Ann Surg Treat Res.
2022 Jul;103(1):1-11. 10.4174/astr.2022.103.1.1.
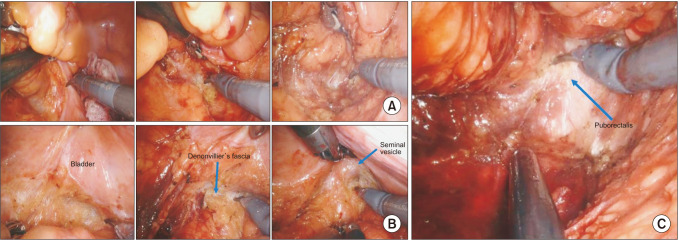
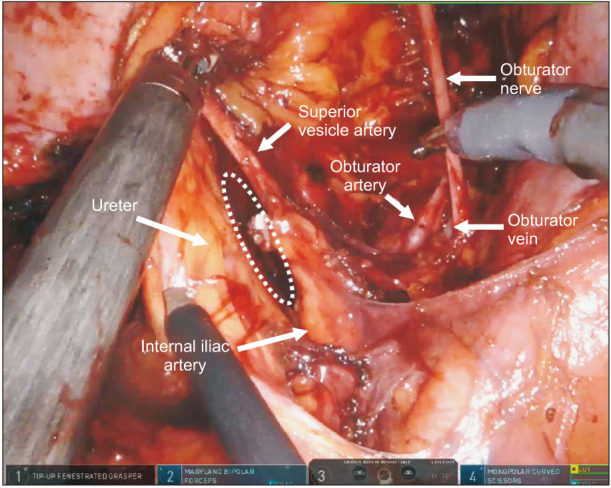
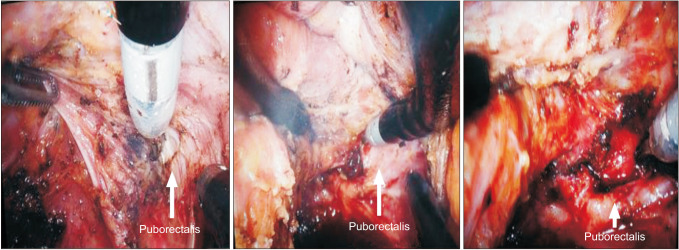
Current status and role of robotic approach in patients with low-lying rectal cancer
- Affiliations
-
- 1Division of Colon and Rectal Surgery, Department of Surgery, Korea University College of Medicine, Seoul, Korea
- KMID: 2531142
- DOI: http://doi.org/10.4174/astr.2022.103.1.1
Abstract
- Utilization of robotic surgical systems has increased over the years. Robotic surgery is presumed to have advantages of enhanced visualization, improved dexterity, and reduced tremor, which is purported to be more suitable for rectal cancer surgery in a confined space than laparoscopic or open surgery. However, evidence supporting improved clinical and oncologic outcomes after robotic surgery remains controversial and limited despite the widespread adoption of robotic surgical systems. To date, numerous observational studies and a few randomized controlled trials have failed to demonstrate that short-term, oncological, and functional outcomes after a robotic surgery are superior to those of laparoscopic surgery for low rectal cancer patients. The objective of this review is to summarize the current state of robotic surgery and its impact on low-lying rectal cancer.
Keyword
Figure
Cited by 2 articles
-
Single-port
versus multiport robotic total mesorectal excision for rectal cancer: initial experiences by case-matched analysis of short-term outcomes
Min Hye Jeong, Hye Jin Kim, Gyu-Seog Choi, Seung Ho Song, Jun Seok Park, Soo Yeun Park, Sung Min Lee, Dong Hee Na
Ann Surg Treat Res. 2023;105(2):99-106. doi: 10.4174/astr.2023.105.2.99.Fluorescence-guided colorectal surgery: applications, clinical results, and protocols
Jin-Min Jung, In Ja Park, Eun Jung Park, Gyung Mo Son,
Ann Surg Treat Res. 2023;105(5):252-263. doi: 10.4174/astr.2023.105.5.252.
Reference
-
1. Heald RJ, Husband EM, Ryall RD. The mesorectum in rectal cancer surgery: the clue to pelvic recurrence? Br J Surg. 1982; 69:613–616. PMID: 6751457.2. Sebag-Montefiore D, Stephens RJ, Steele R, Monson J, Grieve R, Khanna S, et al. Preoperative radiotherapy versus selective postoperative chemoradiotherapy in patients with rectal cancer (MRC CR07 and NCIC-CTG C016): a multicentre, randomised trial. Lancet. 2009; 373:811–820. PMID: 19269519.
Article3. Sauer R, Becker H, Hohenberger W, Rödel C, Wittekind C, Fietkau R, et al. Preoperative versus postoperative chemoradiotherapy for rectal cancer. N Engl J Med. 2004; 351:1731–1740. PMID: 15496622.
Article4. Kapiteijn E, Marijnen CA, Nagtegaal ID, Putter H, Steup WH, Wiggers T, et al. Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer. N Engl J Med. 2001; 345:638–646. PMID: 11547717.
Article5. MacFarlane JK, Ryall RD, Heald RJ. Mesorectal excision for rectal cancer. Lancet. 1993; 341:457–460. PMID: 8094488.
Article6. Nagtegaal ID, Quirke P. What is the role for the circumferential margin in the modern treatment of rectal cancer? J Clin Oncol. 2008; 26:303–312. PMID: 18182672.
Article7. Maslekar S, Sharma A, Macdonald A, Gunn J, Monson JR, Hartley JE. Mesorectal grades predict recurrences after curative resection for rectal cancer. Dis Colon Rectum. 2007; 50:168–175. PMID: 17160574.
Article8. Varela C, Kim NK. Surgical treatment of low-lying rectal cancer: updates. Ann Coloproctol. 2021; 37:395–424. PMID: 34961303.
Article9. Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ, et al. Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol. 2005; 6:477–484. PMID: 15992696.
Article10. Park JW, Kang SB, Hao J, Lim SB, Choi HS, Kim DW, et al. Open versus laparoscopic surgery for mid or low rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): 10-year follow-up of an open-label, non-inferiority, randomised controlled trial. Lancet Gastroenterol Hepatol. 2021; 6:569–577. PMID: 33894918.
Article11. Mercieca-Bebber R, Eggins R, Brown K, Gebski VJ, Brewer K, Lai L, et al. Patient-reported bowel, urinary and sexual outcomes after laparoscopic-assisted resection or open resection for rectal cancer: the Australasian Laparoscopic Cancer of the Rectum Randomized Clinical Trial (ALaCart). Ann Surg. 2022; 02. 15. DOI: 10.1097/SLA.0000000000005412. [Epub].12. Fleshman J, Branda ME, Sargent DJ, Boller AM, George VV, Abbas MA, et al. Disease-free survival and local recurrence for laparoscopic resection compared with open resection of stage II to III rectal cancer: follow-up results of the ACOSOG Z6051 Randomized Controlled Trial. Ann Surg. 2019; 269:589–595. PMID: 30080730.
Article13. Fleshman J, Branda M, Sargent DJ, Boller AM, George V, Abbas M, et al. Effect of laparoscopic-assisted resection vs open resection of stage II or III rectal cancer on pathologic outcomes: the ACOSOG Z6051 Randomized Clinical Trial. JAMA. 2015; 314:1346–1355. PMID: 26441179.
Article14. Jayne DG, Thorpe HC, Copeland J, Quirke P, Brown JM, Guillou PJ. Five-year follow-up of the Medical Research Council CLASICC trial of laparoscopically assisted versus open surgery for colorectal cancer. Br J Surg. 2010; 97:1638–1645. PMID: 20629110.
Article15. Baek SJ, Kim CH, Cho MS, Bae SU, Hur H, Min BS, et al. Robotic surgery for rectal cancer can overcome difficulties associated with pelvic anatomy. Surg Endosc. 2015; 29:1419–1424. PMID: 25159651.
Article16. Park JS, Choi GS, Lim KH, Jang YS, Jun SH. Robotic-assisted versus laparoscopic surgery for low rectal cancer: case-matched analysis of short-term outcomes. Ann Surg Oncol. 2010; 17:3195–3202. PMID: 20589436.
Article17. Baek SJ, Kim SH, Cho JS, Shin JW, Kim J. Robotic versus conventional laparoscopic surgery for rectal cancer: a cost analysis from a single institute in Korea. World J Surg. 2012; 36:2722–2729. PMID: 22855217.
Article18. Park EJ, Cho MS, Baek SJ, Hur H, Min BS, Baik SH, et al. Long-term oncologic outcomes of robot ic low anterior resection for rectal cancer: a comparative study with laparoscopic surgery. Ann Surg. 2015; 261:129–137. PMID: 24662411.
Article19. Patriti A, Ceccarelli G, Bartoli A, Spaziani A, Biancafarina A, Casciola L. Short- and medium-term outcome of robot-assisted and traditional laparoscopic rectal resection. JSLS. 2009; 13:176–183. PMID: 19660212.20. Cho MS, Baek SJ, Hur H, Min BS, Baik SH, Lee KY, et al. Short and long-term outcomes of robotic versus laparoscopic total mesorectal excision for rectal cancer: a case-matched retrospective study. Medicine (Baltimore). 2015; 94:e522. PMID: 25789947.21. Law WL, Foo DC. Comparison of short-term and oncologic outcomes of robotic and laparoscopic resection for mid- and distal rectal cancer. Surg Endosc. 2017; 31:2798–2807. PMID: 27785627.
Article22. Debakey Y, Zaghloul A, Farag A, Mahmoud A, Elattar I. Robotic-assisted versus conventional laparoscopic approach for rectal cancer surgery, First Egyptian Academic Center experience, RCT. Minim Invasive Surg. 2018; 2018:5836562. PMID: 30245874.
Article23. Kim MJ, Park SC, Park JW, Chang HJ, Kim DY, Nam BH, et al. Robot-assisted versus laparoscopic surgery for rectal cancer: a Phase II Open Label Prospective Randomized Controlled Trial. Ann Surg. 2018; 267:243–251. PMID: 28549014.24. Denadai MV, Melani AG, Neto MC, Romagnolo LG, Diniz FD, Véo CA. Robotic rectal surgery: outcomes of the first 102 totally robotic cases handled using the single-docking technique in a reference institution. J Surg Oncol. 2021; 123:997–1004. PMID: 33368284.
Article25. Crippa J, Grass F, Dozois EJ, Mathis KL, Merchea A, Colibaseanu DT, et al. Robotic surgery for rectal cancer provides advantageous outcomes over laparoscopic approach: results from a large retrospective cohort. Ann Surg. 2021; 274:e1218–e1222. PMID: 32068552.26. Prete FP, Pezzolla A, Prete F, Testini M, Marzaioli R, Patriti A, et al. Robotic versus laparoscopic minimally invasive surgery for rectal cancer: a systematic review and meta-analysis of randomized controlled trials. Ann Surg. 2018; 267:1034–1046. PMID: 28984644.
Article27. Jayne D, Pigazzi A, Marshall H, Croft J, Corrigan N, Copeland J, et al. Effect of robotic-assisted vs conventional laparoscopic surgery on risk of conversion to open laparotomy among patients undergoing resection for rectal cancer: the ROLARR Randomized Clinical Trial. JAMA. 2017; 318:1569–1580. PMID: 29067426.
Article28. Oh CK, Huh JW, Lee YJ, Choi MS, Pyo DH, Lee SC, et al. Long-term oncologic outcome of postoperative complications after colorectal cancer surgery. Ann Coloproctol. 2020; 36:273–280. PMID: 32054256.
Article29. Abdalla S, Lupinacci RM, Genova P, Oberlin O, Goasguen N, Fabiani B, et al. Does conversion during minimally invasive rectal surgery for cancer have an impact on short-term and oncologic outcomes? Results of a retrospective cohort study. Surg Endosc. 2022; 36:3558–3566. PMID: 34398282.
Article30. Hopkins MB, Geiger TM, Bethurum AJ, Ford MM, Muldoon RL, Beck DE, et al. Comparing pathologic outcomes for robotic versus laparoscopic Surgery in rectal cancer resection: a propensity adjusted analysis of 7616 patients. Surg Endosc. 2020; 34:2613–2622. PMID: 31346754.
Article31. Lim DR, Bae SU, Hur H, Min BS, Baik SH, Lee KY, et al. Long-term oncological outcomes of robotic versus laparoscopic total mesorectal excision of mid-low rectal cancer following neoadjuvant chemoradiation therapy. Surg Endosc. 2017; 31:1728–1737. PMID: 27631313.
Article32. Tilney HS, Huddy JR, Nizar AS, Smith R, Gudgeon AM. Minimal access rectal cancer surgery: an observational study of patient outcomes from a district general hospital with over a decade of experience with robotic rectal cancer surgery. Colorectal Dis. 2021; 23:1961–1970. PMID: 34157214.
Article33. Kim J, Baek SJ, Kang DW, Roh YE, Lee JW, Kwak HD, et al. Robotic resection is a good prognostic factor in rectal cancer compared with laparoscopic resection: long-term survival analysis using propensity score matching. Dis Colon Rectum. 2017; 60:266–273. PMID: 28177988.
Article34. Yamaoka Y, Shiomi A, Kagawa H, Hino H, Manabe S, Kato S, et al. Robotic surgery for clinical T4 rectal cancer: short- and long-term outcomes. Surg Endosc. 2022; 36:91–99. PMID: 33409593.
Article35. Park SY, Lee SM, Park JS, Kim HJ, Choi GS. Robot surgery shows similar long-term oncologic outcomes as laparoscopic surgery for mid/lower rectal cancer but is beneficial to ypT3/4 after preoperative chemoradiation. Dis Colon Rectum. 2021; 64:812–821. PMID: 33833141.
Article36. Barry MJ, Fowler FJ Jr, O’Leary MP, Bruskewitz RC, Holtgrewe HL, Mebust WK, et al. The Measurement Committee of the American Urological Association. The American Urological Association symptom index for benign prostatic hyperplasia. J Urol. 1992; 148:1549–1557. PMID: 1279218.
Article37. Mak TW, Lee JF, Futaba K, Hon SS, Ngo DK, Ng SS. Robotic surgery for rectal cancer: A systematic review of current practice. World J Gastrointest Oncol. 2014; 6:184–193. PMID: 24936229.
Article38. Panteleimonitis S, Ahmed J, Ramachandra M, Farooq M, Harper M, Parvaiz A. Urogenital function in robotic vs laparoscopic rectal cancer surgery: a comparative study. Int J Colorectal Dis. 2017; 32:241–248. PMID: 27770247.
Article39. Wang G, Wang Z, Jiang Z, Liu J, Zhao J, Li J. Male urinary and sexual function after robotic pelvic autonomic nerve-preserving surgery for rectal cancer. Int J Med Robot. 2017; 13:e1725.
Article40. D’Annibale A, Pernazza G, Monsellato I, Pende V, Lucandri G, Mazzocchi P, et al. Total mesorectal excision: a comparison of oncological and functional outcomes between robotic and laparoscopic surgery for rectal cancer. Surg Endosc. 2013; 27:1887–1895. PMID: 23292566.
Article41. Kim HJ, Choi GS, Park JS, Park SY, Yang CS, Lee HJ. The impact of robotic surgery on quality of life, urinary and sexual function following total mesorectal excision for rectal cancer: a propensity score-matched analysis with laparoscopic surgery. Colorectal Dis. 2018; 20:O103–O113. PMID: 29460997.
Article42. Rosen RC, Cappelleri JC, Gendrano N 3rd. The International Index of Erectile Function (IIEF): a state-of-the-science review. Int J Impot Res. 2002; 14:226–244. PMID: 12152111.
Article43. Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R, et al. The Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther. 2000; 26:191–208. PMID: 10782451.
Article44. Park SY, Choi GS, Park JS, Kim HJ, Ryuk JP, Yun SH. Urinary and erectile function in men after total mesorectal excision by laparoscopic or robot-assisted methods for the treatment of rectal cancer: a case-matched comparison. World J Surg. 2014; 38:1834–1842. PMID: 24366278.
Article45. Galata C, Vassilev G, Haas F, Kienle P, Büttner S, Reißfelder C, et al. Clinical, oncological, and functional outcomes of Da Vinci (Xi)-assisted versus conventional laparoscopic resection for rectal cancer: a prospective, controlled cohort study of 51 consecutive cases. Int J Colorectal Dis. 2019; 34:1907–1914. PMID: 31642968.
Article46. Fleming CA, Cullinane C, Lynch N, Killeen S, Coffey JC, Peirce CB. Urogenital function following robotic and laparoscopic rectal cancer surgery: meta-analysis. Br J Surg. 2021; 108:128–137. PMID: 33711141.
Article47. Kim MC, Oh JH. Lateral pelvic lymph node dissection after neoadjuvant chemoradiotherapy in patients with rectal cancer: a single-center experience and literature review. Ann Coloproctol. 2021; 37:382–394. PMID: 34961302.
Article48. Fujita S, Mizusawa J, Kanemitsu Y, Ito M, Kinugasa Y, Komori K, et al. Mesorectal excision with or without lateral lymph node dissection for clinical stage II/III lower rectal cancer (JCOG0212): a multicenter, randomized controlled, noninferiority trial. Ann Surg. 2017; 266:201–207. PMID: 28288057.
Article49. Kusters M, Slater A, Muirhead R, Hompes R, Guy RJ, Jones OM, et al. What to do with lateral nodal disease in low locally advanced rectal cancer?: a call for further reflection and research. Dis Colon Rectum. 2017; 60:577–585. PMID: 28481851.
Article50. Peacock O, Limvorapitak T, Bednarski BK, Kaur H, Taggart MW, Dasari A, et al. Robotic lateral pelvic lymph node dissection after chemoradiation for rectal cancer: a Western perspective. Colorectal Dis. 2020; 22:2049–2056. PMID: 32892473.
Article51. Kim HJ, Choi GS, Park JS, Park SY, Lee HJ, Woo IT, et al. Selective lateral pelvic lymph node dissection: a comparative study of the robotic versus laparoscopic approach. Surg Endosc. 2018; 32:2466–2473. PMID: 29124406.
Article52. Malakorn S, Ouchi A, Sammour T, Bednarski BK, Chang GJ. Robotic lateral pelvic lymph node dissection after neoadjuvant chemoradiation: view from the West. Dis Colon Rectum. 2018; 61:1119–1120. PMID: 30086062.
Article53. Kawada K, Yoshitomi M, Inamoto S, Sakai Y. Indocyanine green fluorescence-guided laparoscopic lateral lymph node dissection for rectal cancer. Dis Colon Rectum. 2019; 62:1401. PMID: 31596765.
Article54. Son GM, Ahn HM, Lee IY, Ha GW. Multifunctional indocyanine green applications for fluorescence-guided laparoscopic colorectal surgery. Ann Coloproctol. 2021; 37:133–140. PMID: 34102813.
Article55. Park IJ, Kim JC. Intersphincteric resection for patients with low-lying rectal cancer: oncological and functional outcomes. Ann Coloproctol. 2018; 34:167–174. PMID: 30208679.
Article56. Eldamshety O, Kotb S, Khater A, Roshdy S, Elashry M, Zahi MS, et al. Early and late functional outcomes of anal sphincter-sparing procedures with total mesorectal excision for anorectal adenocarcinoma. Ann Coloproctol. 2020; 36:148–154. PMID: 32311866.
Article57. Piozzi GN, Kim SH. Robotic intersphincteric resection for low rectal cancer: technical controversies and a systematic review on the perioperative, oncological, and functional outcomes. Ann Coloproctol. 2021; 37:351–367. PMID: 34784706.
Article58. Kim JC, Lee JL, Bong JW, Seo JH, Kim CW, Park SH, et al. Oncological and anorectal functional outcomes of robot-assisted intersphincteric resection in lower rectal cancer, particularly the extent of sphincter resection and sphincter saving. Surg Endosc. 2020; 34:2082–2094. PMID: 31332563.
Article59. Yang SY, Kim NK. Robotic partial excision of levator-ani muscle for locally advanced low rectal cancer invading ipsilateral pelvic floor. Ann Coloproctol. 2020; 36:415–416. PMID: 33486910.
Article60. Yamaguchi T, Kinugasa Y, Shiomi A, Sato S, Yamakawa Y, Kagawa H, et al. Learning curve for robotic-assisted surgery for rectal cancer: use of the cumulative sum method. Surg Endosc. 2015; 29:1679–1685. PMID: 25277477.
Article61. Melich G, Hong YK, Kim J, Hur H, Baik SH, Kim NK, et al. Simultaneous development of laparoscopy and robotics provides acceptable perioperative outcomes and shows robotics to have a faster learning curve and to be overall faster in rectal cancer surgery: analysis of novice MIS surgeon learning curves. Surg Endosc. 2015; 29:558–568. PMID: 25030474.
Article62. Foo CC, Law WL. The learning curve of robotic-assisted low rectal resection of a novice rectal surgeon. World J Surg. 2016; 40:456–462. PMID: 26423674.
Article63. Park EJ, Kim CW, Cho MS, Kim DW, Min BS, Baik SH, et al. Is the learning curve of robotic low anterior resection shorter than laparoscopic low anterior resection for rectal cancer?: a comparative analysis of clinicopathologic outcomes between robotic and laparoscopic surgeries. Medicine (Baltimore). 2014; 93:e109. PMID: 25437022.64. Parascandola SA, Horsey ML, Hota S, Paull JO, Graham A, Pudalov N, et al. The robotic colorectal experience: an outcomes and learning curve analysis of 502 patients. Colorectal Dis. 2021; 23:226–236. PMID: 33048409.
Article65. Bege T, Lelong B, Esterni B, Turrini O, Guiramand J, Francon D, et al. The learning curve for the laparoscopic approach to conservative mesorectal excision for rectal cancer: lessons drawn from a single institution’s experience. Ann Surg. 2010; 251:249–253. PMID: 20040854.
Article66. Kayano H, Okuda J, Tanaka K, Kondo K, Tanigawa N. Evaluation of the learning curve in laparoscopic low anterior resection for rectal cancer. Surg Endosc. 2011; 25:2972–2979. PMID: 21512883.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Role of Robotic Surgery for Rectal Cancer: Overcoming Technical Challenges in Laparoscopic Surgery by Advanced Techniques
- Intersphincteric Resection for Patients With Low-Lying Rectal Cancer: Oncological and Functional Outcomes
- Robotic Intersphincteric Resection for Low Rectal Cancer: Technical Controversies and a Systematic Review on the Perioperative, Oncological, and Functional Outcomes
- Neorectal Mucosal Prolapse After Intersphincteric Resection for Low-Lying Rectal Cancer: A Case Report
- Current status of robotic surgery for pancreatic tumors