J Korean Med Sci.
2022 Jun;37(22):e177. 10.3346/jkms.2022.37.e177.
The Assessment and Outcomes of Crossmatching in Lung Transplantation in Korean Patients
- Affiliations
-
- 1Department of Thoracic and Cardiovascular Surgery, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- 2Division of Infectious Disease, Department of Internal Medicine, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- 3Division of Pulmonology & Critical Medicine, Department of Internal Medicine, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2530419
- DOI: http://doi.org/10.3346/jkms.2022.37.e177
Abstract
- Background
In lung transplantation, human leukocyte antigen (HLA) compatibility is not included in the lung allocation score system or considered when placing donor allografts. However, HLA matching may affect the outcomes of lung transplantation. This study evaluated the current assessment status, prevalence, and effects of HLA crossmatching in lung transplantation in Korean patients using nationwide multicenter registry data.
Methods
Two hundred and twenty patients who received lung transplantation at six tertiary hospitals in South Korea between March 2015 and December 2019 were retrospectively reviewed. Clinical data, including general demographic characteristics, primary diagnosis, and pretransplant status of the recipients and donors registered by the Korean Organ Transplant Registry, were retrospectively analyzed. Survival analysis was performed using the Kaplan-Meier method with log-rank tests.
Results
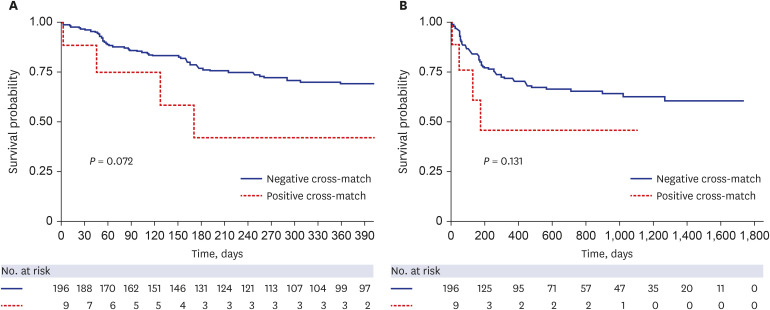
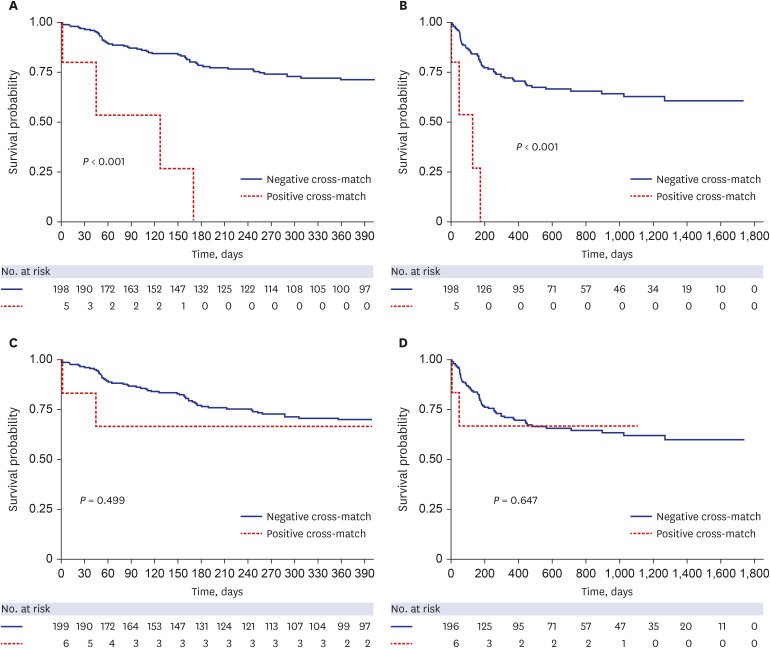
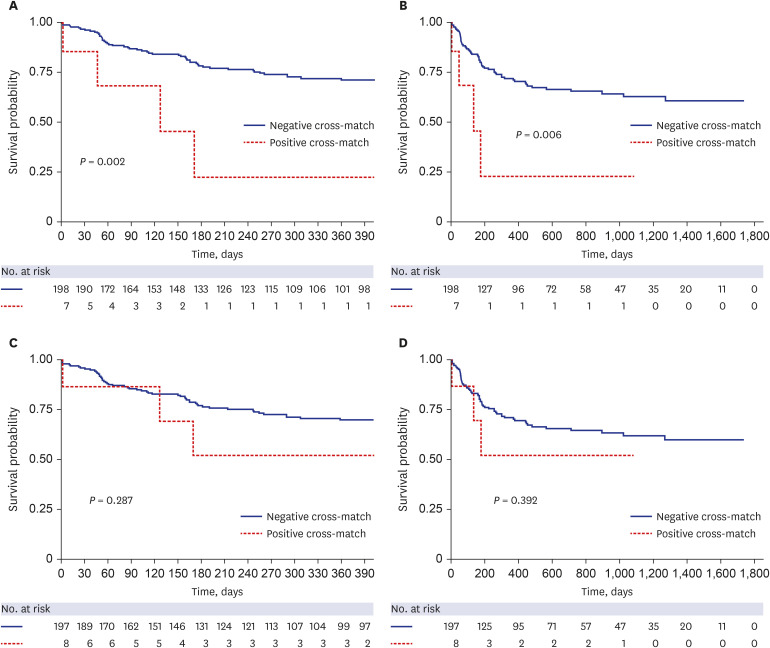
Complement-dependent cytotoxic crossmatch (CDC-XM) was performed in 208 patients (94.5%) and flow cytometric crossmatch (flow-XM) was performed in 125 patients (56.8%). Among them, nine patients (4.1%) showed T cell- and/or B cell-positive crossmatches. The incidences of postoperative complications, including primary graft dysfunction, acute rejection, and chronic allograft dysfunction in positively crossmatched patients, were not significant compared with those in patients without mismatches. Moreover, Kaplan-Meier analyses showed poorer 1-year survival in patients with positive crossmatch according to CDC-XM (P < 0.001) and T lymphocyte XM (P = 0.002) than in patients without mismatches.
Conclusion
Positive CDC and T lymphocyte crossmatching results should be considered in the allocation of donor lungs. If unavailable, the result should be considered for postoperative management in lung transplantation.
Figure
Reference
-
1. Patel R, Terasaki PI. Significance of the positive crossmatch test in kidney transplantation. N Engl J Med. 1969; 280(14):735–739. PMID: 4886455.2. Opelz G, Döhler B, Süsal C. Analysis of positive kidney, heart, and liver transplant crossmatches reported to the Collaborative Transplant Study. Hum Immunol. 2009; 70(8):627–630. PMID: 19375469.3. Tinckam KJ, Chandraker A. Mechanisms and role of HLA and non-HLA alloantibodies. Clin J Am Soc Nephrol. 2006; 1(3):404–414. PMID: 17699239.4. Fidler SJ, Irish AB, Lim W, Ferrari P, Witt CS, Christiansen FT. Pre-transplant donor specific anti-HLA antibody is associated with antibody-mediated rejection, progressive graft dysfunction and patient death. Transpl Immunol. 2013; 28(4):148–153. PMID: 23665534.5. Leech SH, Rubin S, Eisen HJ, Mather PJ, Goldman BI, McClurken JB, et al. Cardiac transplantation across a positive prospective lymphocyte cross-match in sensitized recipients. Clin Transplant. 2003; 17(Suppl 9):17–26. PMID: 12795663.6. Colvin MM, Cook JL, Chang PP, Hsu DT, Kiernan MS, Kobashigawa JA, et al. Sensitization in heart transplantation: emerging knowledge: a scientific statement from the American Heart Association. Circulation. 2019; 139(12):e553–e578. PMID: 30776902.7. Tait BD, Süsal C, Gebel HM, Nickerson PW, Zachary AA, Claas FH, et al. Consensus guidelines on the testing and clinical management issues associated with HLA and non-HLA antibodies in transplantation. Transplantation. 2013; 95(1):19–47. PMID: 23238534.8. Dick A, Humpe A, Kauke T. Impact, screening, and therapy of HLA antibodies in patients before and after lung transplantation. Transfus Med Hemother. 2019; 46(5):337–347. PMID: 31832059.9. Lobo LJ, Aris RM, Schmitz J, Neuringer IP. Donor-specific antibodies are associated with antibody-mediated rejection, acute cellular rejection, bronchiolitis obliterans syndrome, and cystic fibrosis after lung transplantation. J Heart Lung Transplant. 2013; 32(1):70–77. PMID: 23260706.10. Ju L, Suberbielle C, Li X, Mooney N, Charron D. HLA and lung transplantation. Front Med. 2019; 13(3):298–313. PMID: 29974325.11. Park MH, Kim S, Hwang H, Park H, Kwak J, Kwon EK, et al. Positive rates of preliminary crossmatches among transplantation candidates waitlisted for different organs in the Korean Network for Organ Sharing. Transplant Proc. 2016; 48(7):2464–2466. PMID: 27742323.12. Jeong YH, Kim DK, Choi S. Current status of lung transplantation in Korea. Curr Chall Thorac Surg. 2022; 4:4.13. Moon SW, Park MS, Lee JG, Paik HC, Kim YT, Lee HJ, et al. Panel-reactive and donor-specific antibodies before lung transplantation can affect outcomes in Korean patients receiving lung transplantation. Yonsei Med J. 2020; 61(7):606–613. PMID: 32608204.14. Yu WS, Kim SY, Kim YT, Lee HJ, Park S, Choi SM, et al. Characteristics of lung allocation and outcomes of lung transplant according to the Korean urgency status. Yonsei Med J. 2019; 60(10):992–997. PMID: 31538435.15. Hamrick CW, Lebeck LK. Flow cytometric T and B cell crossmatching. Hahn AB, Land GA, Strothman RM, editors. ASHI Laboratory Manual. 4th ed. Philadelphia, PA, USA: American Society for Histocompatibility and Immunogenetics;2000. p. 41–45.16. Smith JD, Danskine AJ, Laylor RM, Rose ML, Yacoub MH. The effect of panel reactive antibodies and the donor specific crossmatch on graft survival after heart and heart-lung transplantation. Transpl Immunol. 1993; 1(1):60–65. PMID: 8081763.17. Stewart S, Fishbein MC, Snell GI, Berry GJ, Boehler A, Burke MM, et al. Revision of the 1996 working formulation for the standardization of nomenclature in the diagnosis of lung rejection. J Heart Lung Transplant. 2007; 26(12):1229–1242. PMID: 18096473.18. Otani S, Davis AK, Cantwell L, Ivulich S, Pham A, Paraskeva MA, et al. Evolving experience of treating antibody-mediated rejection following lung transplantation. Transpl Immunol. 2014; 31(2):75–80. PMID: 25004453.19. Christie JD, Edwards LB, Kucheryavaya AY, Benden C, Dipchand AI, Dobbels F, et al. The registry of the International Society for Heart and Lung Transplantation: 29th adult lung and heart-lung transplant report-2012. J Heart Lung Transplant. 2012; 31(10):1073–1086. PMID: 22975097.20. Estenne M, Maurer JR, Boehler A, Egan JJ, Frost A, Hertz M, et al. Bronchiolitis obliterans syndrome 2001: an update of the diagnostic criteria. J Heart Lung Transplant. 2002; 21(3):297–310. PMID: 11897517.21. Sato M, Waddell TK, Wagnetz U, Roberts HC, Hwang DM, Haroon A, et al. Restrictive allograft syndrome (RAS): a novel form of chronic lung allograft dysfunction. J Heart Lung Transplant. 2011; 30(7):735–742. PMID: 21419659.22. Lyu DM, Goff RR, Chan KM. The lung allocation score and its relevance. Semin Respir Crit Care Med. 2021; 42(3):346–356. PMID: 34030198.23. Brugière O, Thabut G, Suberbielle C, Reynaud-Gaubert M, Thomas P, Pison C, et al. Relative impact of human leukocyte antigen mismatching and graft ischemic time after lung transplantation. J Heart Lung Transplant. 2008; 27(6):628–634. PMID: 18503962.24. Strüber M, Wilhelmi M, Harringer W, Niedermeyer J, Anssar M, Künsebeck A, et al. Flush perfusion with low potassium dextran solution improves early graft function in clinical lung transplantation. Eur J Cardiothorac Surg. 2001; 19(2):190–194. PMID: 11167111.25. Hopkins PM, McNeil K. Evidence for immunosuppression in lung transplantation. Curr Opin Organ Transplant. 2008; 13(5):477–483. PMID: 19060529.26. Smits JM, Mertens BJ, Van Houwelingen HC, Haverich A, Persijn GG, Laufer G. Predictors of lung transplant survival in Eurotransplant. Am J Transplant. 2003; 3(11):1400–1406. PMID: 14525601.27. Quantz MA, Bennett LE, Meyer DM, Novick RJ. Does human leukocyte antigen matching influence the outcome of lung transplantation? An analysis of 3,549 lung transplantations. J Heart Lung Transplant. 2000; 19(5):473–479. PMID: 10808155.28. Sutton PM, Harmer AH, Bayne AM, Welsh KI. The flow cytometric detection of alloantibodies in screening for renal transplantation. Transpl Int. 1995; 8(5):360–365. PMID: 7576017.29. Cervelli C, Pisani F, Aureli A, Azzarone R, Scimitarra M, Battistoni C, et al. For anti-HLA-specific donor antibodies detection by flow cytometry cytotoxic crossmatches comparison of methods. Transplant Proc. 2013; 45(7):2761–2764. PMID: 24034042.30. Mulley WR, Kanellis J. Understanding crossmatch testing in organ transplantation: a case-based guide for the general nephrologist. Nephrology (Carlton). 2011; 16(2):125–133. PMID: 21272123.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Cutcome of Living-related Renal Transplantation with Previously Positive but Currently Negative HLA Crossmatching
- Recent Advancement in Heart and Lung Transplantation
- Technical Aspects of Lung Transplantation: Pediatric and Lobar Transplantation
- Indications for Lung Transplantation and Patient Selection
- The assessment and outcomes of human leukocyte antigen mismatches of lung transplantation in Korean patients