J Korean Neurosurg Soc.
2022 Jul;65(4):603-608. 10.3340/jkns.2021.0222.
Extracranial Carotid-Vertebral Artery Bypass Technique and Surgical Outcomes
- Affiliations
-
- 1Department of Neurosurgery, Seoul St. Mary’s Hospital, The Catholic University of Korea, Seoul, Korea
- 2Department of Neurosurgery, Bucheon St. Mary’s Hospital, The Catholic University of Korea, Seoul, Korea
- KMID: 2531630
- DOI: http://doi.org/10.3340/jkns.2021.0222
Abstract
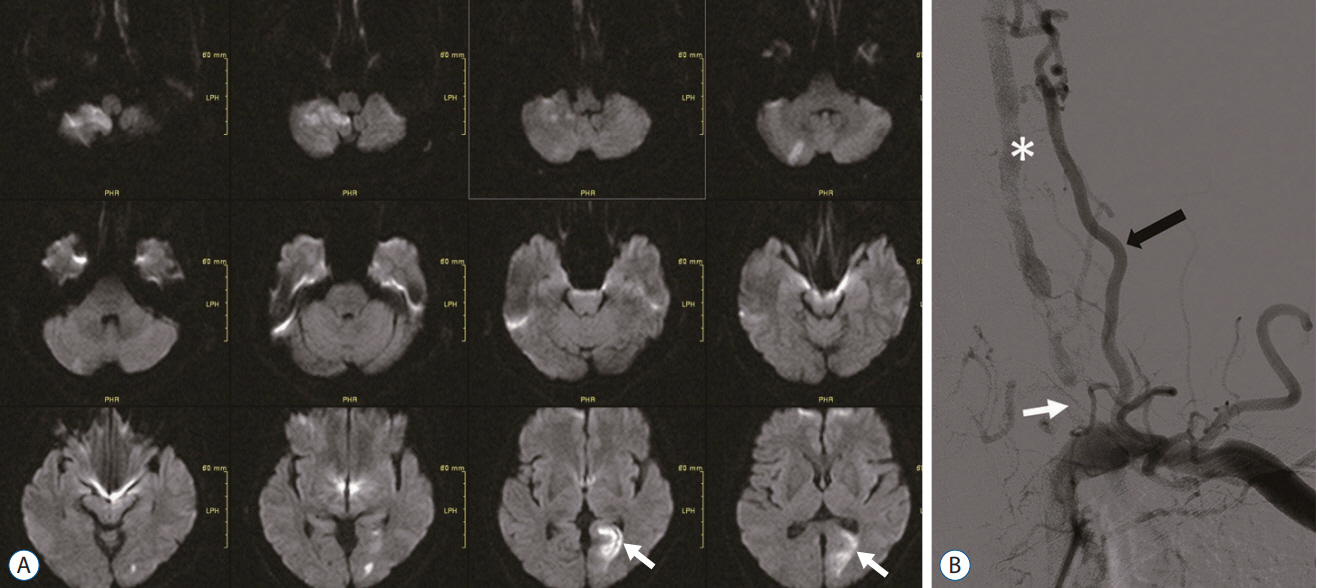
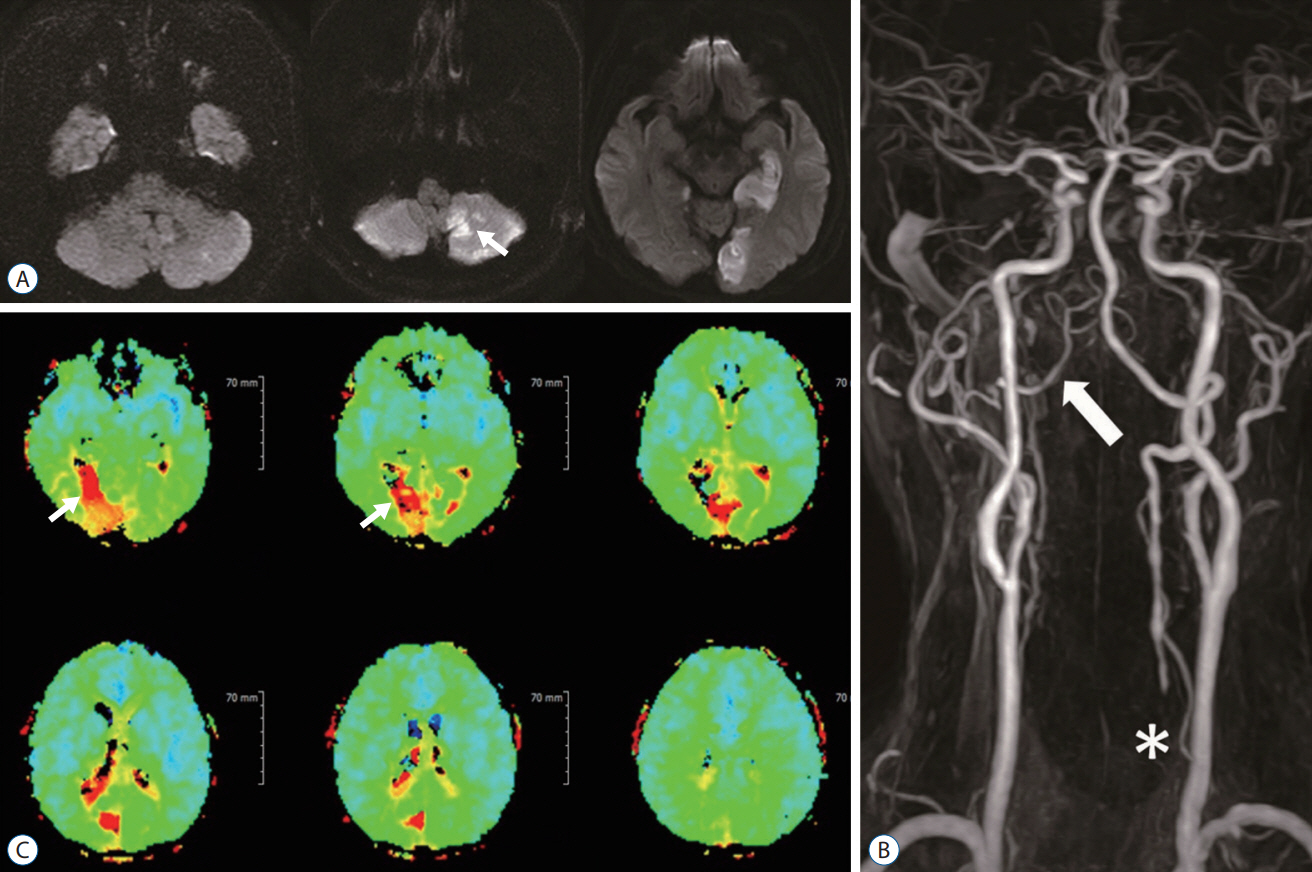
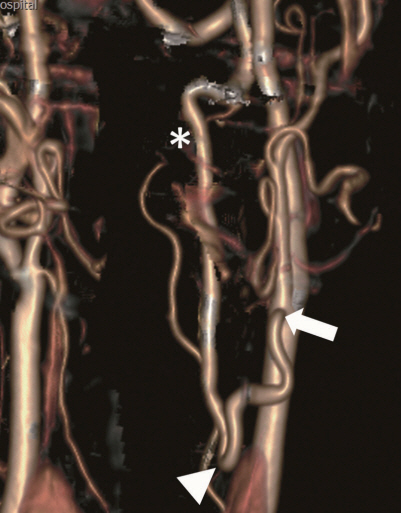
- Vertebral artery (VA) occlusion is frequently encountered, usually without acute ischemic injury of the brain. However, when it is accompanied by hypoplasia or stenosis of the opposite VA, brain ischemia may develop due to insufficient collateral supply. Both hemodynamic instability and embolic infarction can occur in VA occlusion, which may cause severe symptoms in a patient. Extracranial carotid-VA bypass should be considered for symptomatic VA occlusion patients, especially when the patient has repeated ischemic brain injuries. In this report, the cases of three extracranial carotid-VA bypass patients are introduced, along with a brief description of the surgical techniques. All three cases were treated with different bypass methods according to their disease location.
Figure
Reference
-
References
1. Berguer R. Mechanical compression of the vertebral arteries. In : Berguer R, Bauer RB, editors. Vertebrobasilar arterial occlusive disease: Medical and surgical management. New York: Raven Press;1984. p. 45–71.2. Berguer R. Distal vertebral artery bypass: technique, the "occipital connection," and potential uses. J Vasc Surg. 2:621–626. 1985.
Article3. Berguer R. Suboccipital approach to the distal vertebral artery. J Vasc Surg. 30:344–349. 1999.
Article4. Berguer R. Complex Carotid and Vertebral Revascularizations. In : Pearce WH, Matsumura JS, Yao JST, editors. Vascular Surgery in the Endovascular Era. Evanston: Greenwood Academic;2008. p. 344–352.5. Berguer R, Morasch MD, Kline RA. A review of 100 consecutive reconstructions of the distal vertebral artery for embolic and hemodynamic disease. J Vasc Surg. 27:852–859. 1998.
Article6. Caplan LR, Wityk RJ, Glass TA, Tapia J, Pazdera L, Chang HM, et al. New england medical center posterior circulation registry. Ann Neurol. 56:389–398. 2004.
Article7. Chastain HD 2nd, Campbell MS, Iyer S, Roubin GS, Vitek J, Mathur A, et al. Extracranial vertebral artery stent placement: in-hospital and follow-up results. J Neurosurg. 91:547–552. 1999.
Article8. Kieffer E, Praquin B, Chiche L, Koskas F, Bahnini A. Distal vertebral artery reconstruction: long-term outcome. J Vasc Surg. 36:549–554. 2002.
Article9. Kieffer E, Rancurel G, Richard T. Reconstruction of the distal cervical vertebral artery. In : Berguer R, Bauer RB, editors. Vertebrobasilar arterial occlusive disease: Medical and surgical management. New York: Raven Press;1984. p. 265–289.10. Morasch MD, Phade SV, Naughton P, Garcia-Toca M, Escobar G, Berguer R. Primary extracranial vertebral artery aneurysms. Ann Vasc Surg. 27:418–423. 2013.
Article11. Sundt TM Jr, Piepgras DG, Houser OW, Campbell JK. Interposition saphenous vein grafts for advanced occlusive disease and large aneurysms in the posterior circulation. J Neurosurg. 56:205–215. 1982.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical Treatment of Occlusive Cerebrovascular Disease
- Extracranial-Intracranial Bypass Surgery: Surgical Techniques and Perioperative Management
- Asymptomatic Extracranial Internal Carotid Artery Aneurysm: A Case Report
- Occipital Artery to Distal Extracranial Vertebral Artery Bypass for Bilateral Proximal Vertebral Artery Occlusion: Case Report
- Extracranial Carotid-Vertebral Artery Bypass Technique and Surgical Outcomes