Figure
Reference
-
References
1. Tsuji T, Hiraoka T, Kanemitsu K, Takamori H, Tanabe D, Tashiro S. Lymphatic spreading pattern of intrahepatic cholangiocarcinoma. Surgery. 2001; 129:401–7.
Article2. Morine Y, Shimada M, Utsunomiya T, Imura S, Ikemoto T, Mori H, et al. Clinical impact of lymph node dissection in surgery for peripheral-type intrahepatic cholangiocarcinoma. Surg Today. 2012; 42:147–51.
Article3. Cho JW, Lee HW, Hwang S. Benefit of pyloroplasty to prevent gastric stasis in intrahepatic cholangiocarcinoma patients undergoing extensive left-sided lymph node dissection. Korean J Hepatobiliary Pancreat Surg. 2016; 20:32–7.
Article4. Lee A. Gastroparesis: what is the current state-of-the-art for evaluation and medical management?: what are the results? J Gastrointest Surg. 2013; 17:1553–6.
Article5. Stevens JE, Jones KL, Rayner CK, Horowitz M. Pathophysiology and pharmacotherapy of gastroparesis: current and future perspectives. Expert Opin Pharmacother. 2013; 14:1171–86.
Article6. Hwang S, Lee YJ, Song GW, Park KM, Kim KH, Ahn CS, et al. Prognostic impact of tumor growth type on 7th AJCC Staging System for intrahepatic cholangiocarcinoma: a single-center experience of 659 cases. J Gastrointest Surg. 2015; 19:1291–304.
Article7. Nathan H, Aloia TA, Vauthey JN, Abdalla EK, Zhu AX, Schulick RD, et al. A proposed staging system for intrahepatic cholangiocarcinoma. Ann Surg Oncol. 2009; 16:14–22.
Article8. Clark CJ, Wood-Wentz CM, Reid-Lombardo KM, Kendrick ML, Huebner M, Que FG. Lymphadenectomy in the staging and treatment of intrahepatic cholangiocarcinoma: a population-based study using the National Cancer Institute SEER database. HPB (Oxford). 2011; 13:612–20.
Article9. Adachi T, Eguchi S. Lymph node dissection for intrahepatic cholangiocarcinoma: a critical review of the literature to date. J Hepatobiliary Pancreat Sci. 2014; 21:162–8.
Article10. Ribero D, Pinna AD, Guglielmi A, Ponti A, Nuzzo G, Giulini SM, et al. Surgical approach for long-term survival of patients with intrahepatic cholangiocarcinoma: a multi-institutional analysis of 434 patients. Arch Surg. 2012; 147:1107–13.
Article11. de Jong MC, Nathan H, Sotiropoulos GC, Paul A, Alexandrescu S, Marques H, et al. Intrahepatic cholangiocarcinoma: an international multi-institutional analysis of prognostic factors and lymph node assessment. J Clin Oncol. 2011; 29:3140–5.
Article12. Lo CM. Complications and long-term outcome of living liver donors: a survey of 1,508 cases in five Asian centers. Transplantation. 2003; 75(3 Suppl):S12–5.
Article13. Hwang S, Lee SG, Lee YJ, Sung KB, Park KM, Kim KH, et al. Lessons learned from 1,000 living donor liver transplantations in a single center: how to make living donations safe. Liver Transpl. 2006; 12:920–7.
Article14. Kinoshita A, Takatsuki M, Hidaka M, Soyama A, Eguchi S, Kanematsu T. Prevention of gastric stasis by omentum patching after living donor left hepatectomy. Surg Today. 2012; 42:816–8.
Article15. Kendall BJ, Chakravarti A, Kendall E, Soykan I, McCallum RW. The effect of intravenous erythromycin on solid meal gastric emptying in patients with chronic symptomatic post-vagotomy-antrectomy gastroparesis. Aliment Pharmacol Ther. 1997; 11:381–5.
Article16. Malagelada JR, Rees WD, Mazzotta LJ, Go VL. Gastric motor abnormalities in diabetic and postvagotomy gastroparesis: effect of metoclopramide and bethanechol. Gastroenterology. 1980; 78:286–93.
Article17. Larson JM, Tavakkoli A, Drane WE, Toskes PP, Moshiree B. Advantages of azithromycin over erythromycin in improving the gastric emptying half-time in adult patients with gastroparesis. J Neurogastroenterol Motil. 2010; 16:407–13.
Article18. Sutera L, Dominguez LJ, Belvedere M, Putignano E, Vernuccio L, Ferlisi A, et al. Azithromycin in an older woman with diabetic gastroparesis. Am J Ther. 2008; 15:85–8.
Article19. Potter TG, Snider KR. Azithromycin for the treatment of gastroparesis. Ann Pharmacother. 2013; 47:411–5.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Benefit of pyloroplasty to prevent gastric stasis in intrahepatic cholangiocarcinoma patients undergoing extensive left-sided lymph node dissection
- Intrahepatic Cholangiocarcinoma Initially Presented as a Distant Metastatic Lymph Node without Demonstrable Hepatic Mass: A Case Report
- Non-recurrent Laryngeal Nerve Identified During Robotic Thyroidectomy in a Patient with Papillary Thyroid Carcinoma
- Management of Malignant Melanoma Using Sentinel Lymph Node Biopsy: A Case Report
- Treatment of Malignant Melanoma Using Sentinel Lymph Node Dissection