Acute Crit Care.
2022 May;37(2):230-236. 10.4266/acc.2021.00843.
Cinematic virtual reality for anxiety management in mechanically ventilated patients: a feasibility and pilot study
- Affiliations
-
- 1Integrative Health and Wellbeing Research Program at the Earl E. Bakken Center for Spirituality and Healing, University of Minnesota School of Nursing, Minneapolis, MN, USA
- 2Division of Pulmonary, Allergy, Critical Care and Sleep Medicine, Department of Internal Medicine, University of Minnesota Medical School, Minneapolis, MN, USA
- KMID: 2531681
- DOI: http://doi.org/10.4266/acc.2021.00843
Abstract
- Background
Mechanically ventilated patients experience anxiety for many reasons. Pharmacological treatments such as benzodiazepines are commonly employed to manage anxiety; however, these therapies often cause undesired side effects. Additional therapies for anxiety management are needed. We sought to determine whether cell phone-based virtual reality therapy could feasibly be used for anxiety management in mechanically ventilated patients.
Methods
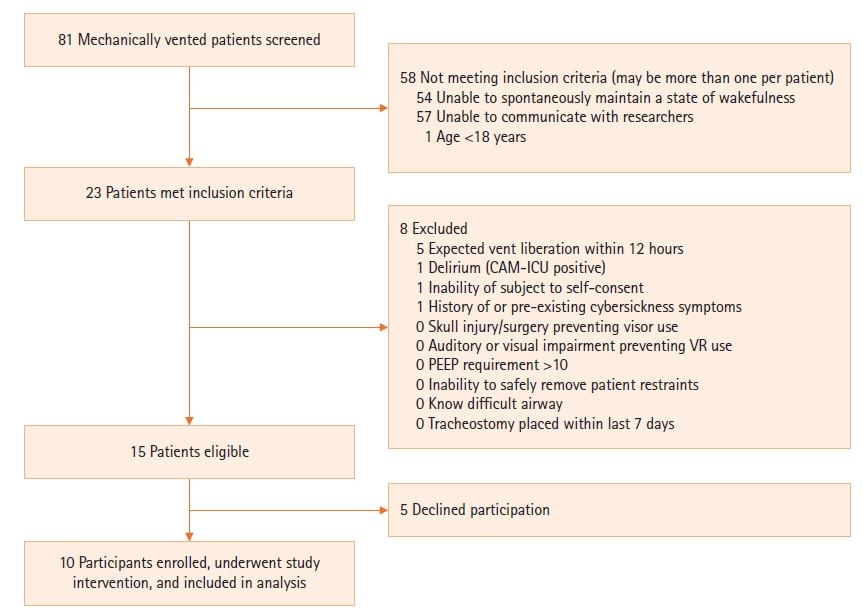
Mechanically ventilated subjects underwent at least one session of virtual reality therapy in which they were shown a cinematic video of an outdoor green space or blue space with 360° visual range of motion. Goal session duration was 5 minutes. The primary outcome was incidence of predefined patient safety events, including self-extubation and accidental removal of tubes or lines.
Results
Ten subjects underwent a total of 18 virtual reality sessions. Fifteen sessions lasted the planned 5 minutes, one session was extended at participant request, and two sessions were terminated early at participant request. There were no occurrences of the predefined safety events, and no occurrences of cybersickness. Use of a visual analog scale to measure anxiety level was feasible for this pilot study, demonstrating feasibility of this scale for future, larger scale studies.
Conclusions
Virtual reality therapy shows potential as a means of managing anxiety in patients undergoing mechanical ventilation, and further rigorous exploration with this protocol is feasible.
Keyword
Figure
Reference
-
1. Pandharipande PP, Pun BT, Herr DL, Maze M, Girard TD, Miller RR, et al. Effect of sedation with dexmedetomidine vs lorazepam on acute brain dysfunction in mechanically ventilated patients: the MENDS randomized controlled trial. JAMA. 2007; 298:2644–53.
Article2. Ludmir J, Netzer G. Go big: measuring and tackling psychological morbidity after critical illness. Ann Am Thorac Soc. 2016; 13:1217–8.
Article3. Nikayin S, Rabiee A, Hashem MD, Huang M, Bienvenu OJ, Turnbull AE, et al. Anxiety symptoms in survivors of critical illness: a systematic review and meta-analysis. Gen Hosp Psychiatry. 2016; 43:23–29.
Article4. Wunsch H, Christiansen CF, Johansen MB, Olsen M, Ali N, Angus DC, et al. Psychiatric diagnoses and psychoactive medication use among nonsurgical critically ill patients receiving mechanical ventilation. JAMA. 2014; 311:1133–42.
Article5. Parker AM, Sricharoenchai T, Raparla S, Schneck KW, Bienvenu OJ, Needham DM. Posttraumatic stress disorder in critical illness survivors: a metaanalysis. Crit Care Med. 2015; May. 43:1121–9.6. Lee CH, Lee CY, Hsu MY, Lai CL, Sung YH, Lin CY, et al. Effects of music intervention on state anxiety and physiological indices in patients undergoing mechanical ventilation in the intensive care unit. Biol Res Nurs. 2017; 19:137–44.
Article7. Mofredj A, Alaya S, Tassaioust K, Bahloul H, Mrabet A. Music therapy, a review of the potential therapeutic benefits for the critically ill. J Crit Care. 2016; 35:195–9.
Article8. Chlan LL, Weinert CR, Heiderscheit A, Tracy MF, Skaar DJ, Guttormson JL, et al. Effects of patient-directed music intervention on anxiety and sedative exposure in critically ill patients receiving mechanical ventilatory support: a randomized clinical trial. JAMA. 2013; 309:2335–44.
Article9. Faber AW, Patterson DR, Bremer M. Repeated use of immersive virtual reality therapy to control pain during wound dressing changes in pediatric and adult burn patients. J Burn Care Res. 2013; 34:563–8.
Article10. Markus LA, Willems KE, Maruna CC, Schmitz CL, Pellino TA, Wish JR, et al. Virtual reality: feasibility of implementation in a regional burn center. Burns. 2009; 35:967–9.
Article11. Small C, Stone R, Pilsbury J, Bowden M, Bion J. Virtual restorative environment therapy as an adjunct to pain control during burn dressing changes: study protocol for a randomised controlled trial. Trials. 2015; 16:329.
Article12. Nilsson S, Finnström B, Kokinsky E, Enskär K. The use of virtual reality for needle-related procedural pain and distress in children and adolescents in a paediatric oncology unit. Eur J Oncol Nurs. 2009; 13:102–9.
Article13. Mosso-Vázquez JL, Gao K, Wiederhold BK, Wiederhold MD. Virtual reality for pain management in cardiac surgery. Cyberpsychol Behav Soc Netw. 2014; 17:371–8.
Article14. Dascal J, Reid M, IsHak WW, Spiegel B, Recacho J, Rosen B, et al. Virtual reality and medical inpatients: a systematic review of randomized, controlled trials. Innov Clin Neurosci. 2017; 14:14–21.15. Turon M, Fernandez-Gonzalo S, Jodar M, Gomà G, Montanya J, Hernando D, et al. Feasibility and safety of virtual-reality-based early neurocognitive stimulation in critically ill patients. Ann Intensive Care. 2017; 7:81.
Article16. Weech S, Kenny S, Barnett-Cowan M. Presence and cybersickness in virtual reality are negatively related: a review. Front Psychol. 2019; 10:158.
Article17. Hoffmann MJ. FDA regulatory process. Silver Spring (MD): U.S. Food and Drug Administration;2021. [cited 2021 July 7]. Available from: https://www.fda.gov/media/90419/download.18. Rebenitsch L, Owen C. Review on cybersickness in applications and visual displays. Virtual Real. 2016; 20:101–25.
Article19. McMahan EA, Estes D. The effect of contact with natural environments on positive and negative affect: a meta-analysis. J Posit Psychol. 2015; 10:507–19.
Article20. Bruck S, Watters PA. Accessible virtual reality therapy using portable media devices. Stud Health Technol Inform. 2010; 154:87–91.21. Sricharoenchai T, Parker AM, Zanni JM, Nelliot A, Dinglas VD, Needham DM. Safety of physical therapy interventions in critically ill patients: a single-center prospective evaluation of 1110 intensive care unit admissions. J Crit Care. 2014; 29:395–400.
Article22. Chlan LL. Relationship between two anxiety instruments in patients receiving mechanical ventilatory support. J Adv Nurs. 2004; 48:493–9.
Article23. Gerber SM, Jeitziner MM, Wyss P, Chesham A, Urwyler P, Müri RM, et al. Visuo-acoustic stimulation that helps you to relax: a virtual reality setup for patients in the intensive care unit. Sci Rep. 2017; 7:13228.
Article24. Gerber SM, Jeitziner MM, Sänger SD, Knobel SEJ, Marchal-Crespo L, Müri RM, et al. Comparing the relaxing effects of different virtual reality environments in the intensive care unit: observational study. JMIR Perioper Med. 2019; 2:e15579.
Article25. Ong TL, Ruppert MM, Akbar M, Rashidi P, Ozrazgat-Baslanti T, Bihorac A, et al. Improving the intensive care patient experience with virtual reality-a feasibility study. Crit Care Explor. 2020; 2:e0122.
Article26. Lee JH, Lee HC, Jeon YT, Hwang JW, Lee H, Oh HW, et al. Clinical outcomes after unplanned extubation in a surgical intensive care population. World J Surg. 2014; 38:203–10.
Article27. Kiekkas P, Aretha D, Panteli E, Baltopoulos GI, Filos KS. Unplanned extubation in critically ill adults: clinical review. Nurs Crit Care. 2013; 18:123–34.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Virtual Reality in Current and Future Psychiatry
- The digital literacy, awareness, and educational needs of virtual reality among nursing students
- Effect of Virtual Reality Distraction on Pain and Anxiety in Children during Local Anesthesia
- Two Cases of Posttraumatic Stress Disorder Caused by a Motor Vehicle Accident Treated with Virtual Reality Exposure Therapy
- Home-based walking intervention for middle-aged migrant women using 360-degree virtual videos and a wearable activity tracker: A mixed-methods pilot study