J Korean Foot Ankle Soc.
2022 Jun;26(2):59-65. 10.14193/jkfas.2022.26.2.59.
What is the Significance of the Posterior Malleolus in Ankle Fractures?
- Affiliations
-
- 1Department of Orthopedic Surgery, Hallym University Sacred Heart Hospital, Anyang, Korea
- KMID: 2530484
- DOI: http://doi.org/10.14193/jkfas.2022.26.2.59
Abstract
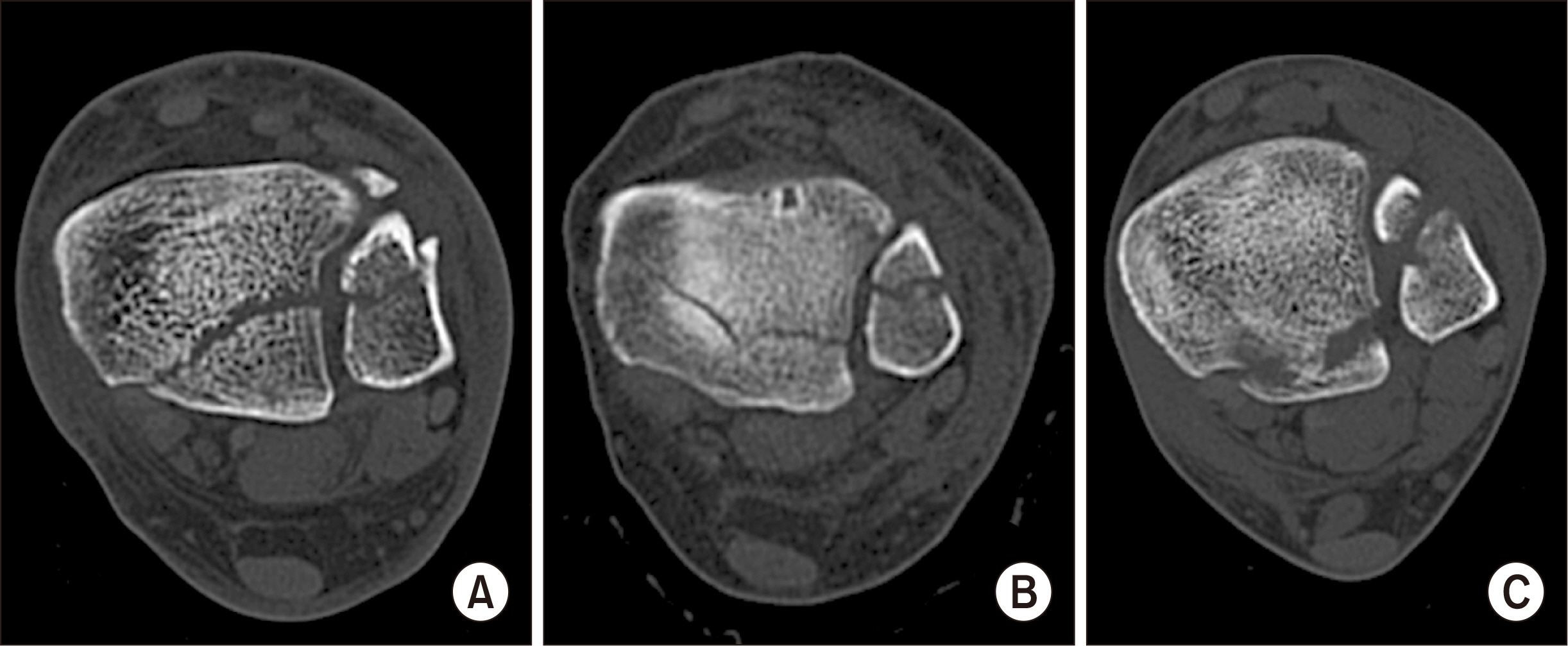
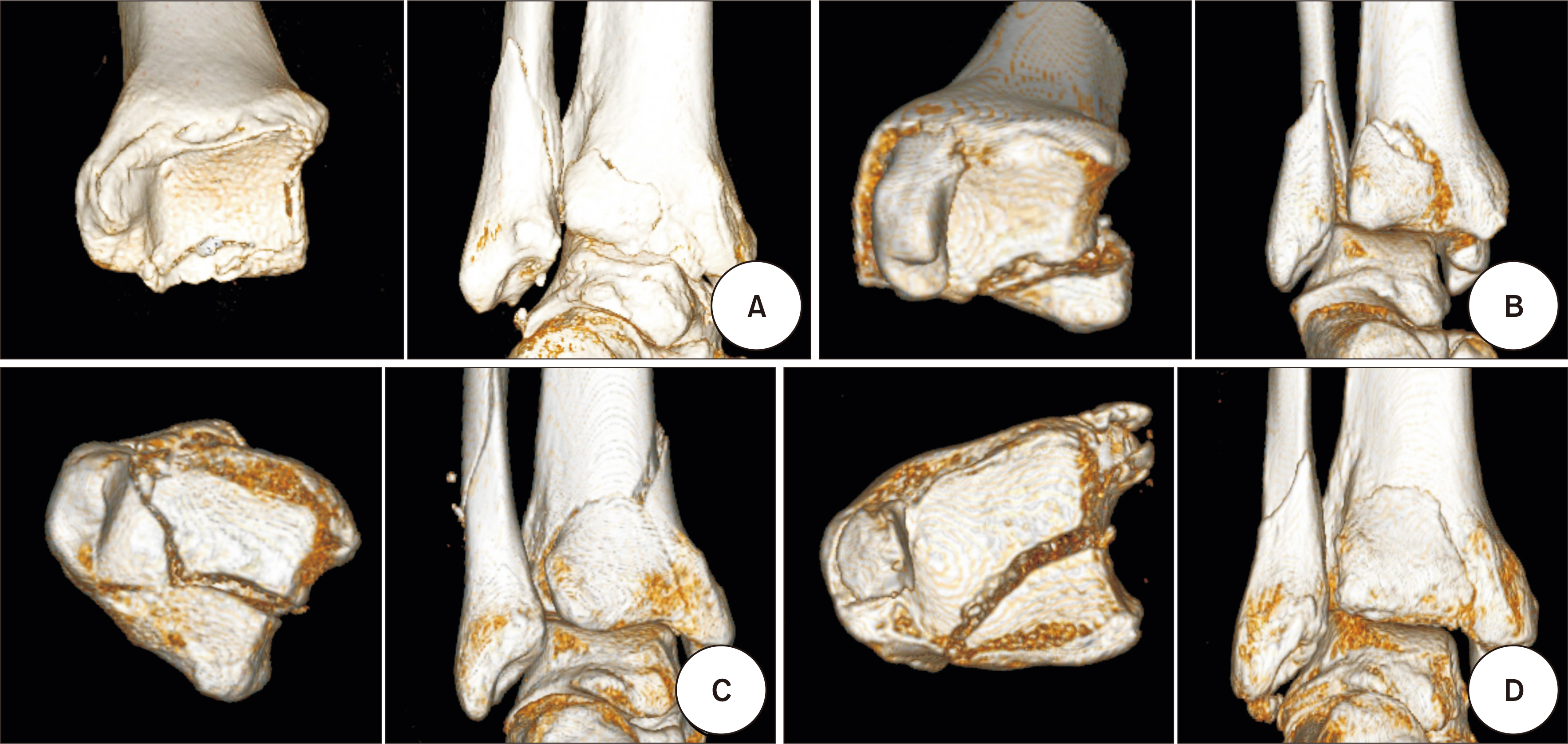
- The posterior malleolar fracture is relatively common fracture of the foot and ankle, but several aspects of this are still controversial. If the posterior malleolus is involved in the ankle fracture, the prognosis is usually poor. A computed tomography scan is essential for accurate diagnosis and treatment planning. Although indirect reduction and the anterior to posterior screw fixation technique have the advantages of a small incision with the requirement of relatively simple skills, direct open reduction and fixation from the posterior side provide a more biomechanically stable and accurate reduction. The precise reduction of the posterior malleolar fragment helps to achieve congruency of the tibia and fibula in the incisura and contributes to syndesmotic stability. It is important to determine the indications for surgical treatment by comprehensively evaluating the three-dimensional structure of the posterior malleolar fracture and all related injuries to the ankle.
Figure
Reference
-
1. Heim D, Niederhauser K, Simbrey N. 2010; The Volkmann dogma: a retrospective, long-term, single-center study. Eur J Trauma Emerg Surg. 36:515–9. doi: 10.1007/s00068-010-0061-6. DOI: 10.1007/s00068-010-0061-6. PMID: 26816305.
Article2. Jaskulka RA, Ittner G, Schedl R. 1989; Fractures of the posterior tibial margin: their role in the prognosis of malleolar fractures. J Trauma. 29:1565–70. doi: 10.1097/00005373-198911000-00018. DOI: 10.1097/00005373-198911000-00018. PMID: 2585569.3. Broos PL, Bisschop AP. 1991; Operative treatment of ankle fractures in adults: correlation between types of fracture and final results. Injury. 22:403–6. doi: 10.1016/0020-1383(91)90106-o. DOI: 10.1016/0020-1383(91)90106-o. PMID: 1806506.
Article4. Lindsjö U. Operative treatment of ankle fracture-dislocations. A follow-up study of 306/321 consecutive cases. Clin Orthop Relat Res. 1985; (199):28–38. doi: 10.1097/00003086-198510000-00005. DOI: 10.1097/00003086-198510000-00005. PMID: 3930122.5. Earle H. 1828; Simple, succeeded by compound dislocation forwards, of the inferior extremity of the tibia, with fracture of its posterior edge, comminuted fracture of the fibula, amputation of the leg, and death. Lancet. 29:346–8.6. Ludloff K. 1926; [Zur Frage der Knöchelbrüche mit Heraussprengung eines hinteren Volkmannschen Dreiecks]. Zentralbl Chir. 53:390–1. German.7. von Volkmann R. [Beiträge zur Chirurgie: anschliessend an einen Bericht über die Thätigkeit der chirurgischen Universitäts-klinik zu Halle im Jahre 1873]. Breitkopf und Härtel;Leipzig: 1875. German.8. Destot E. [Traumatismes du pied et rayons x: malléoles, astragale, calcanéum, avant-pied]. Masson;Paris: 1911. French.9. Henderson M. 1932; Trimalleolar fracture of the ankle. Surg Clin North Am. 12:867–72.10. Nelson M, Jensen N. 1940; The treatment of trimalleolar fractures of the ankle. Surg Gynecol Obstet. 71:509–14.11. Ferries JS, DeCoster TA, Firoozbakhsh KK, Garcia JF, Miller RA. 1994; Plain radiographic interpretation in trimalleolar ankle fractures poorly assesses posterior fragment size. J Orthop Trauma. 8:328–31. doi: 10.1097/00005131-199408000-00009. DOI: 10.1097/00005131-199408000-00009. PMID: 7965295.
Article12. Bartoníček J, Rammelt S, Tuček M, Naňka O. 2015; Posterior malleolar fractures of the ankle. Eur J Trauma Emerg Surg. 41:587–600. doi: 10.1007/s00068-015-0560-6. DOI: 10.1007/s00068-015-0560-6. PMID: 26253884.
Article13. Bartoníček J, Rammelt S, Kostlivý K, Vaněček V, Klika D, Trešl I. 2015; Anatomy and classification of the posterior tibial fragment in ankle fractures. Arch Orthop Trauma Surg. 135:505–16. doi: 10.1007/s00402-015-2171-4. DOI: 10.1007/s00402-015-2171-4. PMID: 25708027.
Article14. Büchler L, Tannast M, Bonel HM, Weber M. 2009; Reliability of radiologic assessment of the fracture anatomy at the posterior tibial plafond in malleolar fractures. J Orthop Trauma. 23:208–12. doi: 10.1097/BOT.0b013e31819b0b23. DOI: 10.1097/BOT.0b013e31819b0b23. PMID: 19516096.
Article15. Rammelt S, Heim D, Hofbauer LC, Grass R, Zwipp H. 2011; [Problems and controversies in the treatment of ankle fractures]. Unfallchirurg. 114:847–60. German. doi: 10.1007/s00113-011-1978-x. DOI: 10.1007/s00113-011-1978-x. PMID: 21779900.16. Xu HL, Li X, Zhang DY, Fu ZG, Wang TB, Zhang PX, et al. 2012; A retrospective study of posterior malleolus fractures. Int Orthop. 36:1929–36. doi: 10.1007/s00264-012-1591-9. DOI: 10.1007/s00264-012-1591-9. PMID: 22777382. PMCID: PMC3427438.
Article17. Müller ME, Nazarian S, Koch P. [Classification AO des fractures]. Vol. 1, Les os longs:Springer-Verlag;Berlin: 1987. French. DOI: 10.1007/978-3-662-06263-0_1.18. Heim UF. 1989; Trimalleolar fractures: late results after fixation of the posterior fragment. Orthopedics. 12:1053–9. doi: 10.3928/0147-7447-19890801-05. DOI: 10.3928/0147-7447-19890801-05. PMID: 2771825.
Article19. Haraguchi N, Haruyama H, Toga H, Kato F. 2006; Pathoanatomy of posterior malleolar fractures of the ankle. J Bone Joint Surg Am. 88:1085–92. doi: 10.2106/JBJS.E.00856. Erratum in: J Bone Joint Surg Am. 2006;88:1835. DOI: 10.2106/JBJS.E.00856. PMID: 16651584.
Article20. Klammer G, Kadakia AR, Joos DA, Seybold JD, Espinosa N. 2013; Posterior pilon fractures: a retrospective case series and proposed classification system. Foot Ankle Int. 34:189–99. doi: 10.1177/1071100712469334. DOI: 10.1177/1071100712469334. PMID: 23413057.21. Switaj PJ, Weatherford B, Fuchs D, Rosenthal B, Pang E, Kadakia AR. 2014; Evaluation of posterior malleolar fractures and the posterior pilon variant in operatively treated ankle fractures. Foot Ankle Int. 35:886–95. doi: 10.1177/1071100714537630. DOI: 10.1177/1071100714537630. PMID: 24942618.
Article22. Mason LW, Marlow WJ, Widnall J, Molloy AP. 2017; Pathoanatomy and associated injuries of posterior malleolus fracture of the ankle. Foot Ankle Int. 38:1229–35. doi: 10.1177/1071100717719533. DOI: 10.1177/1071100717719533. PMID: 28758439.
Article23. Rammelt S, Bartoníček J. 2020; Posterior malleolar fractures: a critical analysis review. JBJS Rev. 8:e19. DOI: 10.2106/JBJS.RVW.19.00207. PMID: 32960029.24. Heim U. 1982; [Indications and technic for the stabilization of the posterior Volkmann's triangle in malleolar fractures]. Unfallheilkunde. 85:388–94. German.25. Müller ME, Allgöwer M, Schneider R, Willenegger H. Manual of internal fixation: techniques recommended by the AO-ASIF group. 3rd ed. Springer;Berlin: 1991. DOI: 10.1007/978-3-662-02695-3.26. Verhage SM, Hoogendoorn JM, Krijnen P, Schipper IB. 2018; When and how to operate the posterior malleolus fragment in trimalleolar fractures: a systematic literature review. Arch Orthop Trauma Surg. 138:1213–22. doi: 10.1007/s00402-018-2949-2. DOI: 10.1007/s00402-018-2949-2. PMID: 29752537.
Article27. Hoogendoorn JM. 2017; Posterior malleolar open reduction and internal fixation through a posterolateral approach for trimalleolar fractures. JBJS Essent Surg Tech. 7:e31. doi: 10.2106/JBJS.ST.17.00016. DOI: 10.2106/JBJS.ST.17.00016. PMID: 30233966. PMCID: PMC6132997.
Article28. Verhage SM, Krijnen P, Schipper IB, Hoogendoorn JM. 2019; Persistent postoperative step-off of the posterior malleolus leads to higher incidence of post-traumatic osteoarthritis in trimalleolar fractures. Arch Orthop Trauma Surg. 139:323–9. doi: 10.1007/s00402-018-3056-0. DOI: 10.1007/s00402-018-3056-0. PMID: 30430238. PMCID: PMC6394475.
Article29. Blom RP, Meijer DT, de Muinck Keizer RO, Stufkens SAS, Sierevelt IN, Schepers T, et al. 2019; Posterior malleolar fracture morphology determines outcome in rotational type ankle fractures. Injury. 50:1392–7. doi: 10.1016/j.injury.2019.06.003. DOI: 10.1016/j.injury.2019.06.003. PMID: 31176480.
Article30. Blom RP, Hayat B, Al-Dirini RMA, Sierevelt I, Kerkhoffs GMMJ, Goslings JC, et al. Posterior malleolar ankle fractures. Bone Joint J. 2020; 102-B:1229–41. doi: 10.1302/0301-620X.102B9.BJJ-2019-1660.R1. DOI: 10.1302/0301-620X.102B9.BJJ-2019-1660.R1. PMID: 32862684.
Article31. Miller AN, Carroll EA, Parker RJ, Helfet DL, Lorich DG. 2010; Posterior malleolar stabilization of syndesmotic injuries is equivalent to screw fixation. Clin Orthop Relat Res. 468:1129–35. doi: 10.1007/s11999-009-1111-4. DOI: 10.1007/s11999-009-1111-4. PMID: 19798540. PMCID: PMC2835618.
Article32. Bartoníček J, Rammelt S, Tuček M. 2017; Posterior malleolar fractures: changing concepts and recent developments. Foot Ankle Clin. 22:125–45. doi: 10.1016/j.fcl.2016.09.009. DOI: 10.1016/j.fcl.2016.09.009. PMID: 28167058.33. Solan MC, Sakellariou A. Posterior malleolus fractures: worth fixing. Bone Joint J. 2017; 99-B:1413–9. doi: 10.1302/0301-620X.99B11.BJJ-2017-1072. DOI: 10.1302/0301-620X.99B11.BJJ-2017-1072. PMID: 29092978.34. Weber M. 2004; Trimalleolar fractures with impaction of the posteromedial tibial plafond: implications for talar stability. Foot Ankle Int. 25:716–27. doi: 10.1177/107110070402501005. DOI: 10.1177/107110070402501005. PMID: 15566703.
Article35. Bois AJ, Dust W. 2008; Posterior fracture dislocation of the ankle: technique and clinical experience using a posteromedial surgical approach. J Orthop Trauma. 22:629–36. doi: 10.1097/BOT.0b013e318184ba4e. DOI: 10.1097/BOT.0b013e318184ba4e. PMID: 18827593.
Article36. Zhong S, Shen L, Zhao JG, Chen J, Xie JF, Shi Q, et al. 2017; Comparison of posteromedial versus posterolateral approach for posterior malleolus fixation in trimalleolar ankle fractures. Orthop Surg. 9:69–76. doi: 10.1111/os.12308. DOI: 10.1111/os.12308. PMID: 28371502. PMCID: PMC6584429.
Article37. Tejwani NC, Pahk B, Egol KA. 2010; Effect of posterior malleolus fracture on outcome after unstable ankle fracture. J Trauma. 69:666–9. doi: 10.1097/TA.0b013e3181e4f81e. DOI: 10.1097/TA.0b013e3181e4f81e. PMID: 20838137.
Article38. Mingo-Robinet J, López-Durán L, Galeote JE, Martinez-Cervell C. 2011; Ankle fractures with posterior malleolar fragment: management and results. J Foot Ankle Surg. 50:141–5. doi: 10.1053/j.jfas.2010.12.013. DOI: 10.1053/j.jfas.2010.12.013. PMID: 21353996.
Article39. Langenhuijsen JF, Heetveld MJ, Ultee JM, Steller EP, Butzelaar RM. 2002; Results of ankle fractures with involvement of the posterior tibial margin. J Trauma. 53:55–60. doi: 10.1097/00005373-200207000-00012. DOI: 10.1097/00005373-200207000-00012. PMID: 12131390.
Article40. Evers J, Barz L, Wähnert D, Grüneweller N, Raschke MJ, Ochman S. 2015; Size matters: the influence of the posterior fragment on patient outcomes in trimalleolar ankle fractures. Injury. 46 Suppl 4:S109–13. doi: 10.1016/S0020-1383(15)30028-0. DOI: 10.1016/S0020-1383(15)30028-0. PMID: 26542855.
Article41. De Vries JS, Wijgman AJ, Sierevelt IN, Schaap GR. 2005; Long-term results of ankle fractures with a posterior malleolar fragment. J Foot Ankle Surg. 44:211–7. doi: 10.1053/j.jfas.2005.02.002. DOI: 10.1053/j.jfas.2005.02.002. PMID: 15940600.
Article42. Levack AE, Warner SJ, Gausden EB, Helfet DL, Lorich DG. 2018; Comparing functional outcomes after injury-specific fixation of posterior malleolar fractures and equivalent ligamentous injuries in rotational ankle fractures. J Orthop Trauma. 32:e123–8. doi: 10.1097/BOT.0000000000001104. DOI: 10.1097/BOT.0000000000001104. PMID: 29401086.
Article43. Odak S, Ahluwalia R, Unnikrishnan P, Hennessy M, Platt S. 2016; Management of posterior malleolar fractures: a systematic review. J Foot Ankle Surg. 55:140–5. doi: 10.1053/j.jfas.2015.04.001. DOI: 10.1053/j.jfas.2015.04.001. PMID: 26100091.
Article44. Berkes MB, Little MT, Lazaro LE, Pardee NC, Schottel PC, Helfet DL, et al. 2013; Articular congruity is associated with short-term clinical outcomes of operatively treated SER IV ankle fractures. J Bone Joint Surg Am. 95:1769–75. doi: 10.2106/JBJS.L.00949. DOI: 10.2106/JBJS.L.00949. PMID: 24088969.
Article45. Kang C, Hwang DS, Lee JK, Won Y, Song JH, Lee GS. 2019; Screw fixation of the posterior malleolus fragment in ankle fracture. Foot Ankle Int. 40:1288–94. doi: 10.1177/1071100719865895. DOI: 10.1177/1071100719865895. PMID: 31387392.
Article46. Drijfhout van Hooff CC, Verhage SM, Hoogendoorn JM. 2015; Influence of fragment size and postoperative joint congruency on long-term outcome of posterior malleolar fractures. Foot Ankle Int. 36:673–8. doi: 10.1177/1071100715570895. DOI: 10.1177/1071100715570895. PMID: 25672944.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Irreducible Ankle Fractures by Locked Posterior Malleolar Fragment: Case Report
- The role of posterior malleolar fragments in ankle pain after trimalleolar fractures
- Treatment of Ankle Fracture and Dislocation
- Comparative Study for the Results of Ankle Fracture Depending onthe Extension of the Posterior Malleolus Fracture
- Treatment of the Posterior Malleolar Fracture