J Korean Assoc Oral Maxillofac Surg.
2022 Jun;48(3):182-187. 10.5125/jkaoms.2022.48.3.182.
Coronoidectomy for reduction of superolateral dislocation of mandible condyle
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, School of Dentistry, Jeonbuk National University, Jeonju, Korea
- 2Research Institute of Clinical Medicine of Jeonbuk National UniversityBiomedical Research Institute of Jeonbuk National University Hospital, Jeonju, Korea
- KMID: 2531056
- DOI: http://doi.org/10.5125/jkaoms.2022.48.3.182
Abstract
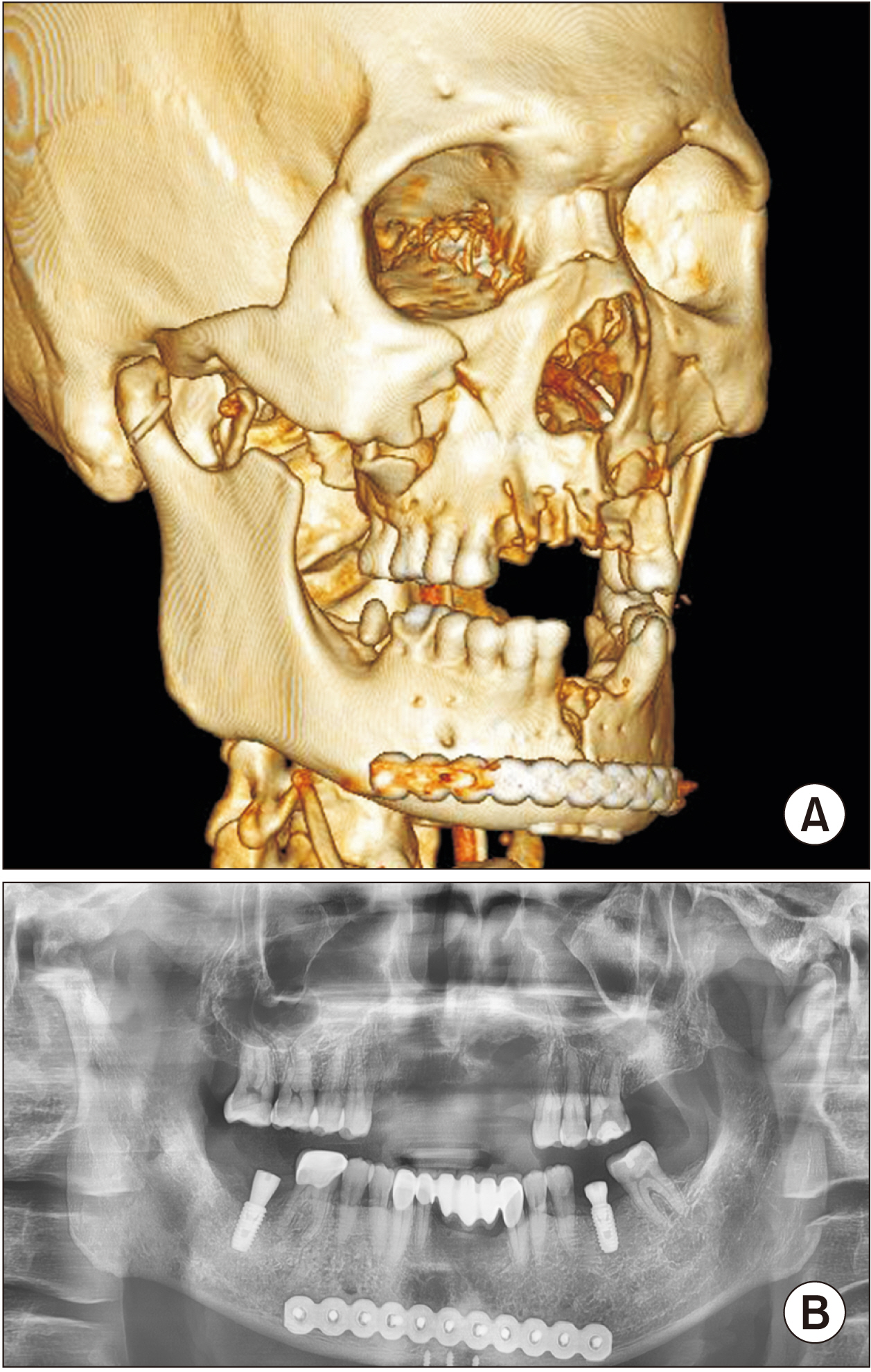
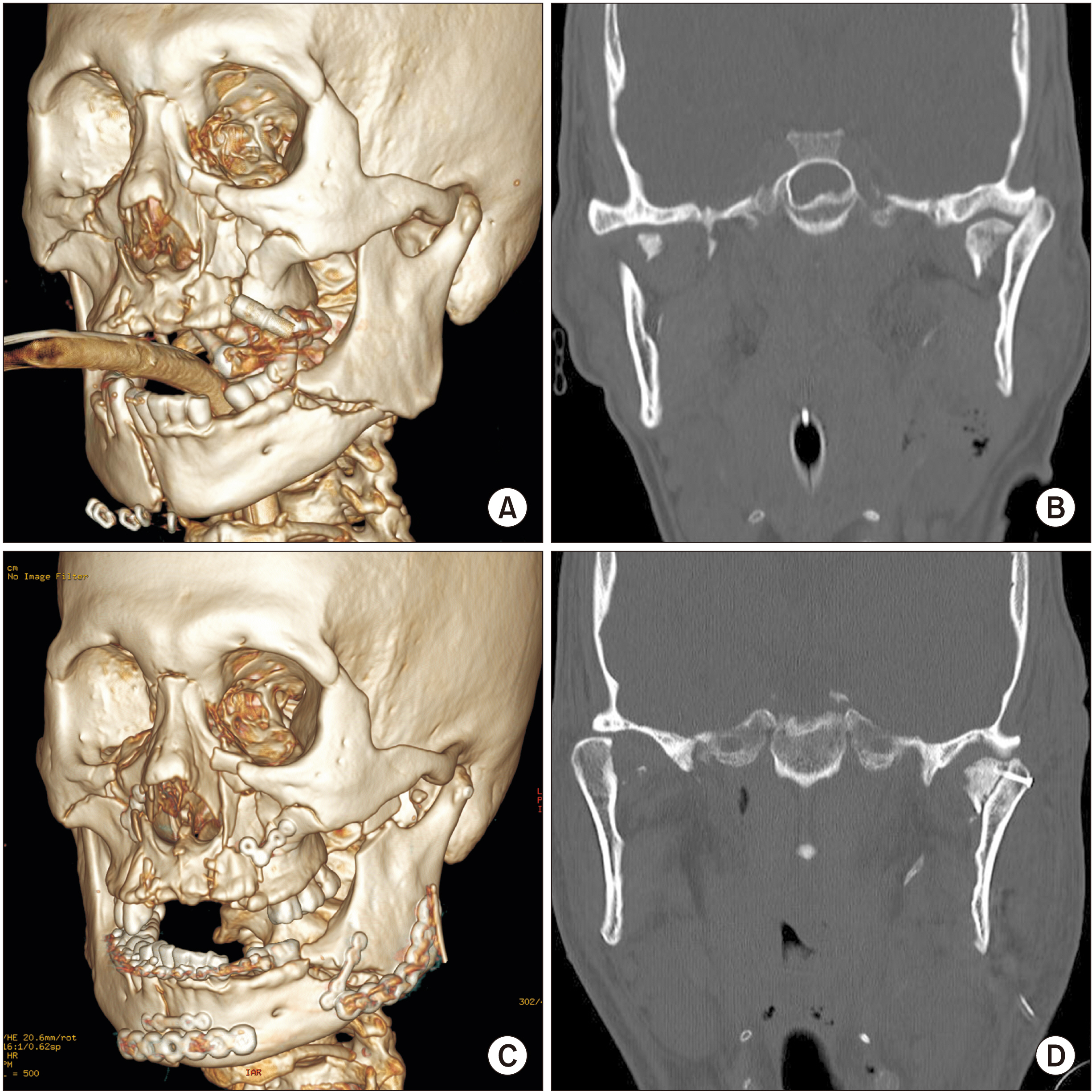
- Superolateral dislocation of the condyle is a rare mandibular fracture. The treatment goal is to return the dislocated condyle to its original position to recover normal function. This study reports on superolateral dislocation of the condyle with mandibular body fracture. The mandibular body was completely separated, and the medial pole of the condyle head was fractured. The condyle segment was unstable and easily dislocated after reduction. The temporalis muscle on the condyle segment might have affected the dislocation of the condyle. A coronoidectomy was performed to disrupt the function of the temporalis muscle on the condyle segment in order to successfully reduce the dislocated condyle. Coronoidectomy is a simple procedure with minimal complications. We successfully performed a coronoidectomy to reduce the superolateral displaced condyle to its original position to achieve normal function. Coronoidectomy can be effectively used for reduction of superolaterally displaced condyles combined with severe maxilla-mandibular fractures.
Keyword
Figure
Reference
-
References
1. Rahman T, Hashmi GS, Ansari MK. 2016; Traumatic superolateral dislocation of the mandibular condyle: case report and review. Br J Oral Maxillofac Surg. 54:457–9. https://doi.org/10.1016/j.bjoms.2015.08.002. DOI: 10.1016/j.bjoms.2015.08.002. PMID: 26305342.
Article2. Patil SG, Patil BS, Joshi U, Rudagi BM, Aftab A. 2017; Superolateral dislocation of bilateral intact mandibular condyles: a rare case series. J Maxillofac Oral Surg. 16:212–8. https://doi.org/10.1007/s12663-016-0928-0. DOI: 10.1007/s12663-016-0928-0. PMID: 28439163. PMCID: PMC5385678.
Article3. Kim BC, Lee YC, Cha HS, Lee SH. 2016; Characteristics of temporomandibular joint structures after mandibular condyle fractures revealed by magnetic resonance imaging. Maxillofac Plast Reconstr Surg. 38:24. https://doi.org/10.1186/s40902-016-0066-0. DOI: 10.1186/s40902-016-0066-0. PMID: 27419123. PMCID: PMC4920844.
Article4. Allen FJ, Young AH. 1969; Lateral displacement of the intact mandibular condyle. A report of five cases. Br J Oral Surg. 7:24–30. https://doi.org/10.1016/s0007-117x(69)80057-0. DOI: 10.1016/S0007-117X(69)80057-0. PMID: 5258902.
Article5. Özalp B, Elbey H, Durgun M, Selçuk CT. 2014; An alternative surgical procedure for anterosuperior dislocation of intact mandibular condyle. J Craniofac Surg. 25:e382–4. https://doi.org/10.1097/SCS.0000000000000965. DOI: 10.1097/SCS.0000000000000965. PMID: 25006956.
Article6. Kothari MC, Hallur N, Sikkerimath B, Gudi S, Kothari CR. 2012; Coronoidectomy, masticatory myotomy and buccal fat pad graft in management of advanced oral submucous fibrosis. Int J Oral Maxillofac Surg. 41:1416–21. https://doi.org/10.1016/j.ijom.2012.03.027. DOI: 10.1016/j.ijom.2012.03.027. PMID: 22551649.
Article7. Wang WH, Xu B, Zhang BJ, Lou HQ. 2016; Temporomandibular joint ankylosis contributing to coronoid process hyperplasia. Int J Oral Maxillofac Surg. 45:1229–33. https://doi.org/10.1016/j.ijom.2016.04.018. DOI: 10.1016/j.ijom.2016.04.018. PMID: 27173825.
Article8. Liu YW, Regmi KP, Ding MC, Li Y, Tian L, Cai BL. 2018; Mandibular coronoidectomy could significantly accelerate the healing process of infratemporal fossa abscess. J Oral Maxillofac Surg. 76:534–44. https://doi.org/10.1016/j.joms.2017.08.014. DOI: 10.1016/j.joms.2017.08.014. PMID: 28888478.
Article9. Kumar P, Singh V, Agrawal A, Bhagol A, Bali R. 2015; Incremental increase in percentage mouth opening after coronoidectomy in temporomandibular joint ankylosis. Int J Oral Maxillofac Surg. 44:859–63. https://doi.org/10.1016/j.ijom.2015.02.008. DOI: 10.1016/j.ijom.2015.02.008. PMID: 25801011.
Article10. Bhutia DP, Mehrotra D, Mahajan N, Howlader D, Gamit J. 2017; Post-traumatic superolateral dislocation of condyle: a case series of 18 condyles with review of literature and a proposed classification. J Oral Biol Craniofac Res. 7:127–33. https://doi.org/10.1016/j.jobcr.2017.04.008. DOI: 10.1016/j.jobcr.2017.04.008. PMID: 28706788. PMCID: PMC5497389.
Article11. Satoh K, Suzuki H, Matsuzaki S. 1994; A type II lateral dislocation of bilateral intact mandibular condyles with a proposed new classification. Plast Reconstr Surg. 93:598–602. DOI: 10.1097/00006534-199493030-00027. PMID: 8115519.
Article12. Bu SS, Jin SL, Yin L. 2007; Superolateral dislocation of the intact mandibular condyle into the temporal fossa: review of the literature and report of a case. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 103:185–9. https://doi.org/10.1016/j.tripleo.2006.01.023. DOI: 10.1016/j.tripleo.2006.01.023. PMID: 17234533.
Article13. Jin KS, Lee H, Sohn JB, Han YS, Jung DU, Sim HY, et al. 2018; Fracture patterns and causes in the craniofacial region: an 8-year review of 2076 patients. Maxillofac Plast Reconstr Surg. 40:29. https://doi.org/10.1186/s40902-018-0168-y. DOI: 10.1186/s40902-018-0168-y. PMID: 30370262. PMCID: PMC6186527.
Article14. Kim BC, Kang Samayoa SR, Kim HJ. 2013; Reduction of superior-lateral intact mandibular condyle dislocation with bone traction hook. J Korean Assoc Oral Maxillofac Surg. 39:238–41. https://doi.org/10.5125/jkaoms.2013.39.5.238. DOI: 10.5125/jkaoms.2013.39.5.238. PMID: 24471051. PMCID: PMC3858138.
Article15. Malik K, Debnath SC, Adhyapok AK, Hazarika K. 2017; An atypical variant of superolateral dislocation of the mandibular condyle: a case report. J Oral Maxillofac Surg. 75:2183.e1–6. https://doi.org/10.1016/j.joms.2017.05.005. DOI: 10.1016/j.joms.2017.05.005. PMID: 28595841.
Article16. Singh V, Gupta P, Khatana S, Bhagol A. 2013; Superolateral dislocation of bilateral intact condyles-an unusual presentation: report of a case and review of literature. Craniomaxillofac Trauma Reconstr. 6:205–10. https://doi.org/10.1055/s-0033-1343780. DOI: 10.1055/s-0033-1343780. PMID: 24436761. PMCID: PMC3773036.
Article17. Shen L, Li P, Li J, Long J, Tian W, Tang W. 2014; Management of superolateral dislocation of the mandibular condyle: a retrospective study of 10 cases. J Craniomaxillofac Surg. 42:53–8. https://doi.org/10.1016/j.jcms.2013.02.002. DOI: 10.1016/j.jcms.2013.02.002. PMID: 23688593.
Article18. Kim SY, Choi YH, Kim YK. 2018; Postoperative malocclusion after maxillofacial fracture management: a retrospective case study. Maxillofac Plast Reconstr Surg. 40:27. https://doi.org/10.1186/s40902-018-0167-z. DOI: 10.1186/s40902-018-0167-z. PMID: 30370261. PMCID: PMC6186531.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Reduction of superior-lateral intact mandibular condyle dislocation with bone traction hook
- Irreducible Posterolateral Dislocation of the Knee Joint with Lateral Dislocation of the Patella: A Report of Two Cases
- Condyle dislocation following mandibular reconstruction using a fibula free flap: complication cases
- Outcome of Surgical Treatment for Mandibular Condyle Fractures
- Current Concepts in the Mandibular Condyle Fracture Management Part II: Open Reduction Versus Closed Reduction