J Yeungnam Med Sci.
2022 Jul;39(3):230-234. 10.12701/yujm.2021.01515.
Assessment of normal anal sphincter anatomy using transanal ultrasonography in healthy Korean volunteers: a retrospective observational study
- Affiliations
-
- 1Hwanggeumbit Surgery Clinic, Daegu, Korea
- 2Department of Surgery, Yeungnam University College of Medicine, Daegu, Korea
- KMID: 2532076
- DOI: http://doi.org/10.12701/yujm.2021.01515
Abstract
- Background
To date, there have been no studies on the normal anatomic values of the anal sphincter in healthy Koreans. Therefore, this study aimed to determine the normal anatomic values of transanal ultrasonography (TAUS).
Methods
The thickness of the external anal sphincter (EAS) and internal anal sphincter (IAS) was measured by TAUS from healthy Korean volunteers between September 2019 and August 2021.
Results
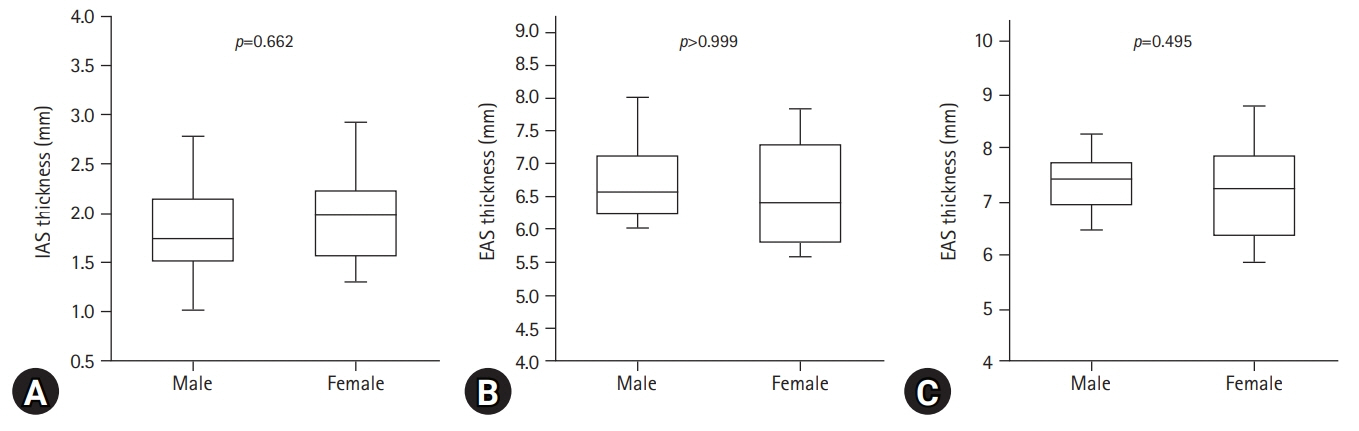
Thirty-six volunteers with a median age of 37 years (range, 20–77 years) and a median body mass index (BMI) of 23.5 kg/m2 (range, 17.2–31.2 kg/m2) were examined. The median thickness of the EAS at 4 cm and 2 cm from the anal verge was 7.4 mm (range, 5.8–8.8 mm) and 6.5 mm (range, 5.6–8.0 mm), respectively. The median thickness of the IAS at 2 cm from the anal verge was 1.8 mm (range, 0.8-4.3 mm). There were no differences in sphincter muscle thickness between the sexes. However, the EAS tended to thicken as the BMI increased (EAS at 2 cm and 4 cm from the anal verge, Spearman rho=0.433, 0.363; p=0.008 and p=0.029, respectively).
Conclusion
In healthy Korean, the median thickness of the IAS at 2 cm from the anal verge was 1.8 mm and the median thickness of the EAS at 2 cm and 4 cm from the anal verge was 6.5 mm and 7.4 mm respectively. There were no differences in anal sphincter thickness between sexes, but BMI was related to EAS thickness.
Keyword
Figure
Reference
-
References
1. National Health Insurance Service (NHIS). Main surgery statistical yearbook for 2019 [Internet]. Wonju: NHIS;2020. [cited 2021 Sep 14]. https://www.nhis.or.kr/nhis/together/wbhaec06800m01.do?mode=view&articleNo=10803657&article.offset=0&articleLimit=10.2. Volløyhaug I, Taithongchai A, Arendsen L, van Gruting I, Sultan AH, Thakar R. Is endoanal, introital or transperineal ultrasound diagnosis of sphincter defects more strongly associated with anal incontinence? Int Urogynecol J. 2020; 31:1471–8.
Article3. Walsh KA, Grivell RM. Use of endoanal ultrasound for reducing the risk of complications related to anal sphincter injury after vaginal birth. Cochrane Database Syst Rev. 2015; 2015:CD010826.
Article4. Visscher AP, Felt-Bersma RJ. Endoanal ultrasound in perianal fistulae and abscesses. Ultrasound Q. 2015; 31:130–7.
Article5. Burnett SJ, Bartram CI. Endosonographic variations in the normal internal anal sphincter. Int J Colorectal Dis. 1991; 6:2–4.
Article6. Nielsen MB, Hauge C, Rasmussen OO, Sørensen M, Pedersen JF, Christiansen J. Anal sphincter size measured by endosonography in healthy volunteers. Effect of age, sex, and parity. Acta Radiol. 1992; 33:453–6.
Article7. Enck P, Heyer T, Gantke B, Schmidt WU, Schäfer R, Frieling T, et al. How reproducible are measures of the anal sphincter muscle diameter by endoanal ultrasound? Am J Gastroenterol. 1997; 92:293–6.8. Law PJ, Bartram CI. Anal endosonography: technique and normal anatomy. Gastrointest Radiol. 1989; 14:349–53.
Article9. Nielsen MB, Pedersen JF, Hauge C, Rasmussen OO, Christiansen J. Endosonography of the anal sphincter: findings in healthy volunteers. AJR Am J Roentgenol. 1991; 157:1199–202.
Article10. Huebner M, Margulies RU, Fenner DE, Ashton-Miller JA, Bitar KN, DeLancey JO. Age effects on internal anal sphincter thickness and diameter in nulliparous females. Dis Colon Rectum. 2007; 50:1405–11.
Article11. Frudinger A, Halligan S, Bartram CI, Price AB, Kamm MA, Winter R. Female anal sphincter: age-related differences in asymptomatic volunteers with high-frequency endoanal US. Radiology. 2002; 224:417–23.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Comparison between Transanal and Transvaginal Ultrasonography of Anal Sphincter in Normal Women
- Anal Endosonographic Findings of Internal Anal Sphincter in Normal Adult Korean
- Evaluation of Anal Continence Function by Analysis of the Rectoanal Reflex
- Transrectal ultrasonography of anorectal diseases: advantages and disadvantages
- Digital flexor tendons of the hand: normal ultrasonographic anatomy