J Korean Diabetes.
2022 Jun;23(2):133-137. 10.4093/jkd.2022.23.2.133.
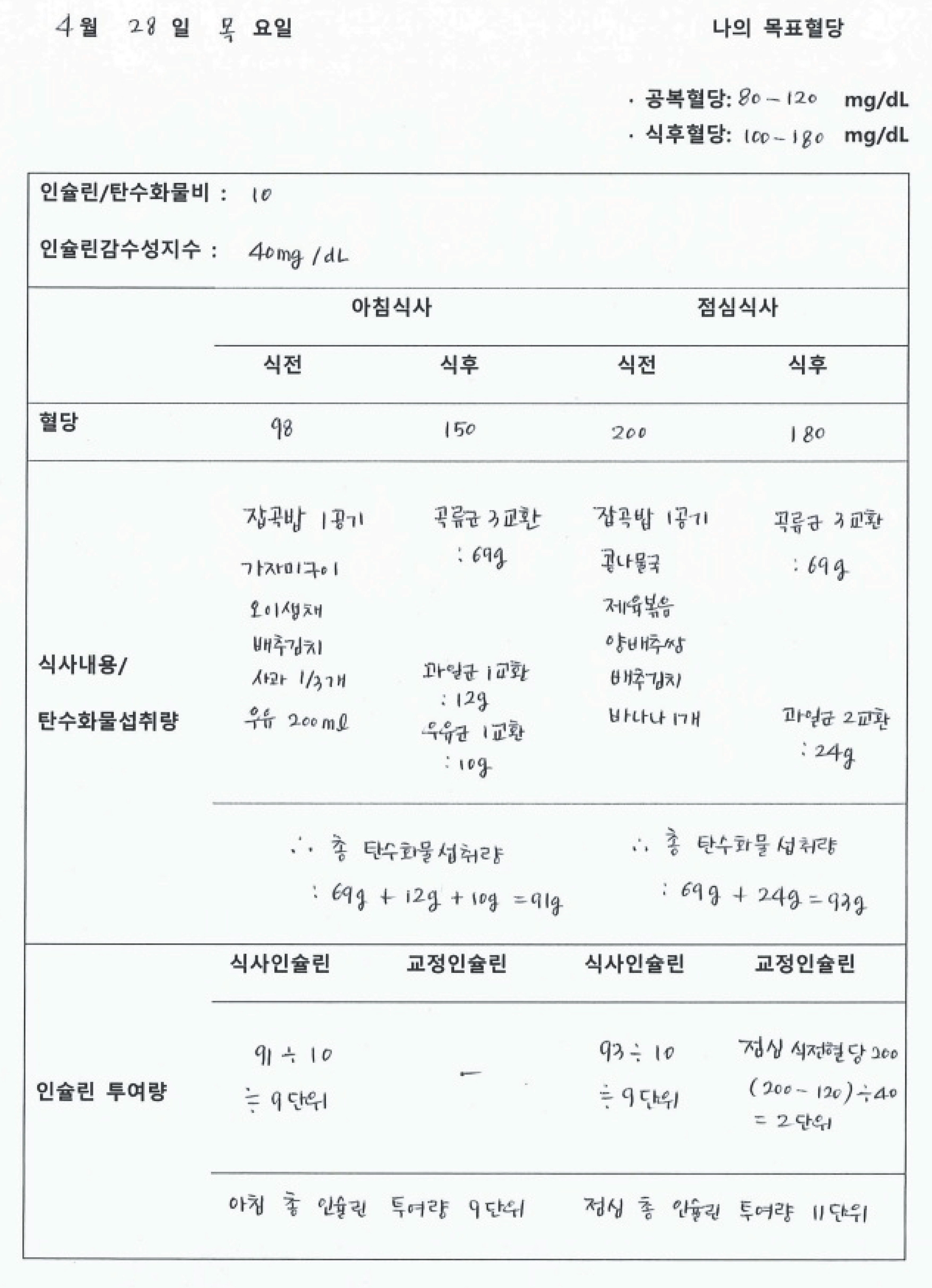
Medical Nutrition Therapy Using Carbohydrate Counting
- Affiliations
-
- 1Department of Nutrition, Seoul National University Bundang Hospital, Seongnam, Korea
- KMID: 2531497
- DOI: http://doi.org/10.4093/jkd.2022.23.2.133
Abstract
- Improved postprandial glucose management requires careful monitoring of carbohydrate counting and consideration of the blood glucose response to dietary carbohydrate. Furthermore, learning how to use insulin-to-carbohydrate ratios for meal planning might help people successfully adjust insulin dose from meal to meal to enhance glycemic control. Regular education to raise knowledge of the link between carbohydrate intake and insulin requirements is critical for those whose meal schedules or carbohydrate consumption are unpredictable. Medical nutrition therapy is an important part of total diabetes management, and each person with diabetes should participate actively in education, self-management, and treatment planning with their health care team, including creation of a personalized food plan.
Figure
Reference
-
1.American Diabetes Association Professional Practice Committee. 5. Facilitating behavior change and well-being to improve health outcomes: Standards of Medical Care in Diabetes-2022. Diabetes Care. 2022. 45(Suppl 1):S60–82.2.Klingensmith GK. Intensive diabetes management. 3rd ed.Alexandria: American Diabetes Association;2003. p. 35–40.3.Warshaw HS., Bolderman KM. Practical carbohydrate counting: a how-to-teach guide for health professionals. Alexandria: American Diabetes Association;2001. p. 26–8.4.Korean Diabetes Association. Core knowledge for diabetes educators. Seoul: Gold Planning and Development;2018. p. 50–60.5.Bell KJ., Barclay AW., Petocz P., Colagiuri S., Brand-Miller JC. Efficacy of carbohydrate counting in type 1 diabetes: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2014. 2:133–40.
Article6.Nakamura T., Hirota Y., Hashimoto N., Matsuda T., Takabe M., Sakaguchi K. Diurnal variation of carbohydrate insulin ratio in adult type 1 diabetic patients treated with continuous subcutaneous insulin infusion. J Diabetes In-vestig. 2014. 5:48–50.
Article7.Hanas R., Adolfsson P. Bolus calculator settings in well-controlled prepubertal children using insulin pumps are characterized by low insulin to carbohydrate ratios and short duration of insulin action time. J Diabetes Sci Tech-nol. 2017. 11:247–52.
Article8.Korean Diabetes Association. Clinical practice guidelines for diabetes. 7th ed.Seoul: Korean Diabetes Association;2021. p. 56–72.9.Kordonouri O., Hartmann R., Remus K., Bläsig S., Sa-deghian E., Danne T. Benefit of supplementary fat plus protein counting as compared with conventional carbohydrate counting for insulin bolus calculation in children with pump therapy. Pediatr Diabetes. 2012. 13:540–4.
Article10.Bao J., de Jong V., Atkinson F., Petocz P., Brand-Miller JC. Food insulin index: physiologic basis for predicting insulin demand evoked by composite meals. Am J Clin Nutr. 2009. 90:986–92.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Nutritional Management and Carbohydrate Counting for Patients with Type 1 Diabetes Mellitus
- The Meal Management of Korean Type 2 Diabetes Patients Using Carbohydrate Counting
- Effect of adherence to carbohydrate counting on metabolic control in children and adolescents with type 1 diabetes mellitus
- Glycemic Index Revisited
- Carbohydrate counting implementation on pediatric type 1 diabetes mellitus: systematic review and meta-analysis