Diabetes Metab J.
2022 Jul;46(4):578-591. 10.4093/dmj.2021.0135.
Reproductive Life Span and Severe Hypoglycemia Risk in Postmenopausal Women with Type 2 Diabetes Mellitus
- Affiliations
-
- 1Division of Gynecologic Endocrinology, Department of Obstetrics and Gynecology, St. Vincent’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Department of Epidemiology, Fay W. Boozman College of Public Health, University of Arkansas for Medical Sciences, Little Rock, AR, USA
- 3Division of Gynecologic Endocrinology, Department of Obstetrics and Gynecology, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 4Division of Gynecologic Endocrinology, Department of Obstetrics and Gynecology, Eunpyeong St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 5Department of Statistics and Actuarial Science, Soongsil University, Seoul, Korea
- 6Division of Endocrinology and Metabolism, Department of Internal Medicine, St. Vincent’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2531962
- DOI: http://doi.org/10.4093/dmj.2021.0135
Abstract
- Background
Estrogen promotes glucose homeostasis, enhances insulin sensitivity, and maintains counterregulatory responses in recurrent hypoglycemia in women of reproductive age. Postmenopausal women with type 2 diabetes mellitus (T2DM) might be more vulnerable to severe hypoglycemia (SH) events. However, the relationship between reproductive factors and SH occurrence in T2DM remains unelucidated.
Methods
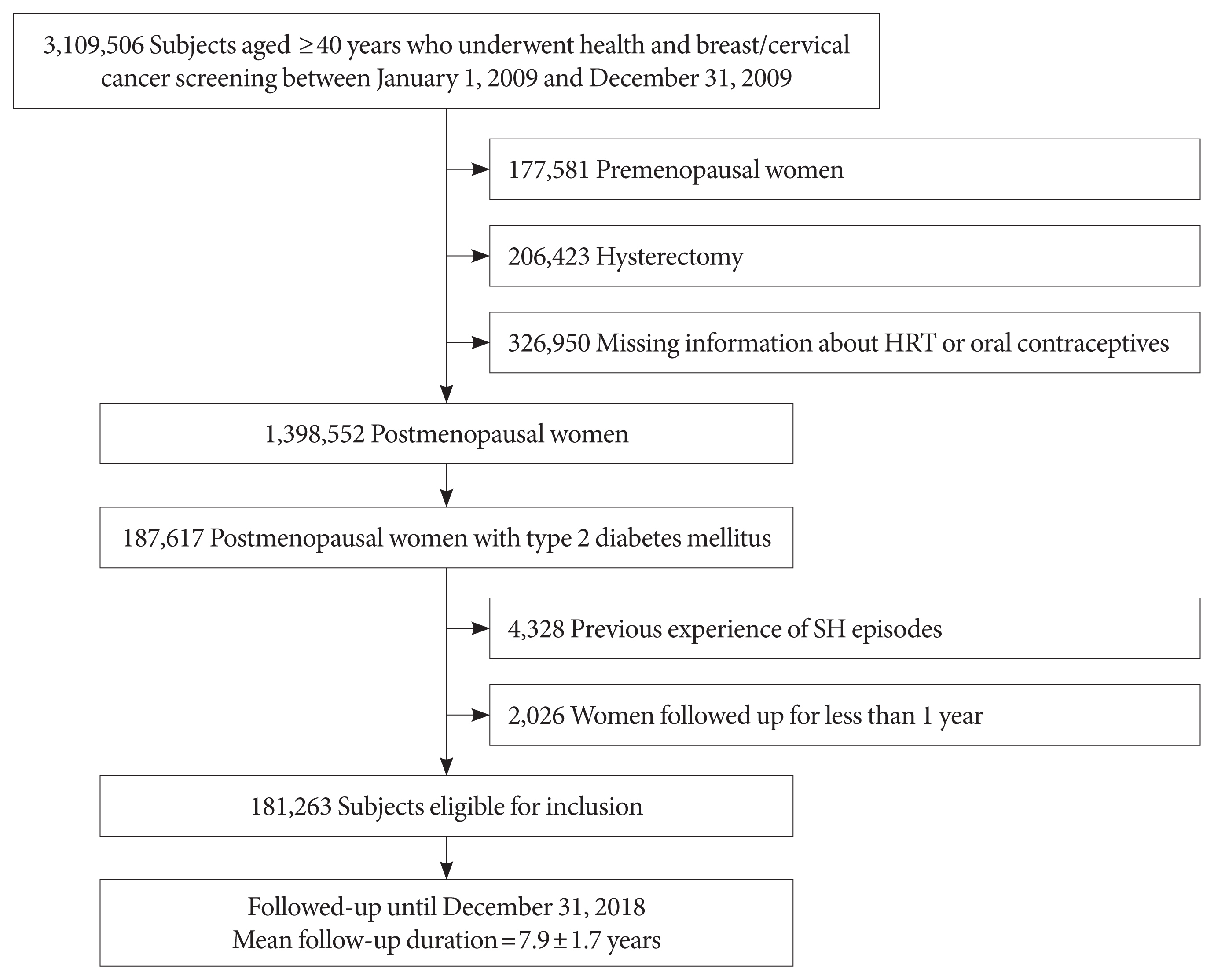
This study included data on 181,263 women with postmenopausal T2DM who participated in a national health screening program from January 1 to December 31, 2009, obtained using the Korean National Health Insurance System database. Outcome data were obtained until December 31, 2018. Associations between reproductive factors and SH incidence were assessed using Cox proportional hazards models.
Results
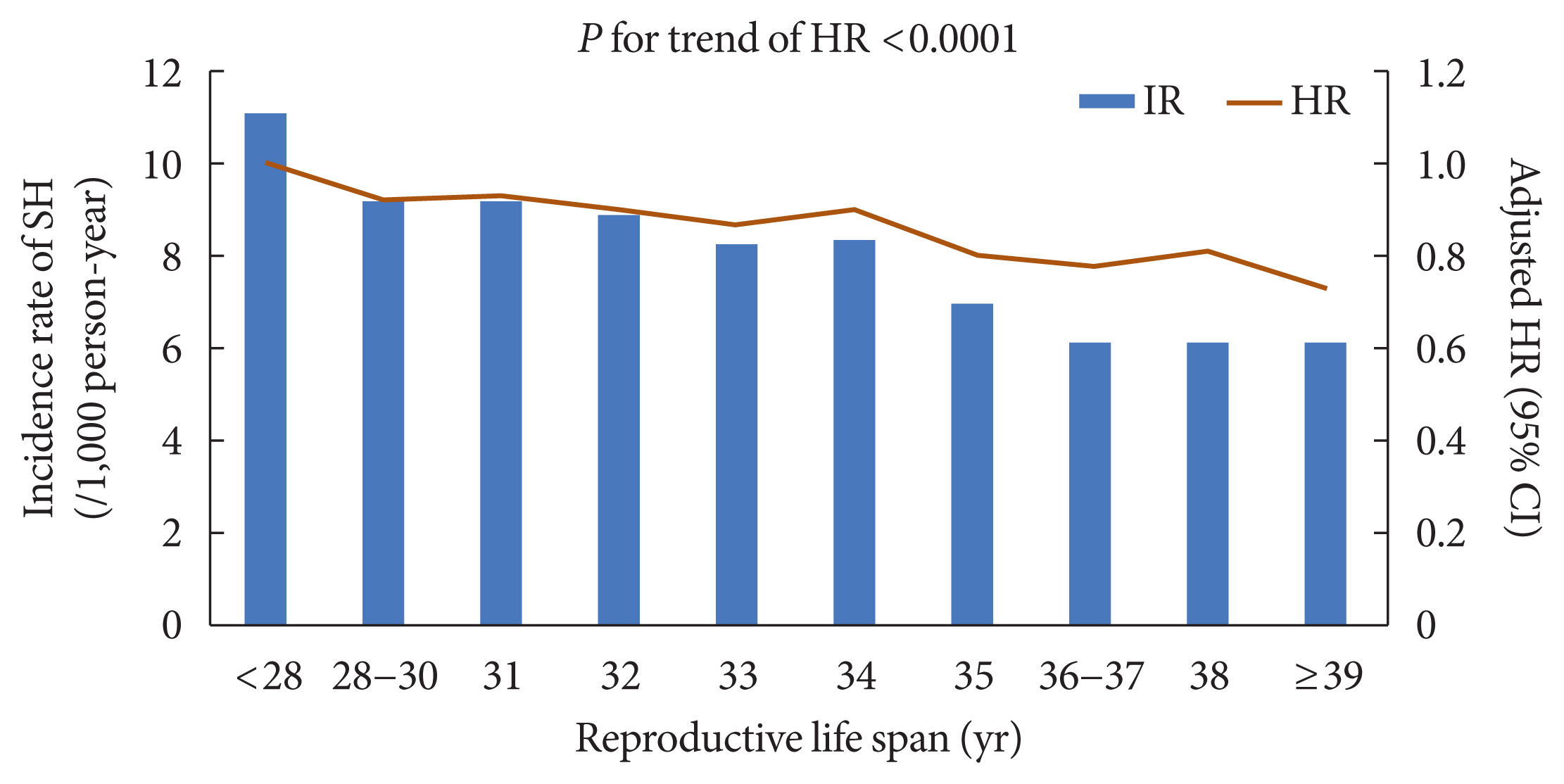
During the mean follow-up of 7.9 years, 11,279 (6.22%) postmenopausal women with T2DM experienced SH episodes. A longer reproductive life span (RLS) (≥40 years) was associated with a lower SH risk compared to a shorter RLS (<30 years) (adjusted hazard ratio [HR], 0.74; 95% confidence interval [CI], 0.69 to 0.80; P for trend <0.001) after multivariable adjustment. SH risk decreased with every 5-year increment of RLS (with <30 years as a reference [adjusted HR, 0.91; 95% CI, 0.86 to 0.95; P=0.0001 for 30−34 years], [adjusted HR, 0.80; 95% CI, 0.76 to 0.84; P<0.001 for 35−39 years], [adjusted HR, 0.74; 95% CI, 0.68 to 0.81; P<0.001 for ≥40 years]). The use of hormone replacement therapy (HRT) was associated with a lower SH risk than HRT nonuse.
Conclusion
Extended exposure to endogenous ovarian hormone during lifetime may decrease the number of SH events in women with T2DM after menopause.
Keyword
Figure
Reference
-
1. Gillies GE, McArthur S. Estrogen actions in the brain and the basis for differential action in men and women: a case for sex-specific medicines. Pharmacol Rev. 2010; 62:155–98.
Article2. Patel S, Homaei A, Raju AB, Meher BR. Estrogen: the necessary evil for human health, and ways to tame it. Biomed Pharmacother. 2018; 102:403–11.
Article3. Shadyab AH, Macera CA, Shaffer RA, Jain S, Gallo LC, Gass ML, et al. Ages at menarche and menopause and reproductive lifespan as predictors of exceptional longevity in women: the Women’s Health Initiative. Menopause. 2017; 24:35–44.
Article4. Brand JS, van der Schouw YT, Onland-Moret NC, Sharp SJ, Ong KK, Khaw KT, et al. Age at menopause, reproductive life span, and type 2 diabetes risk: results from the EPIC-InterAct study. Diabetes Care. 2013; 36:1012–9.5. Iqbal A, Heller S. Managing hypoglycaemia. Best Pract Res Clin Endocrinol Metab. 2016; 30:413–30.
Article6. Choi SY, Ko SH. Severe hypoglycemia as a preventable risk factor for cardiovascular disease in patients with type 2 diabetes mellitus. Korean J Intern Med. 2021; 36:263–70.
Article7. Silbert R, Salcido-Montenegro A, Rodriguez-Gutierrez R, Katabi A, McCoy RG. Hypoglycemia among patients with type 2 diabetes: epidemiology, risk factors, and prevention strategies. Curr Diab Rep. 2018; 18:53.
Article8. McCoy RG, Van Houten HK, Ziegenfuss JY, Shah ND, Wermers RA, Smith SA. Increased mortality of patients with diabetes reporting severe hypoglycemia. Diabetes Care. 2012; 35:1897–901.
Article9. Mauvais-Jarvis F, Clegg DJ, Hevener AL. The role of estrogens in control of energy balance and glucose homeostasis. Endocr Rev. 2013; 34:309–38.
Article10. Briski KP, Nedungadi TP. Adaptation of feeding and counter-regulatory hormone responses to intermediate insulin-induced hypoglycaemia in the ovariectomised female rat: effects of oestradiol. J Neuroendocrinol. 2009; 21:578–85.
Article11. Guillaume M, Montagner A, Fontaine C, Lenfant F, Arnal JF, Gourdy P. Nuclear and membrane actions of estrogen receptor alpha: contribution to the regulation of energy and glucose homeostasis. Adv Exp Med Biol. 2017; 1043:401–26.
Article12. de Souza Santos R, Frank AP, Nelson MD, Garcia MM, Palmer BF, Clegg DJ. Sex, gender, and transgender: metabolic impact of cross hormone therapy. Adv Exp Med Biol. 2017; 1043:611–27.
Article13. Jung CH, Son JW, Kang S, Kim WJ, Kim HS, Kim HS, et al. Diabetes fact sheets in Korea, 2020: an appraisal of current status. Diabetes Metab J. 2021; 45:1–10.
Article14. Seong SC, Kim YY, Khang YH, Heon Park J, Kang HJ, Lee H, et al. Data resource profile: the National Health Information Database of the National Health Insurance Service in South Korea. Int J Epidemiol. 2017; 46:799–800.15. Kim HK, Song SO, Noh J, Jeong IK, Lee BW. Data configuration and publication trends for the Korean National Health Insurance and Health Insurance Review & Assessment Database. Diabetes Metab J. 2020; 44:671–8.
Article16. Takahashi TA, Johnson KM. Menopause. Med Clin North Am. 2015; 99:521–34.
Article17. Yun JS, Park YM, Han K, Cha SA, Ahn YB, Ko SH. Severe hypoglycemia and the risk of cardiovascular disease and mortality in type 2 diabetes: a nationwide population-based cohort study. Cardiovasc Diabetol. 2019; 18:103.
Article18. Yun JS, Ko SH. Current trends in epidemiology of cardiovascular disease and cardiovascular risk management in type 2 diabetes. Metabolism. 2021; 123:154838.
Article19. Lee SE, Kim KA, Son KJ, Song SO, Park KH, Park SH, et al. Trends and risk factors in severe hypoglycemia among individuals with type 2 diabetes in Korea. Diabetes Res Clin Pract. 2021; 178:108946.
Article20. Yun JS, Park YM, Han K, Kim HW, Cha SA, Ahn YB, et al. Severe hypoglycemia and the risk of end stage renal disease in type 2 diabetes. Sci Rep. 2021; 11:4305.
Article21. Yoo JE, Shin DW, Han K, Kim D, Yoon JW, Lee DY. Association of female reproductive factors with incidence of fracture among postmenopausal women in Korea. JAMA Netw Open. 2021; 4:e2030405.
Article22. Kim SK, Jang JY, Kim DL, Rhyu YA, Lee SE, Ko SH, et al. Site-specific cancer risk in patients with type 2 diabetes: a nationwide population-based cohort study in Korea. Korean J Intern Med. 2020; 35:641–51.
Article23. Han K, Yun JS, Park YM, Ahn YB, Cho JH, Cha SA, et al. Development and validation of a risk prediction model for severe hypoglycemia in adult patients with type 2 diabetes: a nationwide population-based cohort study. Clin Epidemiol. 2018; 10:1545–59.
Article24. UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998; 352:837–53.25. McCoy RG, Lipska KJ, Yao X, Ross JS, Montori VM, Shah ND. Intensive treatment and severe hypoglycemia among adults with type 2 diabetes. JAMA Intern Med. 2016; 176:969–78.
Article26. Workgroup on Hypoglycemia, American Diabetes Association. Defining and reporting hypoglycemia in diabetes: a report from the American Diabetes Association Workgroup on Hypoglycemia. Diabetes Care. 2005; 28:1245–9.27. Lee AK, Warren B, Lee CJ, McEvoy JW, Matsushita K, Huang ES, et al. The association of severe hypoglycemia with incident cardiovascular events and mortality in adults with type 2 diabetes. Diabetes Care. 2018; 41:104–11.
Article28. Frier BM, Schernthaner G, Heller SR. Hypoglycemia and cardiovascular risks. Diabetes Care. 2011; 34(Suppl 2):S132–7.
Article29. Davis SN, Fowler S, Costa F. Hypoglycemic counterregulatory responses differ between men and women with type 1 diabetes. Diabetes. 2000; 49:65–72.
Article30. The DCCT Research Group. Epidemiology of severe hypoglycemia in the diabetes control and complications trial. Am J Med. 1991; 90:450–9.31. Davis SN, Shavers C, Costa F. Gender-related differences in counterregulatory responses to antecedent hypoglycemia in normal humans. J Clin Endocrinol Metab. 2000; 85:2148–57.
Article32. Briski KP, Alhamami HN, Alshamrani A, Mandal SK, Shakya M, Ibrahim MH. Sex differences and role of estradiol in hypoglycemia-associated counter-regulation. Adv Exp Med Biol. 2017; 1043:359–83.
Article33. Bremer JP, Baron M, Peters H, Oltmanns KM, Kern W, Fehm HL, et al. Hormonal, subjective, and neurocognitive responses to brief hypoglycemia in postmenopausal women and age-matched men with type 2 diabetes mellitus. Metabolism. 2006; 55:331–8.
Article34. Seale JV, Wood SA, Atkinson HC, Harbuz MS, Lightman SL. Gonadal steroid replacement reverses gonadectomy-induced changes in the corticosterone pulse profile and stress-induced hypothalamic-pituitary-adrenal axis activity of male and female rats. J Neuroendocrinol. 2004; 16:989–98.
Article35. Paranjape SA, Briski KP. Recurrent insulin-induced hypoglycemia causes site-specific patterns of habituation or amplification of CNS neuronal genomic activation. Neuroscience. 2005; 130:957–70.
Article36. Nedungadi TP, Goleman WL, Paranjape SA, Kale AY, Briski KP. Effects of estradiol on glycemic and CNS neuronal activational responses to recurrent insulin-induced hypoglycemia in the ovariectomized female rat. Neuroendocrinology. 2006; 84:235–42.
Article37. Salpeter SR, Walsh JM, Ormiston TM, Greyber E, Buckley NS, Salpeter EE. Meta-analysis: effect of hormone-replacement therapy on components of the metabolic syndrome in postmenopausal women. Diabetes Obes Metab. 2006; 8:538–54.
Article38. Manson JE, Chlebowski RT, Stefanick ML, Aragaki AK, Rossouw JE, Prentice RL, et al. Menopausal hormone therapy and health outcomes during the intervention and extended poststopping phases of the Women’s Health Initiative randomized trials. JAMA. 2013; 310:1353–68.
Article39. Cignarella A, Kratz M, Bolego C. Emerging role of estrogen in the control of cardiometabolic disease. Trends Pharmacol Sci. 2010; 31:183–9.
Article40. Mauvais-Jarvis F, Manson JE, Stevenson JC, Fonseca VA. Menopausal hormone therapy and type 2 diabetes prevention: evidence, mechanisms, and clinical implications. Endocr Rev. 2017; 38:173–88.
Article41. Hodis HN, Mack WJ. Hormone replacement therapy and the association with coronary heart disease and overall mortality: clinical application of the timing hypothesis. J Steroid Biochem Mol Biol. 2014; 142:68–75.
Article42. Pereira RI, Casey BA, Swibas TA, Erickson CB, Wolfe P, Van Pelt RE. Timing of estradiol treatment after menopause may determine benefit or harm to insulin action. J Clin Endocrinol Metab. 2015; 100:4456–62.
Article43. Wend K, Wend P, Krum SA. Tissue-specific effects of loss of estrogen during menopause and aging. Front Endocrinol (Lausanne). 2012; 3:19.
Article44. Barros RP, Gabbi C, Morani A, Warner M, Gustafsson JA. Participation of ERalpha and ERbeta in glucose homeostasis in skeletal muscle and white adipose tissue. Am J Physiol Endocrinol Metab. 2009; 297:E124–33.45. Darko DA, Dornhorst A, Kennedy G, Mandeno RC, Seed M. Glycaemic control and plasma lipoproteins in menopausal women with type 2 diabetes treated with oral and transdermal combined hormone replacement therapy. Diabetes Res Clin Pract. 2001; 54:157–64.
Article46. Stojanovic ND, Kwong P, Byrne DJ, Arnold A, Jagroop IA, Nair D, et al. The effects of transdermal estradiol alone or with cyclical dydrogesterone on markers of cardiovascular disease risk in postmenopausal women with type 2 diabetes: a pilot study. Angiology. 2003; 54:391–9.
Article47. Bean JA, Leeper JD, Wallace RB, Sherman BM, Jagger H. Variations in the reporting of menstrual histories. Am J Epidemiol. 1979; 109:181–5.
Article48. Colditz GA, Stampfer MJ, Willett WC, Stason WB, Rosner B, Hennekens CH, et al. Reproducibility and validity of self-reported menopausal status in a prospective cohort study. Am J Epidemiol. 1987; 126:319–25.
Article49. Langer RD, Hodis HN, Lobo RA, Allison MA. Hormone replacement therapy: where are we now? Climacteric. 2021; 24:3–10.50. Hammar ML, van de Weijer P, Franke HR, Pornel B, von Mauw EM, Nijland EA, et al. Tibolone and low-dose continuous combined hormone treatment: vaginal bleeding pattern, efficacy and tolerability. BJOG. 2007; 114:1522–9.
Article51. Kyvernitakis I, Kostev K, Hars O, Albert US, Hadji P. Discontinuation rates of menopausal hormone therapy among postmenopausal women in the post-WHI study era. Climacteric. 2015; 18:737–42.
Article52. Kim C. Management of cardiovascular risk in perimenopausal women with diabetes. Diabetes Metab J. 2021; 45:492–501.
Article53. Kang BM, Kim MR, Park HM, Yoon BK, Lee BS, Chung HW, et al. Attitudes of Korean clinicians to postmenopausal hormone therapy after the Women’s Health Initiative study. Menopause. 2006; 13:125–9.
Article54. Kim MK, Jung YS, Chon SJ, Yun BH, Cho S, Choi YS, et al. Common causes of postmenopausal bleeding in Korean women: 10-year outcomes from a single medical center. J Korean Med Sci. 2017; 32:830–4.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Risk Factors and Adverse Outcomes of Severe Hypoglycemia in Type 2 Diabetes Mellitus
- Patient Education to Prevent Hypoglycemia
- Treatment Strategy to Prevent Hypoglycemia
- Severe hypoglycemia as a preventable risk factor for cardiovascular disease in patients with type 2 diabetes mellitus
- Avoiding or coping with severe hypoglycemia in patients with type 2 diabetes