Arch Hand Microsurg.
2022 Jun;27(2):154-160. 10.12790/ahm.22.0003.
Nail sparing and sub-nail bed approach for the excision of subungual glomus tumors
- Affiliations
-
- 1Department of Orthopaedic Surgery, Korea University College of Medicine, Seoul, Korea
- KMID: 2531922
- DOI: http://doi.org/10.12790/ahm.22.0003
Abstract
- Purpose
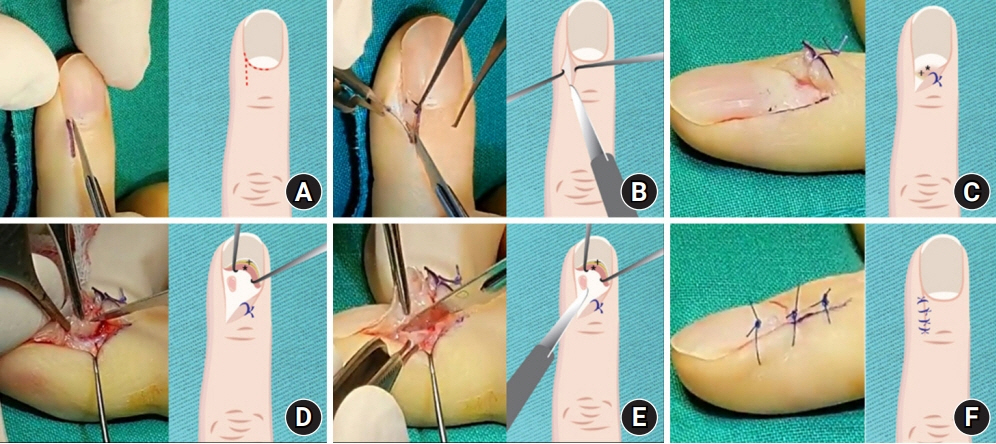
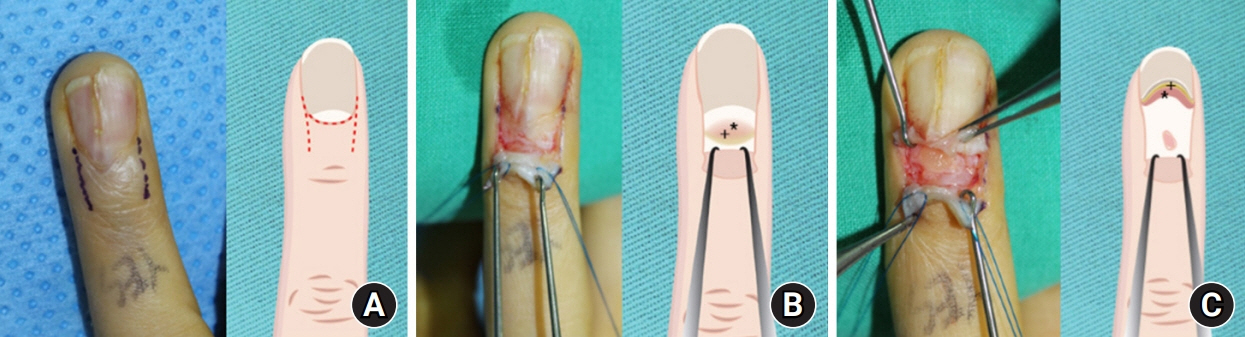
The excision of subungual glomus tumors on the distal phalanx may cause nail deformities. Herein, we report our nail-sparing and sub-nail bed approach for the excision of subungual glomus tumors, which enables subungual glomus tumor excision without removal of the nail plate and further allows access to the tumor mass by dissecting beneath the nail bed and germinal matrix to minimize postoperative pain and nail bed injury. Therefore, the present article describes this operative approach and reports surgical outcomes with respect to patient satisfaction, pain, and the final postoperative nail shape.
Methods
Thirty-two cases of clinically diagnosed subungual glomus tumors treated with this approach were retrospectively evaluated. Mean pain scores were measured at 1 week postoperatively and at the last follow-up. Patients were asked for their subjective opinion regarding the final nail shape, and their responses were assessed as “satisfied” or “unsatisfied.” The objective results for the final nail shape were graded as “excellent,” “good,” or “poor” by two orthopedic hand surgeons.
Results
The mean postoperative pain score (visual analog scale) at 1 week was 1.8. No patients reported pain at the last follow-up. Subjectively, 96.6% of patients were satisfied with the operation. Objectively, the postoperative nail shape was excellent in 9.3% of cases, good in 87.5%, and poor in 3.1%.
Conclusion
This approach provides minimal postoperative pain, high patient satisfaction, and favorable cosmetic outcomes with respect to the nail shape by avoiding removal of the nail plate and incision of the nail bed and germinal matrix.
Figure
Reference
-
References
1. Walsh JJ 4th, Eady JL. Vascular tumors. Hand Clin. 2004; 20:261–8.
Article2. Samaniego E, Crespo A, Sanz A. Key diagnostic features and treatment of subungual glomus tumor. Actas Dermosifiliogr. 2009; 100:875–82.
Article3. Willard KJ, Cappel MA, Kozin SH, Abzug JM. Congenital and infantile skin lesions affecting the hand and upper extremity, part 1: vascular neoplasms and malformations. J Hand Surg Am. 2013; 38:2271–83.
Article4. Lee W, Kwon SB, Cho SH, Eo SR, Kwon C. Glomus tumor of the hand. Arch Plast Surg. 2015; 42:295–301.
Article5. Bharathi RR, Bajantri B. Nail bed injuries and deformities of nail. Indian J Plast Surg. 2011; 44:197–202.
Article6. Tada H, Hirayma T, Takemitsu Y. Prevention of postoperative nail deformity after subungual glomus resection. J Hand Surg Am. 1994; 19:500–3.
Article7. Van Geertruyden J, Lorea P, Goldschmidt D, de Fontaine S, Schuind F, Kinnen L, et al. Glomus tumours of the hand. A retrospective study of 51 cases. J Hand Surg Br. 1996; 21:257–60.8. Fong ST, Lam YL, So YC. A modified periungual approach for treatment of subungual glomus tumour. Hand Surg. 2007; 12:217–21.
Article9. Gandon F, Legaillard P, Brueton R, Le Viet D, Foucher G. Forty-eight glomus tumours of the hand. Retrospective study and four-year follow-up. Ann Chir Main Memb Super. 1992; 11:401–5.10. Lee IJ, Park DH, Park MC, Pae NS. Subungual glomus tumours of the hand: diagnosis and outcome of the transungual approach. J Hand Surg Eur Vol. 2009; 34:685–8.
Article11. Love JG. Glomus tumors: diagnosis and treatment. Proc Staff Meet Mayo Clin. 1944; 19:113–6.12. Morey VM, Garg B, Kotwal PP. Glomus tumours of the hand: review of literature. J Clin Orthop Trauma. 2016; 7:286–91.
Article13. Tomak Y, Akcay I, Dabak N, Eroglu L. Subungual glomus tumours of the hand: diagnosis and treatment of 14 cases. Scand J Plast Reconstr Surg Hand Surg. 2003; 37:121–4.
Article14. Grover C, Khurana A, Jain R, Rathi V. Transungual surgical excision of subungual glomus tumour. J Cutan Aesthet Surg. 2013; 6:196–203.
Article15. Takata H, Ikuta Y, Ishida O, Kimori K. Treatment of subungual glomus tumour. Hand Surg. 2001; 6:25–7.
Article16. Jawalkar H, Maryada VR, Brahmajoshyula V, Kotha GK. Subungual glomus tumors of the hand: treated by transungual excision. Indian J Orthop. 2015; 49:403–7.17. Lee HJ, Kim PT, Kyung HS, Kim HS, Jeon IH. Nail-preserving excision for subungual glomus tumour of the hand. J Plast Surg Hand Surg. 2014; 48:201–4.
Article18. Vasisht B, Watson HK, Joseph E, Lionelli GT. Digital glomus tumors: a 29-year experience with a lateral subperiosteal approach. Plast Reconstr Surg. 2004; 114:1486–9.
Article19. Rosner IA, Argenta AE, Washington KM. Unusual volar pulp location of glomus tumor. Plast Reconstr Surg Glob Open. 2017; 5:e1215.
Article20. Madhar M, Bouslous J, Saidi H, Fikry T, Schuind F. Which approach is best for subungual glomus tumors? Transungual with microsurgical dissection of the nail bed or periungual? Chir Main. 2015; 34:39–43.
Article21. Santoshi JA, Kori VK, Khurana U. Glomus tumor of the fingertips: a frequently missed diagnosis. J Family Med Prim Care. 2019; 8:904–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Subungual Glomus Tumor Resection with Partial Detachment of Nail Plate
- A Case of Subungual Epidermal Cyst
- Clinical and Histopathological Analyses of Glomus Tumors: An Institutional Experience of 29 Cases
- Diagnosis and Preoperative Evaluation of Subungual Glomus Tumors Using Ultrasound
- Reconstruction of the Defect with Dermal Graft After the Removal of Subungual Squamous Cell Carcinoma