Acute Crit Care.
2022 May;37(2):247-255. 10.4266/acc.2021.01396.
Determination of risk factors associated with surgical site infection in patients undergoing preperitoneal pelvic packing for unstable pelvic fracture
- Affiliations
-
- 1Department of Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea
- 2Department of Surgery, Yonsei University Wonju College of Medicine, Wonju, Korea
- 3Trauma Center, Wonju Severance Christian Hospital, Wonju, Korea
- 4Wonju Severance Pelvic Bone Research Group, Yonsei University Wonju College of Medicine, Wonju, Korea
- 5Department of Surgery, Trauma Center, National Health Insurance Service Ilsan Hospital, Goyang, Korea
- KMID: 2531683
- DOI: http://doi.org/10.4266/acc.2021.01396
Abstract
- Background
Several recent studies have shown that preperitoneal pelvic packing (PPP) effectively produces hemostasis in patients with unstable pelvic fractures. However, few studies have examined the rate of surgical site infections (SSIs) in patients undergoing PPP following an unstable pelvic fracture. The purpose of the present study was to evaluate factors associated with SSI in such patients.
Methods
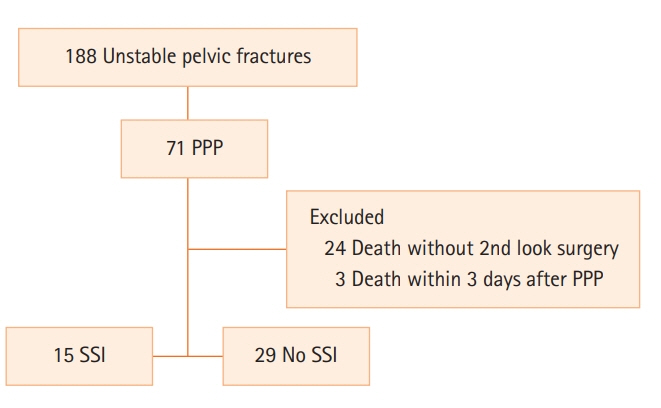
We retrospectively reviewed the medical charts of 188 patients who developed hemorrhagic shock due to pelvic fracture between April 2012 and May 2021. Forty-four patients were enrolled in this study.
Results
SSI occurred in 15 of 44 patients (34.1%). The SSIs occurred more frequently in cases of repacking during the second-look surgery (0 vs. 4 [26.7%], P=0.010) and combined bladder-urethra injury (1 [3.4%] vs. 4 [26.7%], P=0.039). The incidence of SSIs was not significantly different between patients undergoing depacking within or after 48 hours (12 [41.4%] vs. 5 [33.3%], P=0.603). The mean time to diagnosis of SSI was 8.1±3.9 days from PPP. The most isolated organism was Staphylococcus epidermidis.
Conclusions
Repacking and combined bladder-urethra injury are potential risk factors for SSI in patients with unstable pelvic fracture. Close observation is recommended for up to 8 days in patients with these risk factors. Further, 48 hours after PPP, removing the packed gauze on cessation of bleeding and not performing repacking can help prevent SSI. Additional analyses are necessary with a larger number of patients with the potential risk factors identified in this study.
Figure
Reference
-
1. Costantini TW, Coimbra R, Holcomb JB, Podbielski JM, Catalano R, Blackburn A, et al. Current management of hemorrhage from severe pelvic fractures: results of an American Association for the Surgery of Trauma multi-institutional trial. J Trauma Acute Care Surg. 2016; 80:717–23.2. Kim TH, Yoon YC, Chung JY, Song HK. Strategies for the management of hemodynamically unstable pelvic fractures: from preperitoneal pelvic packing to definitive internal fixation. Asian J Surg. 2019; 42:941–6.
Article3. Pohlemann T, Gänsslen A, Bosch U, Tscherne H. The technique of packing for control of hemorrhage in complex pelvis fractures. Tech Orthop. 1995; 9:267–70.4. Stahel PF, Moore EE, Burlew CC, Henderson C, Peña AJ, Harry D, et al. Preperitoneal pelvic packing is not associated with an increased risk of surgical site infections after internal anterior pelvic ring fixation. J Orthop Trauma. 2019; 33:601–7.
Article5. Smith WR, Moore EE, Osborn P, Agudelo JF, Morgan SJ, Parekh AA, et al. Retroperitoneal packing as a resuscitation technique for hemodynamically unstable patients with pelvic fractures: report of two representative cases and a description of technique. J Trauma. 2005; 59:1510–4.
Article6. Burlew CC, Moore EE, Stahel PF, Geddes AE, Wagenaar AE, Pieracci FM, et al. Preperitoneal pelvic packing reduces mortality in patients with life-threatening hemorrhage due to unstable pelvic fractures. J Trauma Acute Care Surg. 2017; 82:233–42.
Article7. Moskowitz EE, Burlew CC, Moore EE, Pieracci FM, Fox CJ, Campion EM, et al. Preperitoneal pelvic packing is effective for hemorrhage control in open pelvic fractures. Am J Surg. 2018; 215:675–7.
Article8. Petrone P, Rodríguez-Perdomo M, Pérez-Jiménez A, Ali F, Brathwaite C, Joseph DK. Pre-peritoneal pelvic packing for the management of life-threatening pelvic fractures. Eur J Trauma Emerg Surg. 2019; 45:417–21.
Article9. Dessie W, Mulugeta G, Fentaw S, Mihret A, Hassen M, Abebe E. Pattern of bacterial pathogens and their susceptibility isolated from surgical site infections at selected referral hospitals, Addis Ababa, Ethiopia. Int J Microbiol. 2016; 2016:2418902.
Article10. Morales CH, Escobar RM, Villegas MI, Castaño A, Trujillo J. Surgical site infection in abdominal trauma patients: risk prediction and performance of the NNIS and SENIC indexes. Can J Surg. 2011; 54:17–24.
Article11. Isbell KD, Hatton GE, Wei S, Green C, Truong V, Woloski J, et al. Risk stratification for superficial surgical site infection after emergency trauma laparotomy. Surg Infect (Larchmt). 2021; 22:697–704.
Article12. Perkins ZB, Maytham GD, Koers L, Bates P, Brohi K, Tai NR. Impact on outcome of a targeted performance improvement programme in haemodynamically unstable patients with a pelvic fracture. Bone Joint J. 2014; 96:1090–7.
Article13. Coccolini F, Stahel PF, Montori G, Biffl W, Horer TM, Catena F, et al. Pelvic trauma: WSES classification and guidelines. World J Emerg Surg. 2017; 12:5.
Article14. National Healthcare Safety Network. Surgical site infection event (SSI) [Internet]. Atlanta (GA): Centers for Disease Control and Prevention; 2021 [Epub]. Available from: http://www.cdc.gov/nhsn/pdfs/pscmanual/9pscssicurrent.pdf.15. Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for prevention of surgical site infection, 1999. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol. 1999; 20:250–78.16. Hamasuna R, Betsunoh H, Sueyoshi T, Yakushiji K, Tsukino H, Nagano M, et al. Bacteria of preoperative urinary tract infections contaminate the surgical fields and develop surgical site infections in urological operations. Int J Urol. 2004; 11:941–7.
Article17. Keel M, Trentz O. Pathophysiology of polytrauma. Injury. 2005; 36:691–709.
Article18. Hietbrink F, Koenderman L, Rijkers G, Leenen L. Trauma: the role of the innate immune system. World J Emerg Surg. 2006; 1:15.19. Stahel PF, Smith WR, Moore EE. Role of biological modifiers regulating the immune response after trauma. Injury. 2007; 38:1409–22.
Article20. Hermans E, Edwards M, Goslings JC, Biert J. Open pelvic fracture: the killing fracture? J Orthop Surg Res. 2018; 13:83.
Article21. Siada SS, Davis JW, Kaups KL, Dirks RC, Grannis KA. Current outcomes of blunt open pelvic fractures: how modern advances in trauma care may decrease mortality. Trauma Surg Acute Care Open. 2017; 2:e000136.
Article22. Song W, Zhou D, Xu W, Zhang G, Wang C, Qiu D, et al. Factors of pelvic infection and death in patients with open pelvic fractures and rectal injuries. Surg Infect (Larchmt). 2017; 18:711–5.
Article23. Kim DH, Chang YR. Preperitoneal pelvic packing. Trauma Image Proc. 2017; 42–3.
Article24. Burlew CC, Moore EE, Smith WR, Johnson JL, Biffl WL, Barnett CC, et al. Preperitoneal pelvic packing/external fixation with secondary angioembolization: optimal care for life-threatening hemorrhage from unstable pelvic fractures. J Am Coll Surg. 2011; 212:628–35.
Article25. Leaper DJ. Risk factors for surgical infection. J Hosp Infect. 1995; 30 Suppl:127–39.
Article26. Li Q, Dong J, Yang Y, Wang G, Wang Y, Liu P, et al. Retroperitoneal packing or angioembolization for haemorrhage control of pelvic fractures: quasi-randomized clinical trial of 56 haemodynamically unstable patients with Injury Severity Score ≥33. Injury. 2016; 47:395–401.
Article27. Lai CY, Tseng IC, Su CY, Hsu YH, Chou YC, Chen HW, et al. High incidence of surgical site infection may be related to suboptimal case selection for non-selective arterial embolization during resuscitation of patients with pelvic fractures: a retrospective study. BMC Musculoskelet Disord. 2020; 21:335.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Preperitoneal Pelvic Packing Prior to Pelvic Angiography in Patients with Hemodynamic Instability due to Severe Pelvic Fracture: Two Cases
- Pelvic Bone Fracture with Preperitoneal Hemorrhage
- Determination of Risk Factors for Predicting Bladder-Urethra Injury in Cases of Pelvic Bone Fracture: A Retrospective Single Center Study
- Retroperitoneal Gauze Packing with Vacuum-Associated Closure for Pelvic Fracture with Hemodynamic Instability
- Preperitoneal pelvic packing for initial management of hemodynamically unstable pelvic fracture: a systematic review and meta-analysis