Acute Crit Care.
2022 May;37(2):258-262. 10.4266/acc.2021.00290.
Acute perimyocarditis mimicking acute myocardial infarction in a 12-year-old boy with duchenne muscular dystrophy
- Affiliations
-
- 1Department of Pediatrics, Seoul National University Hospital, Seoul, Korea
- KMID: 2531685
- DOI: http://doi.org/10.4266/acc.2021.00290
Abstract
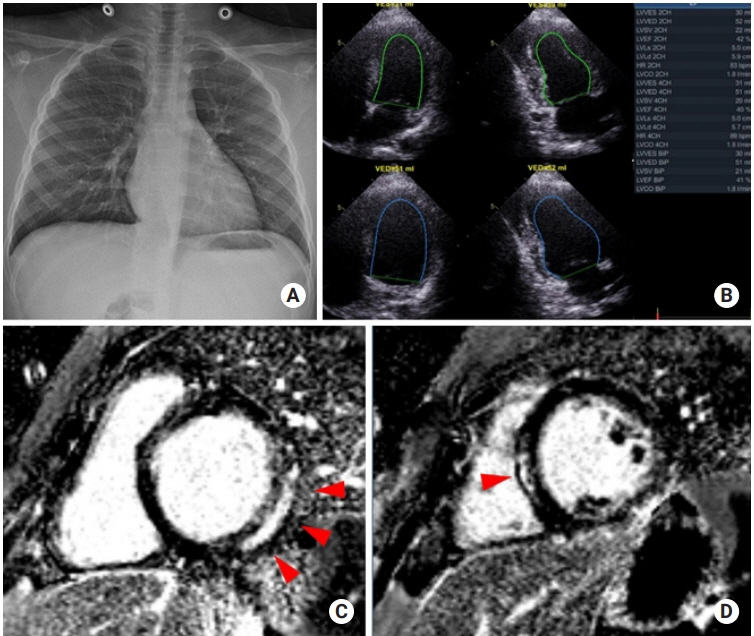
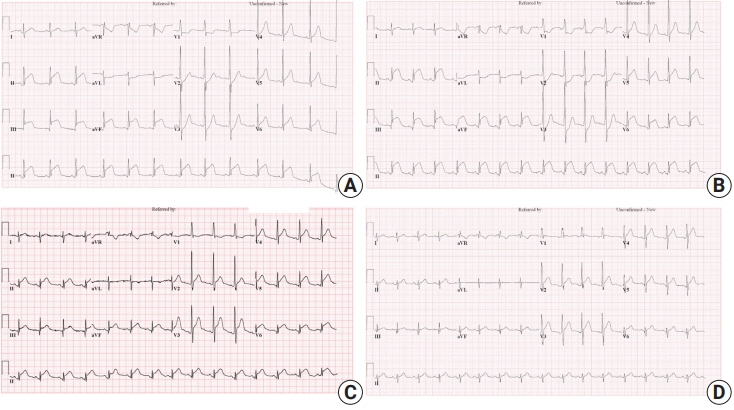
- Differential diagnosis of chest pain in the pediatric population is important but can be challenging. A 12-year-old boy with Duchenne muscular dystrophy presented with chest pain, cardiac enzyme elevation, and convex ST elevations in the inferior leads with reciprocal ST depression in the anterior leads on electrocardiogram. Echocardiography on admission revealed normal left ventricular function. Suspecting acute myocardial infarction, we performed invasive coronary angiography, which revealed normal coronary arteries. A follow-up electrocardiogram showed an acute pericarditis pattern with concave ST elevations in most leads and PR depression, and follow-up echocardiography revealed global left ventricular dysfunction, suggestive of acute perimyocarditis. Ibuprofen was administered for acute pericarditis, and a continuous milrinone infusion was commenced for myocardial dysfunction. The chest pain improved by the next day, and the ST segment elevations normalized on day 4. Echocardiography on day 9 revealed improved left ventricular function. The patient was discharged on day 11, and he is doing well without chest pain through 12 months of follow-up. The last electrocardiogram showed normal sinus rhythm without ST change. Differential diagnosis of acute myocardial infarction and acute perimyocarditis is important for proper treatment strategies and the different prognoses of these two conditions.
Figure
Reference
-
1. de Bliek EC. ST elevation: differential diagnosis and caveats. A comprehensive review to help distinguish ST elevation myocardial infarction from nonischemic etiologies of ST elevation. Turk J Emerg Med. 2018; 18:1–10.
Article2. Deshpande A, Birnbaum Y. ST-segment elevation: distinguishing ST elevation myocardial infarction from ST elevation secondary to nonischemic etiologies. World J Cardiol. 2014; 6:1067–79.
Article3. Adler Y, Charron P, Imazio M, Badano L, Barón-Esquivias G, Bogaert J, et al. 2015 ESC Guidelines for the diagnosis and management of pericardial diseases: The Task Force for the Diagnosis and Management of Pericardial Diseases of the European Society of Cardiology (ESC)endorsed by: The European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2015; 36:2921–64.4. Kindermann I, Barth C, Mahfoud F, Ukena C, Lenski M, Yilmaz A, et al. Update on myocarditis. J Am Coll Cardiol. 2012; 59:779–92.
Article5. Cooper LT, Baughman KL, Feldman AM, Frustaci A, Jessup M, Kuhl U, et al. The role of endomyocardial biopsy in the management of cardiovascular disease: a scientific statement from the American Heart Association, the American College of Cardiology, and the European Society of Cardiology Endorsed by the Heart Failure Society of America and the Heart Failure Association of the European Society of Cardiology. Eur Heart J. 2007; 28:3076–93.
Article6. Bozkurt B, Colvin M, Cook J, Cooper LT, Deswal A, Fonarow GC, et al. Current diagnostic and treatment strategies for specific dilated cardiomyopathies: a scientific statement from the American Heart Association. Circulation. 2016; 134:e579–646.
Article7. Sagar S, Liu PP, Cooper LT Jr. Myocarditis. Lancet. 2012; 379:738–47.
Article8. Liu PP, Mason JW. Advances in the understanding of myocarditis. Circulation. 2001; 104:1076–82.
Article9. Nigro G, Comi LI, Politano L, Bain RJ. The incidence and evolution of cardiomyopathy in Duchenne muscular dystrophy. Int J Cardiol. 1990; 26:271–7.
Article10. Verhaert D, Richards K, Rafael-Fortney JA, Raman SV. Cardiac involvement in patients with muscular dystrophies: magnetic resonance imaging phenotype and genotypic considerations. Circ Cardiovasc Imaging. 2011; 4:67–76.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Acute Gastric Dilatation and Calculous Cholecystitis in Duchenne's Muscular Dystrophy
- Duchenne Muscular Dystrophy Complicated With Dilated Cardiomyopathy and Cerebral Infarction
- Acute Cerebral Infarction and Epilepsy in Duchenne Muscular Dystrophy
- A clinical study on Duchenne muscular dystrophy
- A Case of Progressive Muscular Dystrophy ( Duchenne type )