J Pathol Transl Med.
2022 May;56(3):134-143. 10.4132/jptm.2022.02.22.
Expression of prostate-specific membrane antigen in the neovasculature of primary tumors and lymph node metastasis of laryngeal squamous cell carcinomas
- Affiliations
-
- 1Department of Pathology, Süleyman Demirel Univesity, Çünür/Isparta, Turkey
- 2Department of Otorhinolaryngology, Süleyman Demirel Univesity, Çünür/Isparta, Turkey
- KMID: 2529804
- DOI: http://doi.org/10.4132/jptm.2022.02.22
Abstract
- Background
Prostate-specific membrane antigen (PSMA) expression is encountered in tumor-associated neovascularization.
Methods
PSMA-antibody was applied to the paraffin blocks of 51 patients who were diagnosed with squamous cell carcinoma of the larynx and underwent laryngectomy and one who underwent lymph node dissection. The percentage of vascular expression in tumoral and extratumoral stroma and lymph nodes and intensity score in tumoral epithelium were evaluated and divided into groups according to the level of PSMA expression. Final PSMA expression was determined by multiplying intensity and percentage scores.
Results
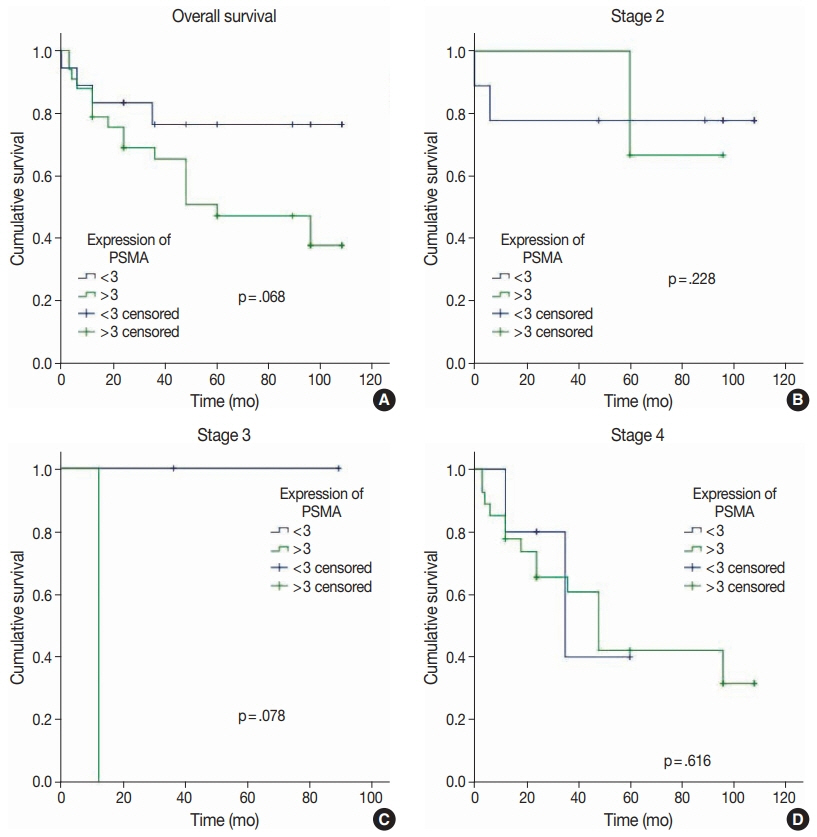
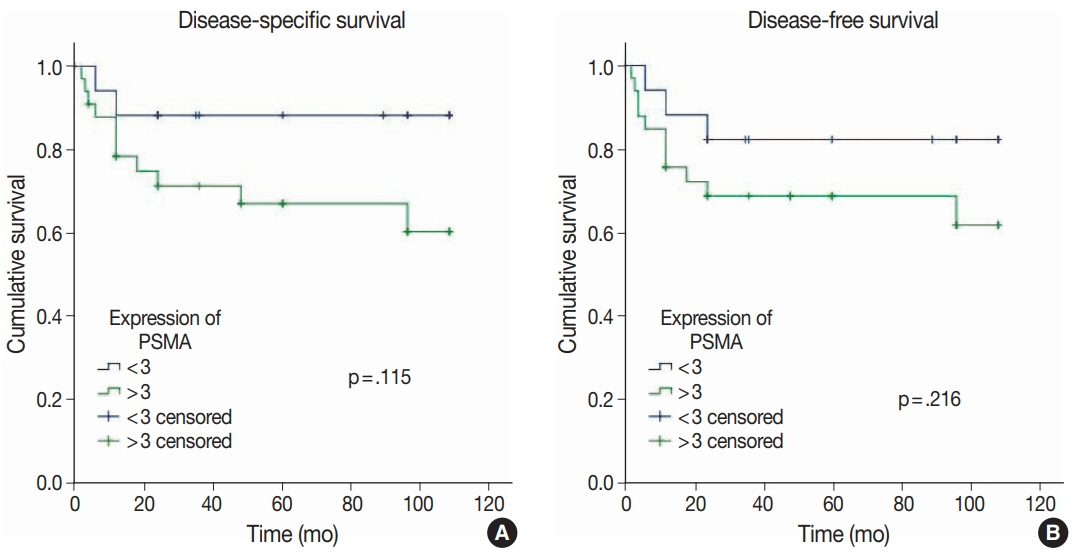
The mean age was 61±10 years. Patients with perineural invasion, cartilage invasion, and local invasion exhibited higher PSMA expression scores. Age, tumor differentiation, tumor diameter, perineural invasion, tumor localization, capsular invasion, depth of invasion, surgical margin status, local invasion, nodal metastasis, TNM classification, and stage were similar in high and low PSMA expression groups. There was no PSMA expression in extratumoral vascular stroma. Significantly higher PSMA expression was observed in the vascular endothelium of metastatic lymph nodes compared with reactive lymph nodes. Patients with advanced-stage disease exhibited higher PSMA vascular expression scores compared to those with earlier stages (p<.001). PSMA expression was not correlated with overall survival, disease-specific survival, or disease-free survival (p>.05).
Conclusions
Our study suggests that higher PSMA expression is associated with cartilage invasion, local invasion, and advanced-stage of disease. PSMA expression can be utilized for detection of lymph node metastasis and has some predictive role in cases of neck metastasis.
Keyword
Figure
Reference
-
References
1. Nocini R, Molteni G, Mattiuzzi C, Lippi G. Updates on larynx cancer epidemiology. Chin J Cancer Res. 2020; 32:18–25.
Article2. Prince A, Aguirre-Ghizo J, Genden E, Posner M, Sikora A. Head and neck squamous cell carcinoma: new translational therapies. Mt Sinai J Med. 2010; 77:684–99.
Article3. Rieger J, Kaessmeyer S, Al Masri S, Hunigen H, Plendl J. Endothelial cells and angiogenesis in the horse in health and disease: a review. Anat Histol Embryol. 2020; 49:656–78.4. Beatrice F, Valente G, Cammarota R, et al. Laryngeal cancer and angiogenesis. Acta Otorhinolaryngol Ital. 1996; 16:355–62.5. Chen X, Liang R, Zhu X. Anti-EGFR therapies in nasopharyngeal carcinoma. Biomed Pharmacother. 2020; 131:110649.
Article6. de Vries LH, Lodewijk L, Braat A, et al. (68)Ga-PSMA PET/CT in radioactive iodine-refractory differentiated thyroid cancer and first treatment results with (177)Lu-PSMA-617. EJNMMI Res. 2020; 10:18.
Article7. Rowe SP, Gorin MA, Pomper MG. Imaging of prostate-specific membrane antigen using [(18)F]DCFPyL. PET Clin. 2017; 12:289–96.
Article8. Bradbury R, Jiang WG, Cui YX. The clinical and therapeutic uses of MDM2 and PSMA and their potential interaction in aggressive cancers. Biomark Med. 2015; 9:1353–70.
Article9. Van de Wiele C, Sathekge M, de Spiegeleer B, et al. PSMA expression on neovasculature of solid tumors. Histol Histopathol. 2020; 35:919–27.10. Gale N, Poljak M, Zidar N. Update from the 4th Edition of the World Health Organization classification of head and neck tumours: what is new in the 2017 WHO blue book for tumours of the hypopharynx, larynx, trachea and parapharyngeal space. Head Neck Pathol. 2017; 11:23–32.
Article11. Seethala RR, Weinreb I, Bullock MJ, et al. Protocol for the examination of specimens from patients with carcinomas of the larynx. Northfield: College of American Pathologists;2019.12. Wernicke AG, Varma S, Greenwood EA, et al. Prostate-specific membrane antigen expression in tumor-associated vasculature of breast cancers. APMIS. 2014; 122:482–9.
Article13. Wernicke AG, Kim S, Liu H, Bander NH, Pirog EC. Prostate-specific membrane antigen (PSMA) expression in the neovasculature of gynecologic malignancies: implications for PSMA-targeted therapy. Appl Immunohistochem Mol Morphol. 2017; 25:271–6.
Article14. Haffner MC, Laimer J, Chaux A, et al. High expression of prostatespecific membrane antigen in the tumor-associated neo-vasculature is associated with worse prognosis in squamous cell carcinoma of the oral cavity. Mod Pathol. 2012; 25:1079–85.
Article15. Silver DA, Pellicer I, Fair WR, Heston WD, Cordon-Cardo C. Prostate-specific membrane antigen expression in normal and malignant human tissues. Clin Cancer Res. 1997; 3:81–5.16. Kasoha M, Unger C, Solomayer EF, et al. Prostate-specific membrane antigen (PSMA) expression in breast cancer and its metastases. Clin Exp Metastasis. 2017; 34:479–90.
Article17. Lin PP. Aneuploid circulating tumor-derived endothelial cell (CTEC): a novel versatile player in tumor neovascularization and cancer metastasis. Cells. 2020; 9:1539.
Article18. Butkiewicz D, Gdowicz-Klosok A, Krzesniak M, et al. Association of genetic variants in ANGPT/TEK and VEGF/VEGFR with progression and survival in head and neck squamous cell carcinoma treated with radiotherapy or radiochemotherapy. Cancers (Basel). 2020; 12:1506.
Article19. Kupisz K, Chibowski D, Klatka J, Klonowski S, Stepulak A. Tumor angiogenesis in patients with laryngeal cancer. Eur Arch Otorhinolaryngol. 1999; 256:303–5.
Article20. Schluter A, Weller P, Kanaan O, et al. CD31 and VEGF are prognostic biomarkers in early-stage, but not in late-stage, laryngeal squamous cell carcinoma. BMC Cancer. 2018; 18:272.
Article21. Sawatsubashi M, Yamada T, Fukushima N, Mizokami H, Tokunaga O, Shin T. Association of vascular endothelial growth factor and mast cells with angiogenesis in laryngeal squamous cell carcinoma. Virchows Arch. 2000; 436:243–8.
Article22. Rodrigo JP, Cabanillas R, Chiara MD, Garcia Pedrero J, Astudillo A, Suarez Nieto C. Prognostic significance of angiogenesis in surgically treated supraglottic squamous cell carcinomas of the larynx. Acta Otorrinolaringol Esp. 2009; 60:272–7.
Article23. Heitkotter B, Trautmann M, Grunewald I, et al. Expression of PSMA in tumor neovasculature of high grade sarcomas including synovial sarcoma, rhabdomyosarcoma, undifferentiated sarcoma and MPNST. Oncotarget. 2017; 8:4268–76.
Article24. Heitkotter B, Steinestel K, Trautmann M, et al. Neovascular PSMA expression is a common feature in malignant neoplasms of the thyroid. Oncotarget. 2018; 9:9867–74.
Article25. Jiao D, Li Y, Yang F, et al. Expression of prostate-specific membrane antigen in tumor-associated vasculature predicts poor prognosis in hepatocellular carcinoma. Clin Transl Gastroenterol. 2019; 10:1–7.
Article26. Franchi A, Gallo O, Paglierani M, et al. Inducible nitric oxide synthase expression in laryngeal neoplasia: correlation with angiogenesis. Head Neck. 2002; 24:16–23.
Article27. White CW, Sondheimer HM, Crouch EC, Wilson H, Fan LL. Treatment of pulmonary hemangiomatosis with recombinant interferon alfa-2a. N Engl J Med. 1989; 320:1197–200.
Article28. Folkman J. Seminars in Medicine of the Beth Israel Hospital, Boston. Clinical applications of research on angiogenesis. N Engl J Med. 1995; 333:1757–63.29. Eisen T, Boshoff C, Mak I, et al. Continuous low dose thalidomide: a phase II study in advanced melanoma, renal cell, ovarian and breast cancer. Br J Cancer. 2000; 82:812–7.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- VEGF Expression and Microvessel Density in Oral Squamous Cell Carcinomas
- Expression of e-cadherin with correlation to clinicopathologic parameters in oral squamous cell carcinoma
- Expression of p53 and nm23 Proteins in Non-Small Cell Lung Cancer
- Expression of p53 and MHC Class I According to HPV Infection in Laryngeal Squamous Cell Carcinomas
- A Study on the Type IV Collagen Expression in the Basement Membrane Surrounding the Cancer Nest(Cancer Nest Membrane) and Cervical Lymph Node Metastasis of Head and Neck Squamous Cell Carcinoma