Anesth Pain Med.
2022 Apr;17(2):165-172. 10.17085/apm.21068.
Association between anesthetic method and postpartum hemorrhage in Korea based on National Health Insurance Service data
- Affiliations
-
- 1Advanced Biomedical Research Institute, Ewha Womans University Seoul Hospital, Seoul, Korea
- 2Department of Anesthesiology and Pain Medicine, Ewha Womans University College of Medicine, Seoul, Korea
- KMID: 2531692
- DOI: http://doi.org/10.17085/apm.21068
Abstract
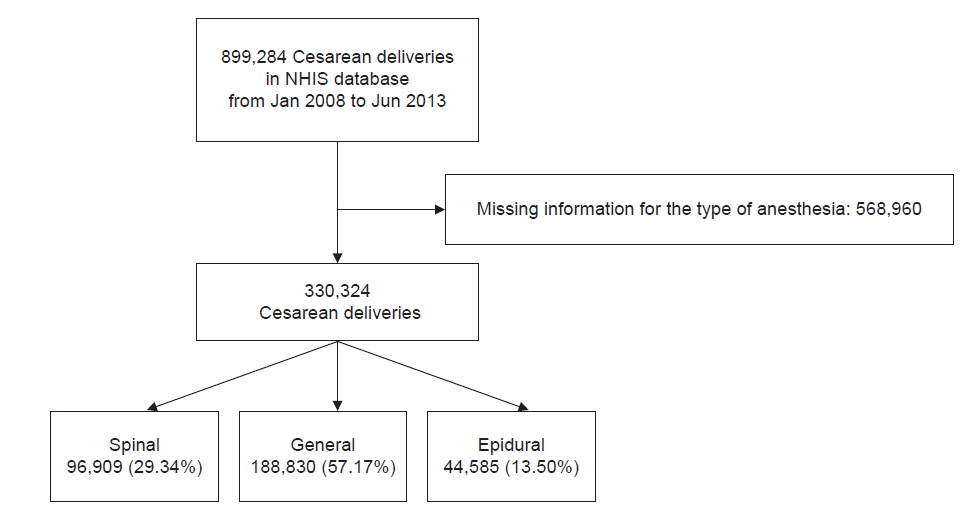
- Background
Postpartum hemorrhage (PPH) is a major cause of maternal mortality and the risk factors for PPH differ among studies. In this large-scale study, we investigated whether the anesthetic method used was associated with PPH after cesarean section. Methods: We extracted data on cesarean sections performed between January 2008 and June 2013 from the National Health Insurance Service database. The anesthetic methods were categorized into general, spinal and epidural anesthesia. To compare the likelihood of PPH among deliveries using different anesthetic methods, crude and adjusted odds ratios (ORs) and 95% confidence intervals were calculated using logistic regression analysis. Results: Data from 330,324 cesarean sections were analyzed, and 21,636 cases of PPH were identified. Univariate analysis showed that general and epidural anesthesia increased the risk of PPH compared to spinal anesthesia. The OR for PPH was highest for morbidly adherent placenta, followed by placenta previa, placental abruption, and hypertension. When other clinical covariates were controlled for, general and epidural anesthesia still remained significant risk factors for PPH compared to spinal anesthesia. Conclusions: This study showed that general and epidural anesthesia elevated the risk of PPH compared to spinal anesthesia during cesarean section. Since we could not consider the potential bias of group differences in indications, more in-depth clinical trials are needed to validate our findings. Obstetric factors such as placental abnormalities had high odds ratios and thus are more important than the choice of anesthetic method, which should be based on the patient’s clinical condition and institutional resources.
Figure
Cited by 1 articles
-
Risk factors for severe postpartum hemorrhage requiring blood transfusion after cesarean delivery for twin pregnancy: a nationwide cohort study
Gi Hyeon Seo, Jong Yeop Kim, Da Yeong Lee, Changjin Lee, Jiyoung Lee
Anesth Pain Med. 2023;18(4):367-375. doi: 10.17085/apm.23019.
Reference
-
1. van Stralen G, von Schmidt Auf Altenstadt JF, Bloemenkamp KW, van Roosmalen J, Hukkelhoven CW. Increasing incidence of postpartum hemorrhage: the Dutch piece of the puzzle. Acta Obstet Gynecol Scand. 2016; 95:1104–10.
Article2. Reale SC, Easter SR, Xu X, Bateman BT, Farber MK. Trends in postpartum hemorrhage in the United States from 2010 to 2014. Anesth Analg. 2020; 130:e119–22.
Article3. Yildiz K, Dogru K, Dalgic H, Serin IS, Sezer Z, Madenoglu H, et al. Inhibitory effects of desflurane and sevoflurane on oxytocin-induced contractions of isolated pregnant human myometrium. Acta Anaesthesiol Scand. 2005; 49:1355–9.
Article4. Kawakita T, Mokhtari N, Huang JC, Landy HJ. Evaluation of risk-assessment tools for severe postpartum hemorrhage in women undergoing cesarean delivery. Obstet Gynecol. 2019; 134:1308–16.
Article5. Butwick AJ, Ramachandran B, Hegde P, Riley ET, El-Sayed YY, Nelson LM. Risk factors for severe postpartum hemorrhage after cesarean delivery: case-control studies. Anesth Analg. 2017; 125:523–32.6. Park JI, Park SH, Kang MS, Kang GW, Kim ST. Evaluation of changes in anesthetic methods for cesarean delivery: an analysis for 5 years using the big data of the Korean Health Insurance Review and Assessment Service. Anesth Pain Med (Seoul). 2020; 15:305–13.
Article7. Wong CA. General anesthesia is unacceptable for elective cesarean section. Int J Obstet Anesth. 2010; 19:209–12.
Article8. Juang J, Gabriel RA, Dutton RP, Palanisamy A, Urman RD. Choice of anesthesia for cesarean delivery: an analysis of the national anesthesia clinical outcomes registry. Anesth Analg. 2017; 124:1914–7.9. Butwick AJ, Palanisamy A. Mode of anaesthesia for caesarean delivery and maternal morbidity: can we overcome confounding by indication? Br J Anaesth. 2018; 120:621–3.
Article10. Dogru K, Dalgic H, Yildiz K, Sezer Z, Madenoglu H. The direct depressant effects of desflurane and sevoflurane on spontaneous contractions of isolated gravid rat myometrium. Int J Obstet Anesth. 2003; 12:74–8.
Article11. Beilin Y. Maternal hemorrhage-regional versus general anesthesia: does it really matter? Anesth Analg. 2018; 127:805–7.12. Rouse DJ, MacPherson C, Landon M, Varner MW, Leveno KJ, Moawad AH, et al. National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Blood transfusion and cesarean delivery. Obstet Gynecol. 2006; 108:891–7.13. Guay J. The effect of neuraxial blocks on surgical blood loss and blood transfusion requirements: a meta-analysis. J Clin Anesth. 2006; 18:124–8.
Article14. Afolabi BB, Lesi FE. Regional versus general anaesthesia for caesarean section. Cochrane Database Syst Rev. 2012; 10:CD004350.
Article15. Sung TY, Jee YS, You HJ, Cho CK. Comparison of the effect of general and spinal anesthesia for elective cesarean section on maternal and fetal outcomes: a retrospective cohort study. Anesth Pain Med (Seoul). 2021; 16:49–55.
Article16. Elena R, Pamela F, Mrinalini B. Effects of anesthesia on uterine activity, progress in labor and outcomes. Shnider and Levinson's: anesthesia for obstetrics. 5th ed. In : Suresh MS, Segal S, Preston RL, Fernando R, LaToya Mason C, editors. Philadelphia (PA): Lippincott Williams & Wilkins;2013. p. 156.17. Hawkins JL. Excess in moderation: general anesthesia for cesarean delivery. Anesth Analg. 2015; 120:1175–7.18. Qian X, Li P, Shi SQ, Garfield RE, Liu H. Uterine and abdominal muscle electromyographic activities in control and PCEA-treated nulliparous women during the second stage of labor. Reprod Sci. 2017; 24:1214–20.
Article19. Ng K, Parsons J, Cyna AM, Middleton P. Spinal versus epidural anaesthesia for caesarean section. Cochrane Database Syst Rev. 2004; 2:CD003765.
Article20. Schewe JC, Komusin A, Zinserling J, Nadstawek J, Hoeft A, Hering R. Effects of spinal anaesthesia versus epidural anaesthesia for caesarean section on postoperative analgesic consumption and postoperative pain. Eur J Anaesthesiol. 2009; 26:52–9.
Article21. Zhang J, Troendle J, Reddy UM, Laughon SK, Branch DW, Burkman R, et al. Consortium on Safe Labor. Contemporary cesarean delivery practice in the United States. Am J Obstet Gynecol. 2010; 203:326.e1–10.22. Bateman BT, Berman MF, Riley LE, Leffert LR. The epidemiology of postpartum hemorrhage in a large, nationwide sample of deliveries. Anesth Analg. 2010; 110:1368–73.
Article23. Nyfløt LT, Sandven I, Stray-Pedersen B, Pettersen S, Al-Zirqi I, Rosenberg M, et al. Risk factors for severe postpartum hemorrhage: a case-control study. BMC Pregnancy Childbirth. 2017; 17:17.
Article24. Belghiti J, Kayem G, Dupont C, Rudigoz RC, Bouvier-Colle MH, Deneux-Tharaux C. Oxytocin during labour and risk of severe postpartum haemorrhage: a population-based, cohort-nested case-control study. BMJ Open. 2011; 1:e000514.
Article25. Mhyre JM, Shilkrut A, Kuklina EV, Callaghan WM, Creanga AA, Kaminsky S, et al. Massive blood transfusion during hospitalization for delivery in New York State, 1998-2007. Obstet Gynecol. 2013; 122:1288–94.
Article26. Masuzawa Y, Yaeko K. Uterine activity during the two hours after placental delivery among low-risk pregnancies: an observational study. J Matern Fetal Neonatal Med. 2017; 30:2446–51.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Overview of Postpartum Hemorrhage Project
- Evaluation of changes in anesthetic methods for cesarean delivery: an analysis for 5 years using the big data of the Korean Health Insurance Review and Assessment Service
- Maternal Health Effects of Internet-Based Education Interventions during the Postpartum Period: A Systematic Review
- A guide for the utilization of Health Insurance Review and Assessment Service National Patient Samples
- Distribution of Medical Service Use for Facial Palsy Between Medicine and Traditional Korean Medicine Based on Population-Based Data of Korea