J Korean Assoc Oral Maxillofac Surg.
2022 Jun;48(3):155-158. 10.5125/jkaoms.2022.48.3.155.
Mischievous mandibular third molars camouflaging temporomandibular joint disorders
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, Jaipur Dental College, Jaipur, India
- 2Private Clinic, Palm Desert, CA, USA
- KMID: 2531051
- DOI: http://doi.org/10.5125/jkaoms.2022.48.3.155
Abstract
Objectives
The aim of this study was to observe the relationship between impacted mandibular third molars and development of temporomandibular joint (TMJ) disorders. Knowledge of the factors that have an adverse effect on the TMJ is necessary for proper diagnosis, treatment, and prognosis of TMJ disorders.
Materials and Methods
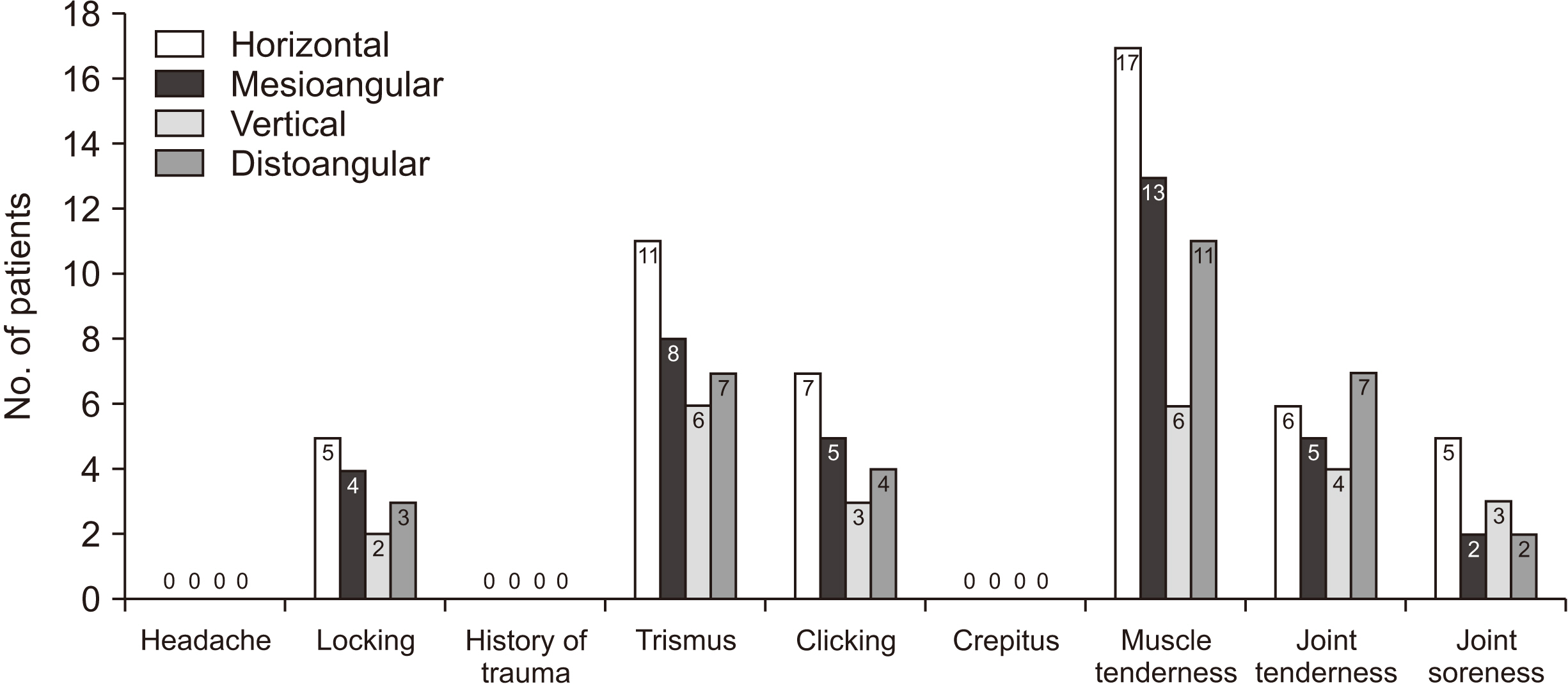
The study was performed on 80 patients aged between 20 and 60 years with impacted mandibular third molars, over a period of two months. The patients were examined clinically and radiologically to determine the type of impaction and detect the associated TMJ symptoms or disorders.
Results
In the 80 patients, 63.8% (51/80) of TMJ disorders were found in the horizontal group, 46.3% (37/80) in the mesioangular group, 42.5% (34/80) in the distoangular group, and 30.0% (24/80) in the vertical group of impacted mandibular third molars.
Conclusion
The study concluded that type of impacted mandibular third molar is factor in the development of temporomandibular disorders.
Keyword
Figure
Reference
-
References
1. Ugolini A, Mapelli A, Segù M, Zago M, Codari M, Sforza C. 2018; Three-dimensional mandibular motion in skeletal Class III patients. Cranio. 36:113–20. https://doi.org/10.1080/08869634.2017.1299830. DOI: 10.1080/08869634.2017.1299830. PMID: 28303737.
Article2. Jasim HH. 2019; Effect of the impacted third molars on the development of temporomandibular joint (TMJ) clicking. J Int Oral Health. 11:393–7. https://doi.org/10.4103/jioh.jioh_310_18. DOI: 10.4103/jioh.jioh_310_18.
Article3. Murphy MK, MacBarb RF, Wong ME, Athanasiou KA. 2013; Temporomandibular disorders: a review of etiology, clinical management, and tissue engineering strategies. Int J Oral Maxillofac Implants. 28:e393–414. https://doi.org/10.11607/jomi.te20. DOI: 10.11607/jomi.te20. PMID: 24278954. PMCID: PMC4349514.
Article4. Clark GT. 1991; Etiologic theory and the prevention of temporomandibular disorders. Adv Dent Res. 5:60–6. https://doi.org/10.1177/08959374910050010901. DOI: 10.1177/08959374910050010901. PMID: 1819285.
Article5. Juhl GI, Jensen TS, Norholt SE, Svensson P. 2009; Incidence of symptoms and signs of TMD following third molar surgery: a controlled, prospective study. J Oral Rehabil. 36:199–209. https://doi.org/10.1111/j.1365-2842.2008.01925.x. DOI: 10.1111/j.1365-2842.2008.01925.x. PMID: 19207447.
Article6. Fischer DJ, Mueller BA, Critchlow CW, LeResche L. 2006; The association of temporomandibular disorder pain with history of head and neck injury in adolescents. J Orofac Pain. 20:191–8. PMID: 16913428.7. Barbosa C, Gavinha S, Soares T, Manso MC. 2016; Coincidence and awareness of the relationship between temporomandibular disorders and jaw injury, orthodontic treatment, and third molar removal in university students. J Oral Facial Pain Headache. 30:221–7. https://doi.org/10.11607/ofph.1587. DOI: 10.11607/ofph.1587. PMID: 27472524.
Article8. Mirmohamadsadeghi H, Alavi O, Karamshahi M, Tabrizi R. 2019; Prevalence of temporomandibular joint problems in candidate patients for impacted third molar surgery with and without the previous temporomandibular disorder: a prospective study. Dent Hypotheses. 10:29–33. https://doi.org/10.4103/denthyp.denthyp_48_19. DOI: 10.4103/denthyp.denthyp_48_19.
Article9. De Rossi SS, Greenberg MS, Liu F, Steinkeler A. 2014; Temporomandibular disorders: evaluation and management. Med Clin North Am. 98:1353–84. https://doi.org/10.1016/j.mcna.2014.08.009. DOI: 10.1016/j.mcna.2014.08.009. PMID: 25443680.
Article10. Lopes V, Mumenya R, Feinmann C, Harris M. 1995; Third molar surgery: an audit of the indications for surgery, post-operative complaints and patient satisfaction. Br J Oral Maxillofac Surg. 33:33–5. https://doi.org/10.1016/0266-4356(95)90083-7. DOI: 10.1016/0266-4356(95)90083-7. PMID: 7718526.
Article11. DeAngelis AF, Chambers IG, Hall GM. 2009; Temporomandibular joint disorders in patients referred for third molar extraction. Aust Dent J. 54:323–5. https://doi.org/10.1111/j.1834-7819.2009.01157.x. DOI: 10.1111/j.1834-7819.2009.01157.x. PMID: 20415930.
Article12. Bertoli FM, Antoniuk SA, Bruck I, Xavier GR, Rodrigues DC, Losso EM. 2007; Evaluation of the signs and symptoms of temporomandibular disorders in children with headaches. Arq Neuropsiquiatr. 65:251–5. https://doi.org/10.1590/s0004-282x2007000200012. DOI: 10.1590/S0004-282X2007000200012. PMID: 17607423.
Article13. Pullinger AG, Seligman DA. 1987; TMJ osteoarthrosis: a differentiation of diagnostic subgroups by symptom history and demographics. J Craniomandib Disord. 1:251–6. PMID: 3481385.14. Huang GJ, Rue TC. 2006; Third-molar extraction as a risk factor for temporomandibular disorder. J Am Dent Assoc. 137:1547–54. https://doi.org/10.14219/jada.archive.2006.0090. DOI: 10.14219/jada.archive.2006.0090. PMID: 17082281.
Article15. Deliverska EG, Petkova M. 2016; Complications after extraction of impacted third molars - literature review. J IMAB. 22:1202–11. https://doi.org/10.5272/jimab.2016223.1202. DOI: 10.5272/jimab.2016223.1202.
Article16. Honda K, Natsumi Y, Urade M. 2008; Correlation between MRI evidence of degenerative condylar surface changes, induction of articular disc displacement and pathological joint sounds in the temporomandibular joint. Gerodontology. 25:251–7. https://doi.org/10.1111/j.1741-2358.2008.00219.x. DOI: 10.1111/j.1741-2358.2008.00219.x. PMID: 18312371.
Article17. Kurita H, Ohtsuka A, Kobayashi H, Kurashina K. 2000; The relationship between the degree of disk displacement and ability to perform disk reduction. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 90:16–20. https://doi.org/10.1067/moe.2000.107222. DOI: 10.1067/moe.2000.107222. PMID: 10884630.
Article18. Akhter R, Hassan NM, Ohkubo R, Tsukazaki T, Aida J, Morita M. 2008; The relationship between jaw injury, third molar removal, and orthodontic treatment and TMD symptoms in university students in Japan. J Orofac Pain. 22:50–6. PMID: 18351034.19. Kim JY, Jee HG, Song HC, Kim SJ, Kim MR. 2017; Clinical and pathologic features related to the impacted third molars in patients of different ages: a retrospective study in the Korean population. J Dent Sci. 12:354–9. https://doi.org/10.1016/j.jds.2017.01.004. DOI: 10.1016/j.jds.2017.01.004. PMID: 30895075. PMCID: PMC6395358.
Article20. Abouelhuda AM, Kim HS, Kim SY, Kim YK. 2017; Association between headache and temporomandibular disorder. J Korean Assoc Oral Maxillofac Surg. 43:363–7. https://doi.org/10.5125/jkaoms.2017.43.6.363. DOI: 10.5125/jkaoms.2017.43.6.363. PMID: 29333365. PMCID: PMC5756792.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A study on simultation of the mandibular movement of the patients with temporomandibular joint disorder
- The Study for Treatment fo Temporo-mandibular Joint Pain
- Treatment of Temporomandibular Joint Disorder by Alloplastic Total Temporomandibular Joint Replacement
- Evaluation of postoperative complications according to treatment of third molars in mandibular angle fracture
- Mandibular condyle position in cone beam computed tomography