Cancer Res Treat.
2022 Jul;54(3):937-949. 10.4143/crt.2021.871.
Incidence and Survival Rates of Cutaneous Melanoma in South Korea Using Nationwide Health Insurance Claims Data
- Affiliations
-
- 1Department of Orthopaedic Surgery, CHA Bundang Medical Center, CHA University, Seongnam, Korea
- 2Department of Internal Medicine, Yongin Severance Hospital, Yonsei University College of Medicine, Yongin, Korea
- 3Department of Internal Medicine, CHA Bundang Medical Center, CHA University, Seongnam, Korea
- 4CHA Graduate School of Medicine, Seongnam, Korea
- 5inCerebro Drug Discovery Institute, inCerebro Co., Ltd., Seoul, Korea
- KMID: 2531339
- DOI: http://doi.org/10.4143/crt.2021.871
Abstract
- Purpose
Melanoma incidence is rising worldwide along with the associated personal and socioeconomic health expenditures. We investigated the incidence and survival-rate patterns of melanoma in South Korea using nationwide data.
Materials and Methods
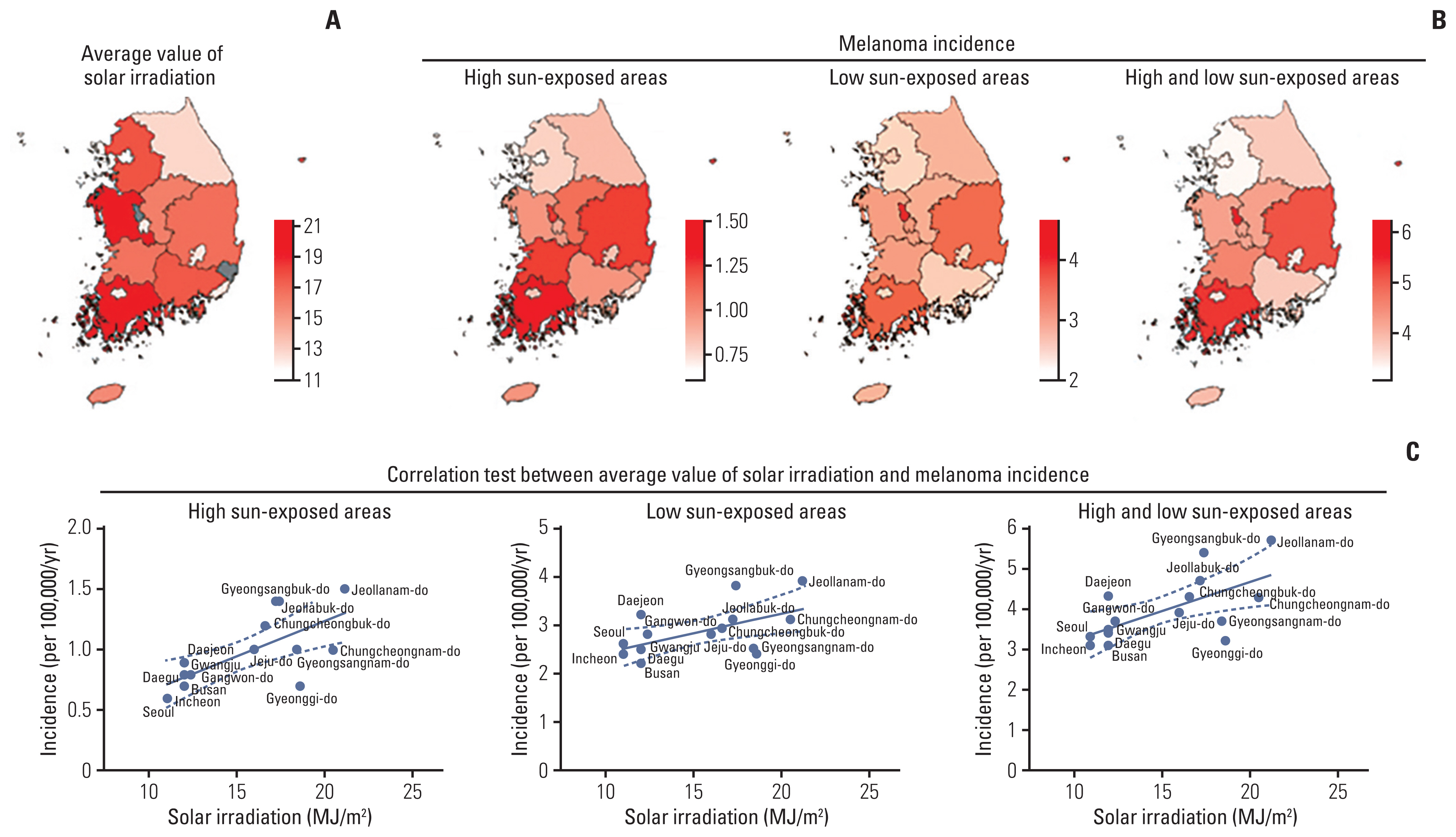
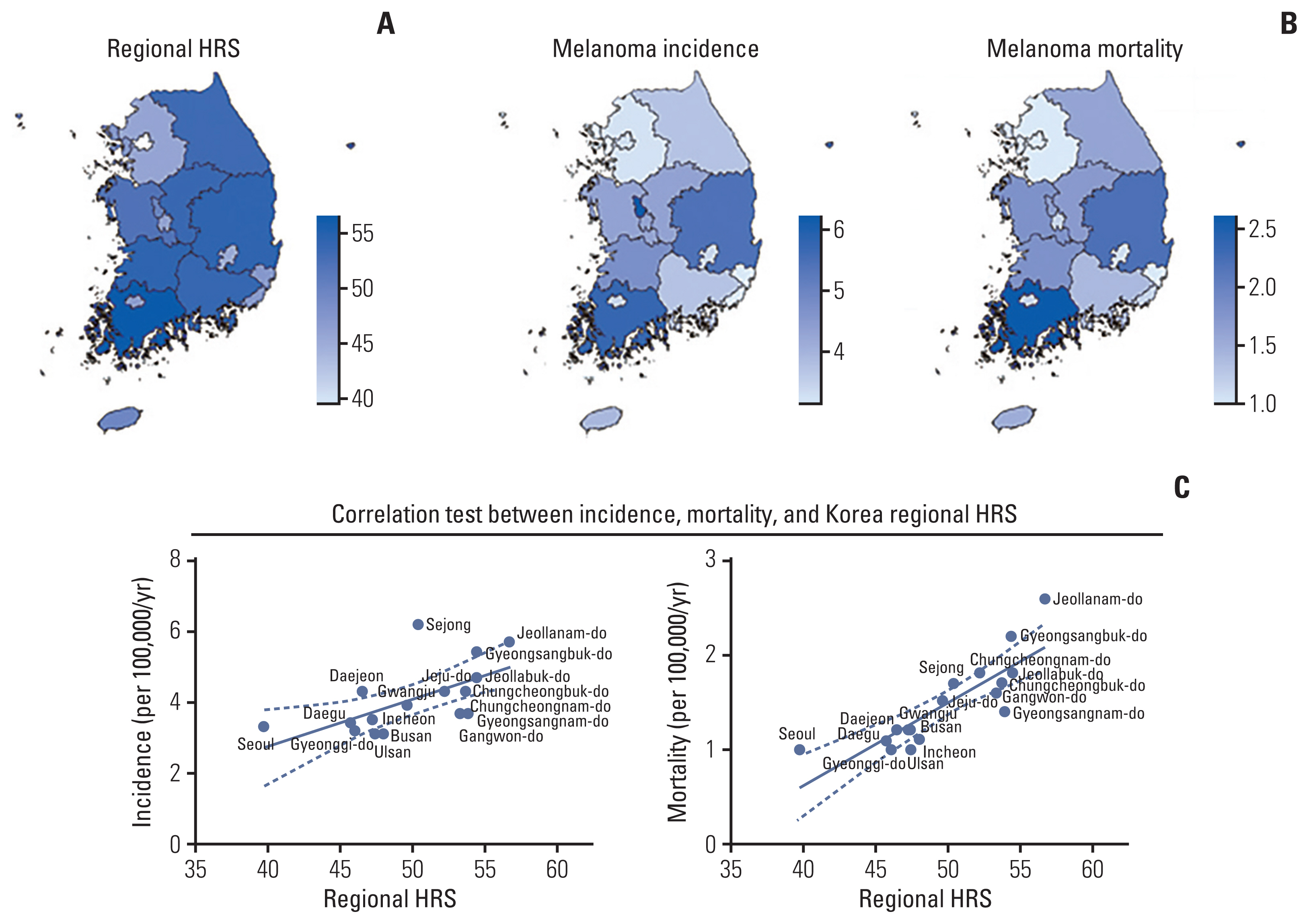
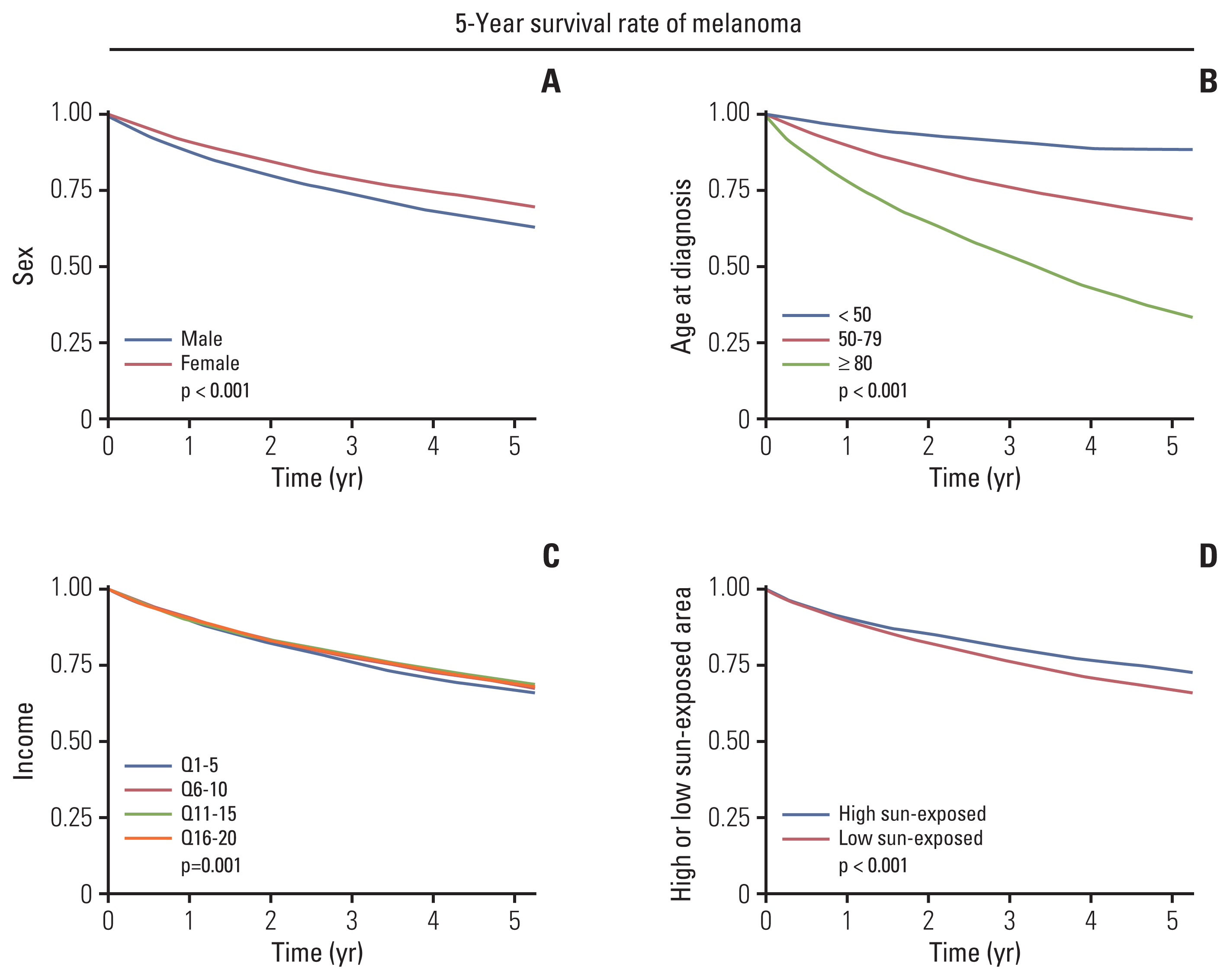
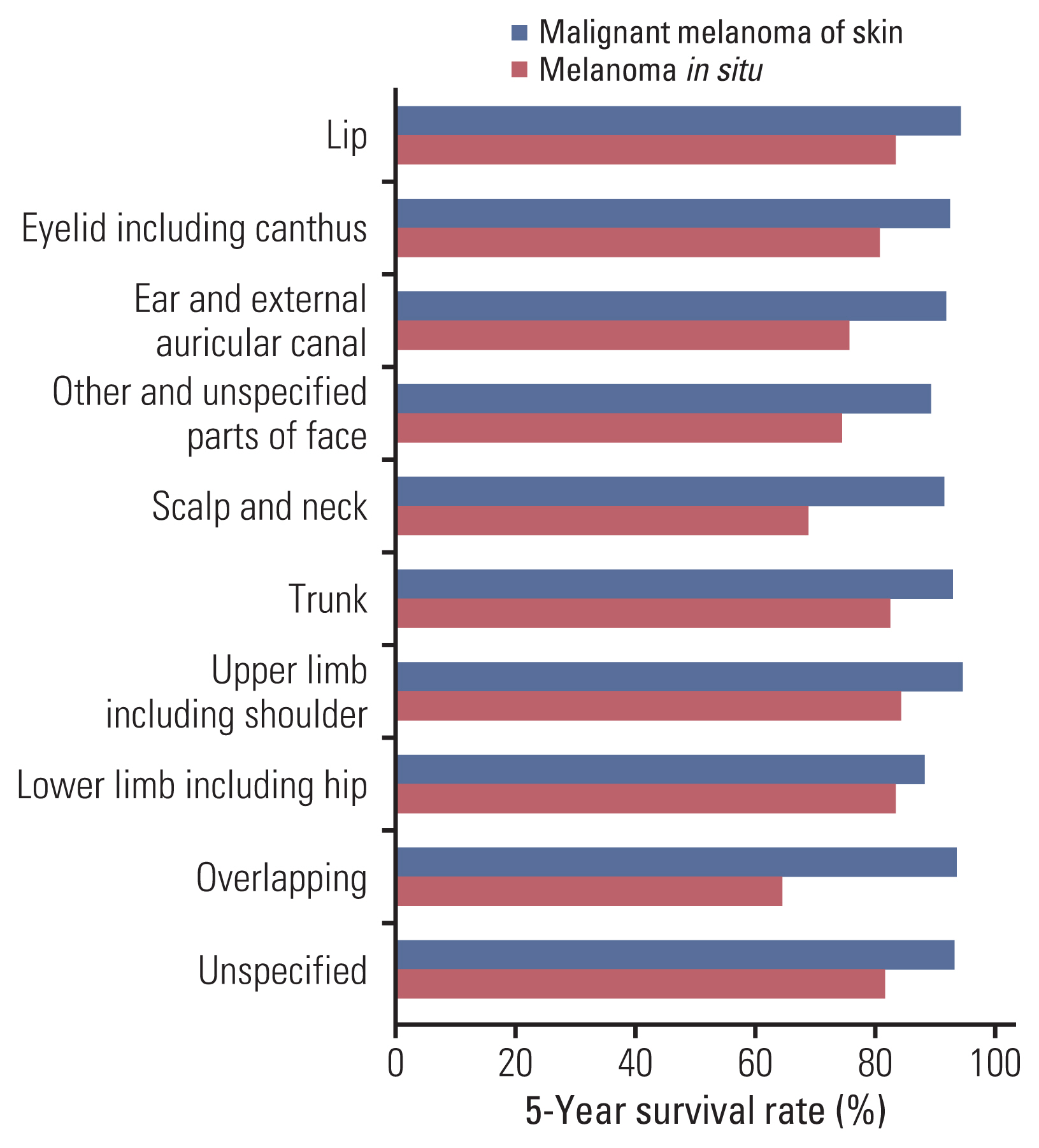
This retrospective cohort study included patients with melanoma between 2004 and 2017, based on National Health Insurance (NHI) claims data in South Korea. The incidence, prevalence, and survival rate were analyzed along with baseline demographic characteristics. We collected solar irradiation dose (SID) and healthcare ranking score (HRS) according to the administrative district from the Korea Meteorological Administration and Korea Health Promotion Institute. The incidence and survival rates were assessed using Pearson's correlation, the Kaplan-Meier estimation, multiple linear regression, and multiple logistic regression methods.
Results
Twenty-five thousand, five hundred ninety-one patients with melanoma were diagnosed during the study period. The age-standardized incidence of melanoma steadily increased from 2004 to 2017 from 2.6 to 3.0/100,000/yr. The incidence of melanoma increased with significantly higher income (p < 0.05). The prevalence followed a similar pattern as the incidence. According to multivariate analysis, HRS significantly influenced the incidence of melanoma in high sun-exposed sites (p < 0.001). There was no significant change in annual mortality. Women had a higher 5-year survival rate than men (78.4% vs. 72.8%). Mortality by the administrative district was highly correlated with HRS.
Conclusion
The incidence of melanoma is increasing in South Korea. A low HRS is associated with both higher incidence and mortality. The findings of this study could be utilized as a guideline for treating melanoma patients.
Keyword
Figure
Reference
-
References
1. Geller AC, Swetter SM, Brooks K, Demierre MF, Yaroch AL. Screening, early detection, and trends for melanoma: current status (2000–2006) and future directions. J Am Acad Dermatol. 2007; 57:555–72.
Article2. Parkin DM, Bray F, Ferlay J, Pisani P. Estimating the world cancer burden: Globocan 2000. Int J Cancer. 2001; 94:153–6.
Article3. Erdei E, Torres SM. A new understanding in the epidemiology of melanoma. Expert Rev Anticancer Ther. 2010; 10:1811–23.
Article4. Prado G, Svoboda RM, Rigel DS. What’s new in melanoma. Dermatol Clin. 2019; 37:159–68.
Article5. Hildenbrand GL, Hildenbrand LC, Bradford K, Cavin SW. Five-year survival rates of melanoma patients treated by diet therapy after the manner of Gerson: a retrospective review. Altern Ther Health Med. 1995; 1:29–37.6. Erdmann F, Lortet-Tieulent J, Schuz J, Zeeb H, Greinert R, Breitbart EW, et al. International trends in the incidence of malignant melanoma 1953–2008: are recent generations at higher or lower risk? Int J Cancer. 2013; 132:385–400.
Article7. Caini S, Gandini S, Sera F, Raimondi S, Fargnoli MC, Boniol M, et al. Meta-analysis of risk factors for cutaneous melanoma according to anatomical site and clinico-pathological variant. Eur J Cancer. 2009; 45:3054–63.
Article8. Pena SD, Di Pietro G, Fuchshuber-Moraes M, Genro JP, Hutz MH, Kehdy Fde S, et al. The genomic ancestry of individuals from different geographical regions of Brazil is more uniform than expected. PLoS One. 2011; 6:e17063.
Article9. Seong SC, Kim YY, Khang YH, Park JH, Kang HJ, Lee H, et al. Data resource profile: the National Health Information Database of the National Health Insurance Service in South Korea. Int J Epidemiol. 2017; 46:799–800.10. Oh CM, Cho H, Won YJ, Kong HJ, Roh YH, Jeong KH, et al. Nationwide trends in the incidence of melanoma and non-melanoma skin cancers from 1999 to 2014 in South Korea. Cancer Res Treat. 2018; 50:729–37.
Article11. Weber A, Leitzmann MF, Sedlmeier AM, Baurecht H, Jochem C, Haferkamp S, et al. Association between physical activity, grip strength and sedentary behaviour with incidence of malignant melanoma: results from the UK Biobank. Br J Cancer. 2021; 125:593–600.
Article12. Segi M. Cancer mortality for selected sites in 24 countries 1950–1957. Sendai: Tohoku University School of Medicine;1960.13. Korean Statistical Information Service. Population trend survey, resident population (mid-year) in five-year age groups - vital statistics: annual 1993–2020 [Internet]. Daejeon: Statistics Korea;2020. [cited 2020 Aug 24]. Available from: https://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1B040M5&conn_path=I2 .14. Korea Meteorological Administration. Domestic climate data: average annual value data (30 years) [Internet]. Seoul: Korea Meteorological Administration;2020. [cited 2020 Aug 16]. Available from: http://web.kma.go.kr/weather/climate/average_30years.jsp?yy_st=1991&x=27&y=15&stn=0&norm=Y&obs=0 .15. Report for healthcare vulnerable region of Korea [Internet]. Seoul: Korea Health Promotion Institution;2016. [cited 2020 Aug 16]. Avaliable from: https://www.khealth.or.kr/kps/publish/view?menuId=MENU00888&page_no=B2017001&pageNum=2&siteId=&srch_text=&srch_cate=&srch_type=&str_clft_cd_list=&str_clft_cd_type_list=&board_idx=9176 .16. Chan YH. Biostatistics 104: correlational analysis. Singapore Med J. 2003; 44:614–9.17. Nikolaou V, Stratigos AJ. Emerging trends in the epidemiology of melanoma. Br J Dermatol. 2014; 170:11–9.
Article18. Tomizuka T, Namikawa K, Higashi T. Characteristics of melanoma in Japan: a nationwide registry analysis 2011–2013. Melanoma Res. 2017; 27:492–7.
Article19. Karimkhani C, Green AC, Nijsten T, Weinstock MA, Dellavalle RP, Naghavi M, et al. The global burden of melanoma: results from the Global Burden of Disease Study 2015. Br J Dermatol. 2017; 177:134–40.
Article20. Shaikh WR, Dusza SW, Weinstock MA, Oliveria SA, Geller AC, Halpern AC. Melanoma thickness and survival trends in the United States 1989 to 2009. J Natl Cancer Inst. 2016; 108:djv294.21. Lew RA, Sober AJ, Cook N, Marvell R, Fitzpatrick TB. Sun exposure habits in patients with cutaneous melanoma: a case control study. J Dermatol Surg Oncol. 1983; 9:981–6.
Article22. Jung HJ, Kweon SS, Lee JB, Lee SC, Yun SJ. A clinicopathologic analysis of 177 acral melanomas in Koreans: relevance of spreading pattern and physical stress. JAMA Dermatol. 2013; 149:1281–8.
Article23. Minagawa A, Omodaka T, Okuyama R. Melanomas and mechanical stress points on the plantar surface of the foot. N Engl J Med. 2016; 374:2404–6.
Article24. Costello CM, Pittelkow MR, Mangold AR. Acral melanoma and mechanical stress on the plantar surface of the foot. N Engl J Med. 2017; 377:395–6.
Article25. Gandini S, Sera F, Cattaruzza MS, Pasquini P, Picconi O, Boyle P, et al. Meta-analysis of risk factors for cutaneous melanoma: II. Sun exposure. Eur J Cancer. 2005; 41:45–60.
Article26. World Health Organization. The global health observatory: Data>GHO>Indicators>UV radiation [Internet]. Geneva: World Health Organization;2020. [cited 2020 Sep 15]. Available from: https://www.who.int/data/gho/data/indicators/indicator-details/GHO/uv-radiation .27. Johnson-Obaseki SE, Labajian V, Corsten MJ, McDonald JT. Incidence of cutaneous malignant melanoma by socioeconomic status in Canada: 1992–2006. J Otolaryngol Head Neck Surg. 2015; 44:53.
Article28. van der Aa MA, de Vries E, Hoekstra HJ, Coebergh JW, Siesling S. Sociodemographic factors and incidence of melanoma in the Netherlands, 1994–2005. Eur J Cancer. 2011; 47:1056–60.
Article29. Warren Andersen S, Blot WJ, Lipworth L, Steinwandel M, Murff HJ, Zheng W. Association of race and socioeconomic status with colorectal cancer screening, colorectal cancer risk, and mortality in Southern US adults. JAMA Netw Open. 2019; 2:e1917995.
Article30. Demidenko E. The p-value you can’t buy. Am Stat. 2016; 70:33–8.31. Geller AC, Miller DR, Lew RA, Clapp RW, Wenneker MB, Koh HK. Cutaneous melanoma mortality among the socioeconomically disadvantaged in Massachusetts. Am J Public Health. 1996; 86:538–43.
Article32. Hopkins ZH, Moreno C, Carlisle R, Secrest AM. Melanoma prognosis in the United States: Identifying barriers for improved care. J Am Acad Dermatol. 2019; 80:1256–62.
Article33. Gillgren P, Brattstrom G, Frisell J, Persson JO, Ringborg U, Hansson J. Effect of primary site on prognosis in patients with cutaneous malignant melanoma: a study using a new model to analyse anatomical locations. Melanoma Res. 2005; 15:125–32.
Article34. Howard MD, Wee E, Wolfe R, McLean CA, Kelly JW, Pan Y. Anatomic location of primary melanoma: Survival differences and sun exposure. J Am Acad Dermatol. 2019; 81:500–9.
Article35. Berwick M, Armstrong BK, Ben-Porat L, Fine J, Kricker A, Eberle C, et al. Sun exposure and mortality from melanoma. J Natl Cancer Inst. 2005; 97:195–9.
Article36. Balzi D, Carli P, Giannotti B, Buiatti E. Skin melanoma in Italy: a population-based study on survival and prognostic factors. Eur J Cancer. 1998; 34:699–704.
Article37. El Sharouni MA, Witkamp AJ, Sigurdsson V, van Diest PJ, Louwman MW, Kukutsch NA. Sex matters: men with melanoma have a worse prognosis than women. J Eur Acad Dermatol Venereol. 2019; 33:2062–7.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Sensitivity of Medical Insurance Claims Data Using Population-based Cancer Registry Data
- Nationwide Trends in the Incidence of Melanoma and Non-melanoma Skin Cancers from 1999 to 2014 in South Korea
- Clinical Study Using Healthcare Claims Database
- Incidence and Prevalence of Overt Hypothyroidism and Causative Diseases in Korea as Determined Using Claims Data Provided by the Health Insurance Review and Assessment Service
- Trends and Clinical Characteristics of Next-Generation Sequencing–Based Genetic Panel Tests: An Analysis of Korean Nationwide Claims Data