Korean J Pain.
2022 Jul;35(3):240-249. 10.3344/kjp.2022.35.3.240.
Not just sensitization: sympathetic mechanisms contribute to expand experimental referred pain
- Affiliations
-
- 1Department of Physiotherapy, Faculty of Health Sciences, Universidad San Jorge, Villanueva de Gállego (Zaragoza), Spain
- 2Department of Health Science and Technology, Faculty of Medicine, Aalborg University, Aalborg, Denmark
- 3Department of Physiatry and Nursing, Faculty of Health Sciences, IIS Aragon, University of Zaragoza, Zaragoza, Spain
- KMID: 2530979
- DOI: http://doi.org/10.3344/kjp.2022.35.3.240
Abstract
- Background
Widespread pain partially depends upon sensitization of central pain mechanisms. However, mechanisms controlling pain distribution are not completely known. The present study sought to assess skin temperature variations in the area of experimentally-induced pain and potential sex differences.
Methods
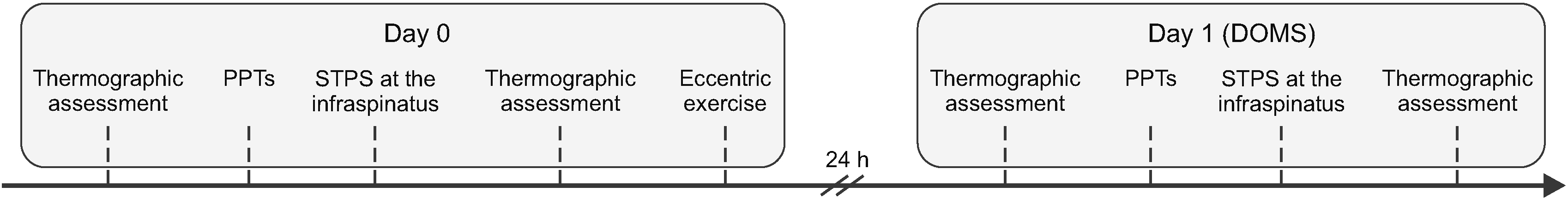
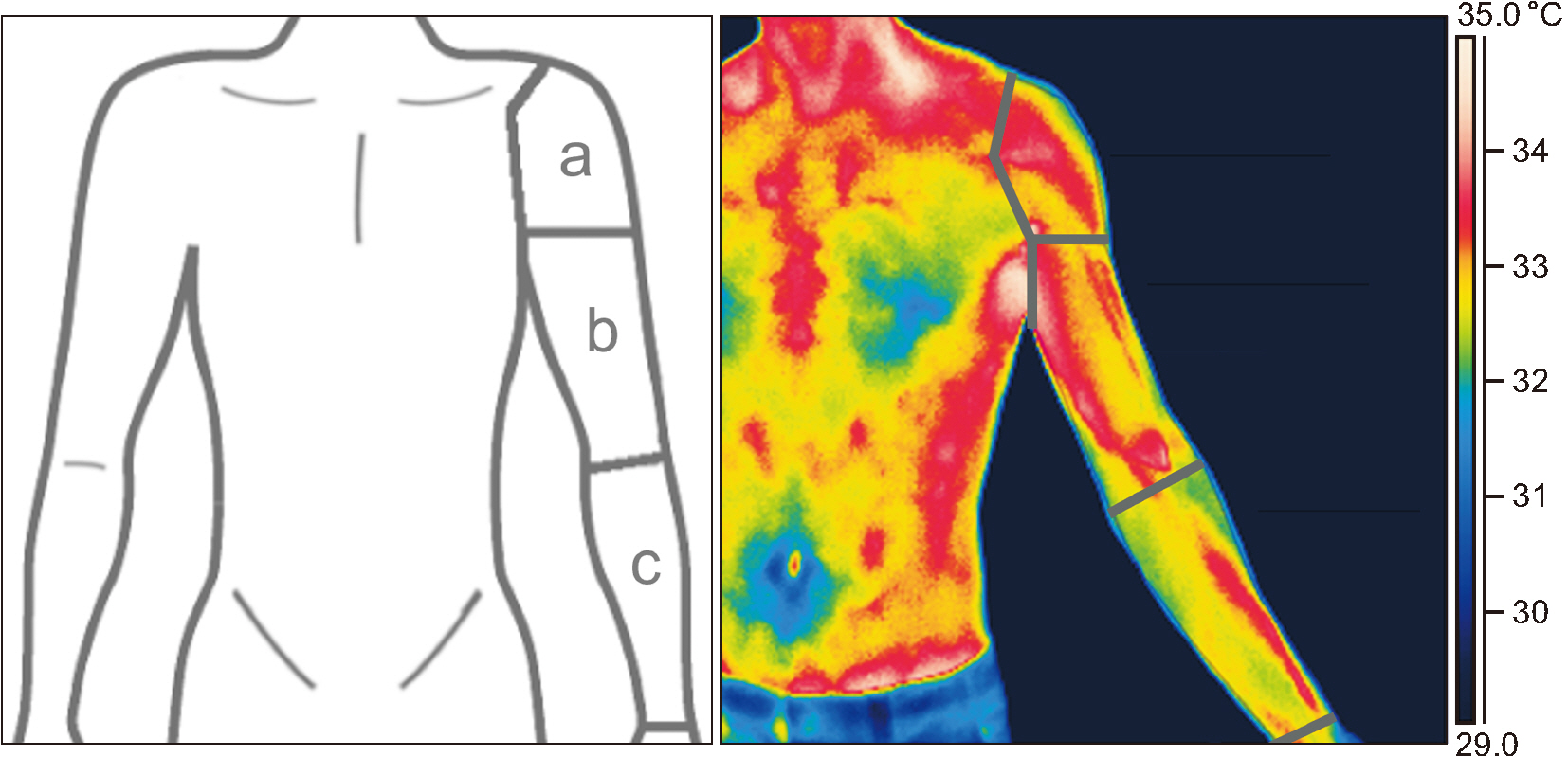
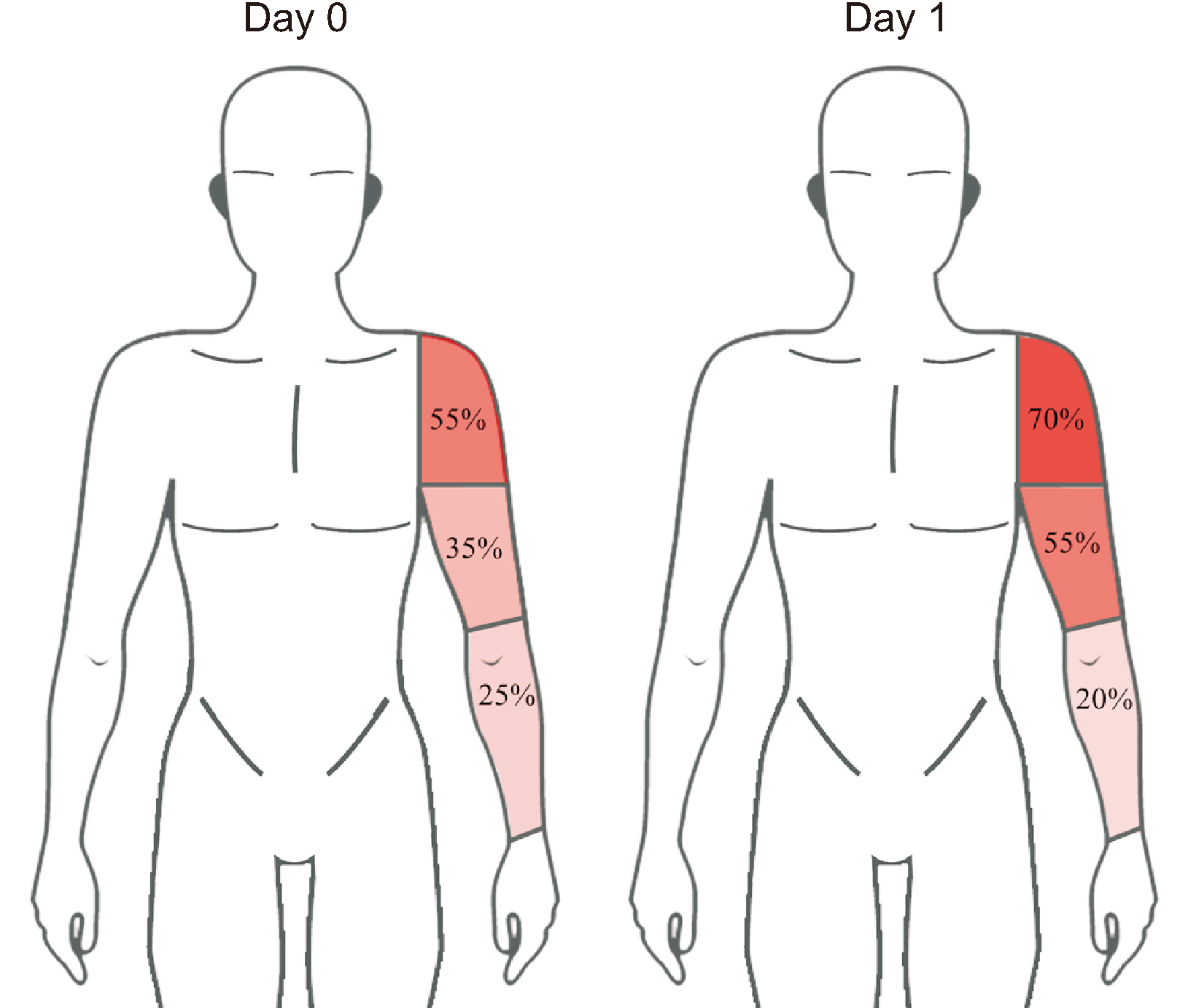
Pressure-pain thresholds (PPTs) were measured on the right infraspinatus muscle. At the end of Day 0, all participants performed an eccentric exercise of the shoulder external rotators to induce muscle soreness 24 hours after. On Day 1, participants indicated on a body chart the area of pain induced by 60 seconds of suprathreshold pressure stimulation (STPS; PPT + 20%) on the right infraspinatus muscle. Skin temperature variations in the area of referred pain were recorded with an infrared thermography camera, immediately before and after the STPS.
Results
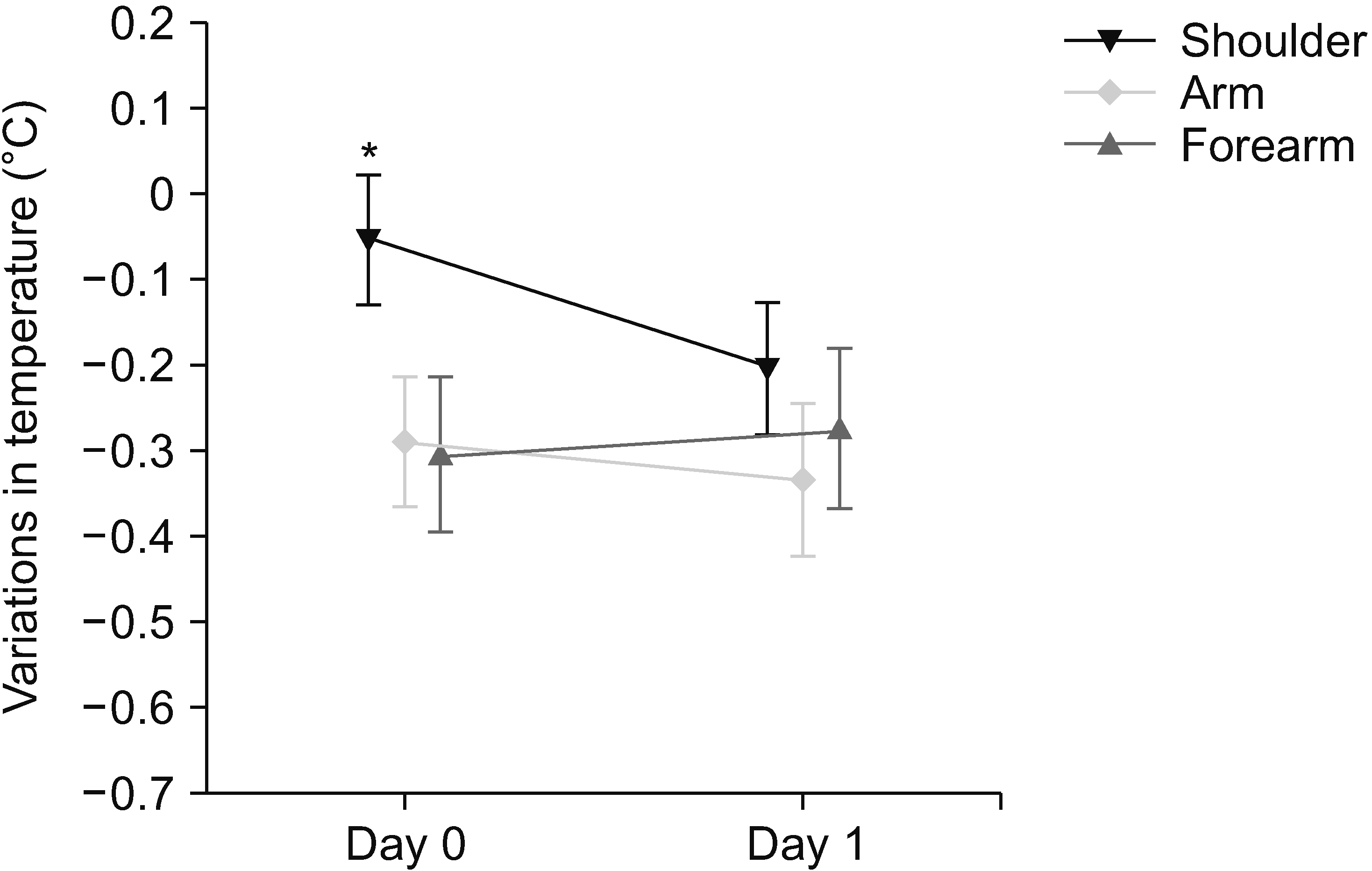
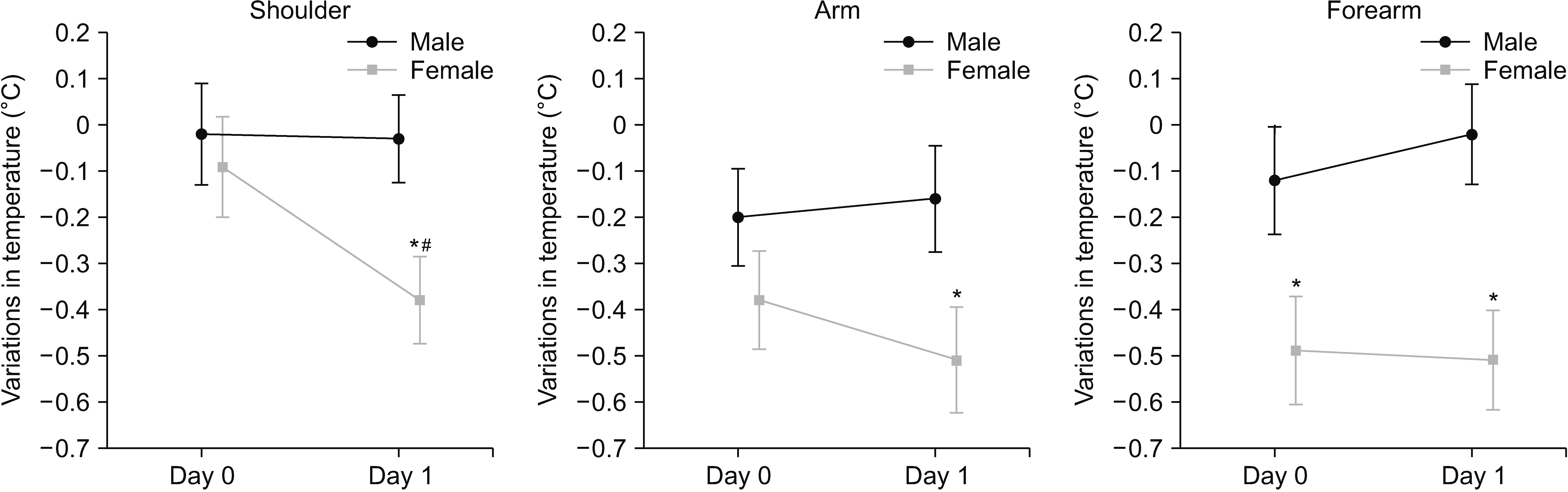
Twenty healthy, pain-free individuals (10 females) participated. On Day 0, the pre-STPS temperature was higher than the post-STPS temperature on the arm (P = 0.001) and forearm (P = 0.003). On Day 1, the pre-STPS temperature was higher than the post-STPS temperature on the shoulder (P = 0.015), arm (P = 0.001), and forearm (P = 0.010). On Day 0, the temperature decrease after STPS in females was greater than in males on the forearm (P = 0.039). On Day 1, a greater temperature decrease was found amongst females compared with males at the shoulder (P = 0.018), arm (P = 0.046), and forearm (P = 0.005).
Conclusions
These findings indicate that sympathetic vasomotor responses contribute to expand pressure-induced referred pain, especially among females.
Keyword
Figure
Cited by 2 articles
-
Data sharing: a direction for securing research transparency
Francis Sahngun Nahm
Korean J Pain. 2022;35(4):359-360. doi: 10.3344/kjp.2022.35.4.359.The impact of central sensitization-related symptoms on subacromial steroid injection outcomes in patients with subacromial impingement syndrome: an observational study
Feyza Nur Yücel, Semiha Özgüç, Yeliz Bahar-Özdemir, Emre Ata
Korean J Pain. 2025;38(1):29-42. doi: 10.3344/kjp.24290.
Reference
-
1. Steingrímsdóttir ÓA, Landmark T, Macfarlane GJ, Nielsen CS. 2017; Defining chronic pain in epidemiological studies: a systematic review and meta-analysis. Pain. 158:2092–107. DOI: 10.1097/j.pain.0000000000001009. PMID: 28767506.
Article2. Gerhardt A, Hartmann M, Blumenstiel K, Tesarz J, Eich W. 2014; The prevalence rate and the role of the spatial extent of pain in nonspecific chronic back pain--a population-based study in the south-west of Germany. Pain Med. 15:1200–10. DOI: 10.1111/pme.12286. PMID: 24341931.
Article3. Vaegter HB, Palsson TS, Graven-Nielsen T. 2017; Facilitated pronociceptive pain mechanisms in radiating back pain compared with localized back pain. J Pain. 18:973–83. DOI: 10.1016/j.jpain.2017.03.002. PMID: 28344100.
Article4. Graven-Nielsen T. 2006; Fundamentals of muscle pain, referred pain, and deep tissue hyperalgesia. Scand J Rheumatol Suppl. 122:1–43. DOI: 10.1080/03009740600865980. PMID: 16997767.5. Doménech-García V, Palsson TS, Herrero P, Graven-Nielsen T. 2016; Pressure-induced referred pain is expanded by persistent soreness. Pain. 157:1164–72. DOI: 10.1097/j.pain.0000000000000497. PMID: 26808146.
Article6. van der Wurff P, Buijs EJ, Groen GJ. 2006; Intensity mapping of pain referral areas in sacroiliac joint pain patients. J Manipulative Physiol Ther. 29:190–5. DOI: 10.1016/j.jmpt.2006.01.007. PMID: 16584942.
Article7. Dimcevski G, Staahl C, Andersen SD, Thorsgaard N, Funch-Jensen P, Arendt-Nielsen L, et al. 2007; Assessment of experimental pain from skin, muscle, and esophagus in patients with chronic pancreatitis. Pancreas. 35:22–9. DOI: 10.1097/mpa.0b013e31805c1762. PMID: 17575541.
Article8. Masuda M, Iida T, Exposto FG, Baad-Hansen L, Kawara M, Komiyama O, et al. 2018; Referred pain and sensations evoked by standardized palpation of the masseter muscle in healthy participants. J Oral Facial Pain Headache. 32:159–66. DOI: 10.11607/ofph.2019. PMID: 29561916.
Article9. Doménech-García V, Skuli Palsson T, Boudreau SA, Herrero P, Graven-Nielsen T. 2018; Pressure-induced referred pain areas are more expansive in individuals with a recovered fracture. Pain. 159:1972–9. DOI: 10.1097/j.pain.0000000000001234. PMID: 29608510.
Article10. Passatore M, Roatta S. 2006; Influence of sympathetic nervous system on sensorimotor function: whiplash associated disorders (WAD) as a model. Eur J Appl Physiol. 98:423–49. DOI: 10.1007/s00421-006-0312-8. PMID: 17036216.
Article11. Martinez-Lavin M. 2007; Biology and therapy of fibromyalgia. Stress, the stress response system, and fibromyalgia. Arthritis Res Ther. 9:216. DOI: 10.1186/ar2146. PMID: 17626613. PMCID: PMC2206360.
Article12. Zhang Y, Ge HY, Yue SW, Kimura Y, Arendt-Nielsen L. 2009; Attenuated skin blood flow response to nociceptive stimulation of latent myofascial trigger points. Arch Phys Med Rehabil. 90:325–32. DOI: 10.1016/j.apmr.2008.06.037. PMID: 19236988.
Article13. Larsson SE, Bodegård L, Henriksson KG, Oberg PA. 1990; Chronic trapezius myalgia. Morphology and blood flow studied in 17 patients. Acta Orthop Scand. 61:394–8. DOI: 10.3109/17453679008993548. PMID: 2239160.14. Morikawa Y, Takamoto K, Nishimaru H, Taguchi T, Urakawa S, Sakai S, et al. 2017; Compression at myofascial trigger point on chronic neck pain provides pain relief through the prefrontal cortex and autonomic nervous system: a pilot study. Front Neurosci. 11:186. DOI: 10.3389/fnins.2017.00186. PMID: 28442987. PMCID: PMC5386976.
Article15. bely JZ Sr, Dickey JP, Montaholi Y. 2017; Experimentally induced central sensitization evokes segmental autonomic responses in humans. Int Phys Med Rehabil J. 1:47–53. https://medcraveonline.com/IPMRJ/experimentally-induced-central-sensitization-evokes-segmental-autonomic-responses-in-humans.html. DOI: 10.15406/ipmrj.2017.01.00013.16. Hinojosa-Laborde C, Chapa I, Lange D, Haywood JR. 1999; Gender differences in sympathetic nervous system regulation. Clin Exp Pharmacol Physiol. 26:122–6. DOI: 10.1046/j.1440-1681.1999.02995.x. PMID: 10065332.
Article17. Hogarth AJ, Mackintosh AF, Mary DA. 2007; Gender-related differences in the sympathetic vasoconstrictor drive of normal subjects. Clin Sci (Lond). 112:353–61. DOI: 10.1042/CS20060288. PMID: 17129210.
Article18. Lei J, You HJ. 2012; Variation of pain and vasomotor responses evoked by intramuscular infusion of hypertonic saline in human subjects: influence of gender and its potential neural mechanisms. Brain Res Bull. 87:564–70. DOI: 10.1016/j.brainresbull.2011.11.003. PMID: 22100333.
Article19. Fillingim RB, King CD, Ribeiro-Dasilva MC, Rahim-Williams B, Riley JL 3rd. 2009; Sex, gender, and pain: a review of recent clinical and experimental findings. J Pain. 10:447–85. DOI: 10.1016/j.jpain.2008.12.001. PMID: 19411059. PMCID: PMC2677686.
Article20. Hildebrandt C, Raschner C, Ammer K. 2010; An overview of recent application of medical infrared thermography in sports medicine in Austria. Sensors (Basel). 10:4700–15. DOI: 10.3390/s100504700. PMID: 22399901. PMCID: PMC3292141.
Article21. Nahm FS. 2013; Infrared thermography in pain medicine. Korean J Pain. 26:219–22. DOI: 10.3344/kjp.2013.26.3.219. PMID: 23861995. PMCID: PMC3710935.
Article22. Ring EF, Ammer K. 2012; Infrared thermal imaging in medicine. Physiol Meas. 33:R33–46. DOI: 10.1088/0967-3334/33/3/R33. PMID: 22370242.
Article23. Dibai-Filho AV, Guirro RRJ. 2015; Evaluation of myofascial trigger points using infrared thermography: a critical review of the literature. J Manipulative Physiol Ther. 38:86–92. DOI: 10.1016/j.jmpt.2014.10.010. PMID: 25467609.
Article24. Simons DG, Travell JG, Simons LS. 2001. Dolor y disfunción miofascial: el manual de los puntos gatillo. 2nd ed. Vol. 1:Médica Panamericana;Madrid: Spanish. https://books.google.es/books?id=30IRTsoFvqcC&printsec=copyright&hl=es#v=onepage&q&f=false. DOI: 10.1016/j.jmpt.2014.10.010.25. RG S. 2015. Guidelines for neuro-musculoskeletal thermography [Internet]. American Academy of Thermology;Greenville (SC): Available at: https://aathermology.org/wp-content/uploads/2018/04/AAT-NMSK-Guidelines-2021.pdf.26. Gibson W, Arendt-Nielsen L, Graven-Nielsen T. 2006; Delayed onset muscle soreness at tendon-bone junction and muscle tissue is associated with facilitated referred pain. Exp Brain Res. 174:351–60. DOI: 10.1007/s00221-006-0466-y. PMID: 16642316.
Article27. Chesterton LS, Sim J, Wright CC, Foster NE. 2007; Interrater reliability of algometry in measuring pressure pain thresholds in healthy humans, using multiple raters. Clin J Pain. 23:760–6. DOI: 10.1097/AJP.0b013e318154b6ae. PMID: 18075402.
Article28. Madeleine P, Mathiassen SE, Arendt-Nielsen L. 2008; Changes in the degree of motor variability associated with experimental and chronic neck-shoulder pain during a standardised repetitive arm movement. Exp Brain Res. 185:689–98. DOI: 10.1007/s00221-007-1199-2. PMID: 18030457.
Article29. Impellizzeri FM, Maffiuletti NA. 2007; Convergent evidence for construct validity of a 7-point likert scale of lower limb muscle soreness. Clin J Sport Med. 17:494–6. DOI: 10.1097/JSM.0b013e31815aed57. PMID: 17993794.
Article30. Choi E, Lee PB, Nahm FS. 2013; Interexaminer reliability of infrared thermography for the diagnosis of complex regional pain syndrome. Skin Res Technol. 19:189–93. DOI: 10.1111/srt.12032. PMID: 23331254.
Article31. Kruse RA Jr, Christiansen JA. 1992; Thermographic imaging of myofascial trigger points: a follow-up study. Arch Phys Med Rehabil. 73:819–23. PMID: 1514891.32. Kimura Y, Ge HY, Zhang Y, Kimura M, Sumikura H, Arendt-Nielsen L. 2009; Evaluation of sympathetic vasoconstrictor response following nociceptive stimulation of latent myofascial trigger points in humans. Acta Physiol (Oxf). 196:411–7. DOI: 10.1111/j.1748-1716.2009.01960.x. PMID: 19210492.
Article33. Skorupska E, Rychlik M, Pawelec W, Samborski W. 2015; Dry needling related short-term vasodilation in chronic sciatica under infrared thermovision. Evid Based Complement Alternat Med. 2015:214374. DOI: 10.1155/2015/214374. PMID: 25821479. PMCID: PMC4363707.
Article34. Skorupska E, Rychlik M, Samborski W. 2015; Intensive vasodilatation in the sciatic pain area after dry needling. BMC Complement Altern Med. 15:72. DOI: 10.1186/s12906-015-0587-6. PMID: 25888420. PMCID: PMC4426539.
Article35. Cagnie B, Barbe T, De Ridder E, Van Oosterwijck J, Cools A, Danneels L. 2012; The influence of dry needling of the trapezius muscle on muscle blood flow and oxygenation. J Manipulative Physiol Ther. 35:685–91. DOI: 10.1016/j.jmpt.2012.10.005. PMID: 23206963.
Article36. Sandberg M, Lundeberg T, Lindberg LG, Gerdle B. 2003; Effects of acupuncture on skin and muscle blood flow in healthy subjects. Eur J Appl Physiol. 90:114–9. DOI: 10.1007/s00421-003-0825-3. PMID: 12827364.
Article37. Sandberg M, Lindberg LG, Gerdle B. 2004; Peripheral effects of needle stimulation (acupuncture) on skin and muscle blood flow in fibromyalgia. Eur J Pain. 8:163–71. DOI: 10.1016/S1090-3801(03)00090-9. PMID: 14987626.
Article38. Sandberg M, Larsson B, Lindberg LG, Gerdle B. 2005; Different patterns of blood flow response in the trapezius muscle following needle stimulation (acupuncture) between healthy subjects and patients with fibromyalgia and work-related trapezius myalgia. Eur J Pain. 9:497–510. DOI: 10.1016/j.ejpain.2004.11.002. PMID: 16139178.
Article39. Lei J, You HJ, Andersen OK, Graven-Nielsen T, Arendt-Nielsen L. 2008; Homotopic and heterotopic variation in skin blood flow and temperature following experimental muscle pain in humans. Brain Res. 1232:85–93. DOI: 10.1016/j.brainres.2008.07.056. PMID: 18680731.
Article40. Nie H, Arendt-Nielsen L, Madeleine P, Graven-Nielsen T. 2006; Enhanced temporal summation of pressure pain in the trapezius muscle after delayed onset muscle soreness. Exp Brain Res. 170:182–90. DOI: 10.1007/s00221-005-0196-6. PMID: 16328284.
Article41. Just TP, DeLorey DS. 2017; Sex differences in sympathetic vasoconstrictor responsiveness and sympatholysis. J Appl Physiol (1985). 123:128–35. DOI: 10.1152/japplphysiol.00139.2017. PMID: 28473610. PMCID: PMC5538817.
Article42. Petrini L, Matthiesen ST, Arendt-Nielsen L. 2015; The effect of age and gender on pressure pain thresholds and suprathreshold stimuli. Perception. 44:587–96. DOI: 10.1068/p7847. PMID: 26422905.
Article43. Riley JL 3rd, Cruz-Almeida Y, Staud R, Fillingim RB. 2020; Age does not affect sex effect of conditioned pain modulation of pressure and thermal pain across 2 conditioning stimuli. Pain Rep. 5:e796. DOI: 10.1097/PR9.0000000000000796. PMID: 32072094. PMCID: PMC7004505.
Article44. Ellermeier W, Westphal W. 1995; Gender differences in pain ratings and pupil reactions to painful pressure stimuli. Pain. 61:435–9. DOI: 10.1016/0304-3959(94)00203-Q. PMID: 7478686.
Article45. Lei J, Jin L, Zhao Y, Sui MY, Huang L, Tan YX, et al. 2011; Sex-related differences in descending norepinephrine and serotonin controls of spinal withdrawal reflex during intramuscular saline induced muscle nociception in rats. Exp Neurol. 228:206–14. DOI: 10.1016/j.expneurol.2011.01.004. PMID: 21238453.
Article46. Mansfield KE, Sim J, Jordan JL, Jordan KP. 2016; A systematic review and meta-analysis of the prevalence of chronic widespread pain in the general population. Pain. 157:55–64. DOI: 10.1097/j.pain.0000000000000314. PMID: 26270591. PMCID: PMC4711387.
Article47. Skorupska E, Rychlik M, Samborski W. 2015; Validation and test-retest reliability of new thermographic technique called Thermovision Technique of Dry Needling for gluteus minimus trigger points in sciatica subjects and TrPs-negative healthy volunteers. Biomed Res Int. 2015:546497. DOI: 10.1155/2015/546497. PMID: 26137486. PMCID: PMC4475557.
Article48. Haddad DS, Brioschi ML, Arita ES. 2012; Thermographic and clinical correlation of myofascial trigger points in the masticatory muscles. Dentomaxillofac Radiol. 41:621–9. DOI: 10.1259/dmfr/98504520. PMID: 23166359. PMCID: PMC3528192.
Article49. Boudreau SA, Badsberg S, Christensen SW, Egsgaard LL. 2016; Digital pain drawings: assessing touch-screen technology and 3D body schemas. Clin J Pain. 32:139–45. DOI: 10.1097/AJP.0000000000000230. PMID: 25756558.50. Slater H, Arendt-Nielsen L, Wright A, Graven-Nielsen T. 2005; Sensory and motor effects of experimental muscle pain in patients with lateral epicondylalgia and controls with delayed onset muscle soreness. Pain. 114:118–30. DOI: 10.1016/j.pain.2004.12.003. PMID: 15733637.
Article