J Korean Neurosurg Soc.
2022 May;65(3):469-478. 10.3340/jkns.2021.0240.
Clinical Grading System, Surgical Outcomes and Prognostic Analysis of Cranial Base Chordomas
- Affiliations
-
- 1School of Medicine, Nankai University, Tianjin, China
- 2Department of Neurosurgery, Tianjin Huanhu Hospital, Tianjin, China
- KMID: 2529592
- DOI: http://doi.org/10.3340/jkns.2021.0240
Abstract
Objective
: Cranial base chordomas are rare, but their treatment is challenging. Tumor recurrence is still common despite improvements in microsurgical techniques and postoperative radiotherapy. We retrospectively analyzed the course of treatment, overall survival, and recurrence/progression of chordomas over the past 10 years.
Methods
: We retrospectively reviewed 50 patients who underwent surgery at Tianjin Huanhu Hospital between 2010 and 2020 and were pathologically diagnosed with chordomas. Tumor resection was performed within the maximum safe range in all patients; the extent of resection was evaluated by imaging; and the incidence of complications, recurrence or progression, and overall survival were assessed.
Results
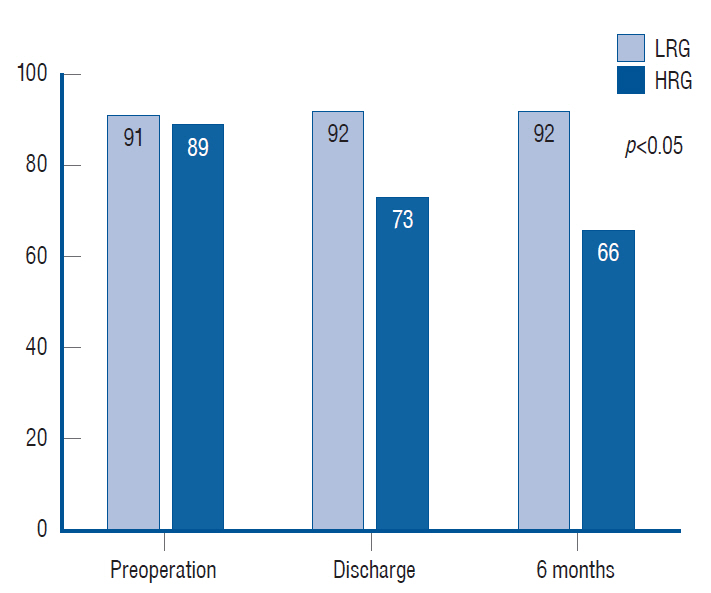
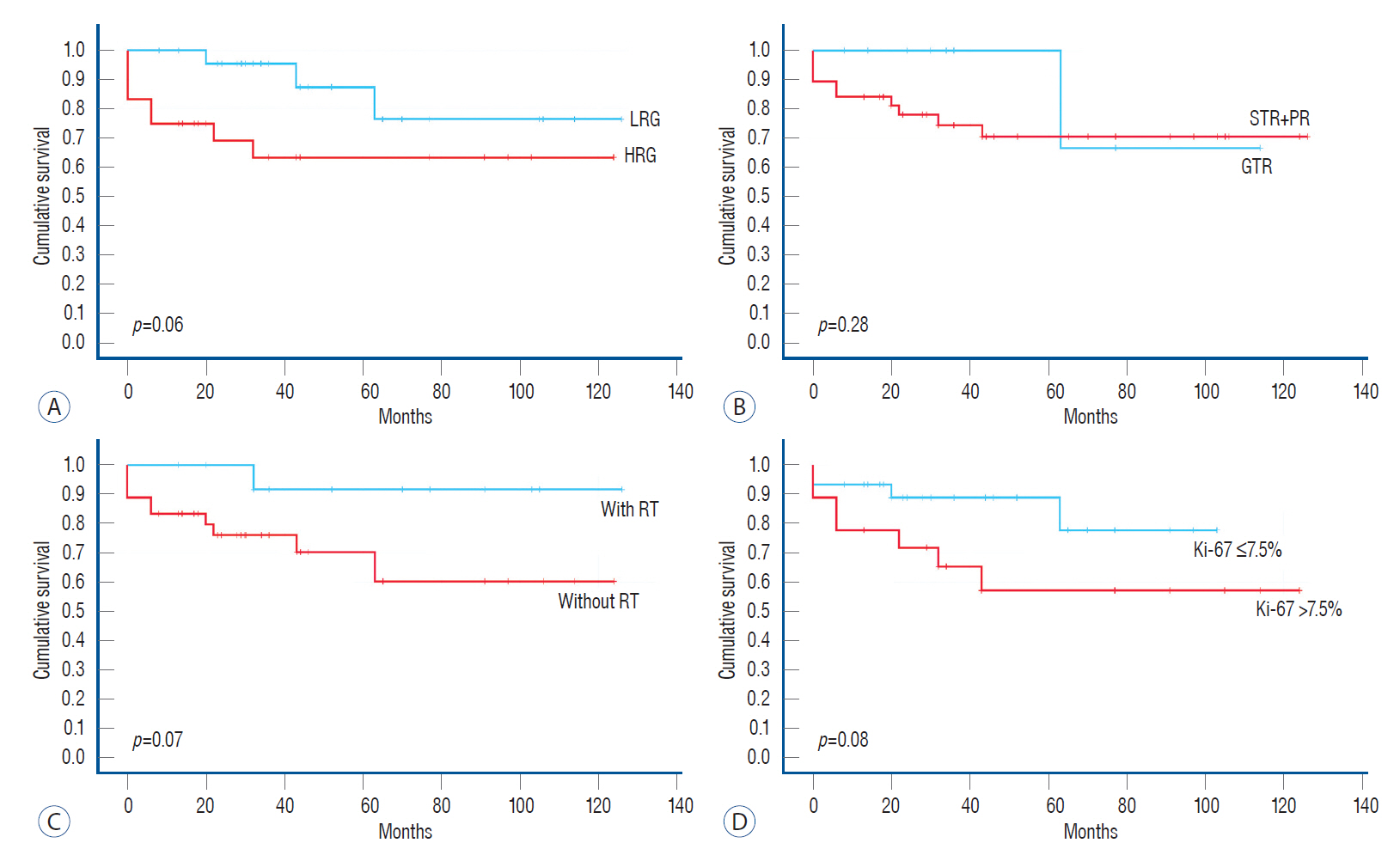
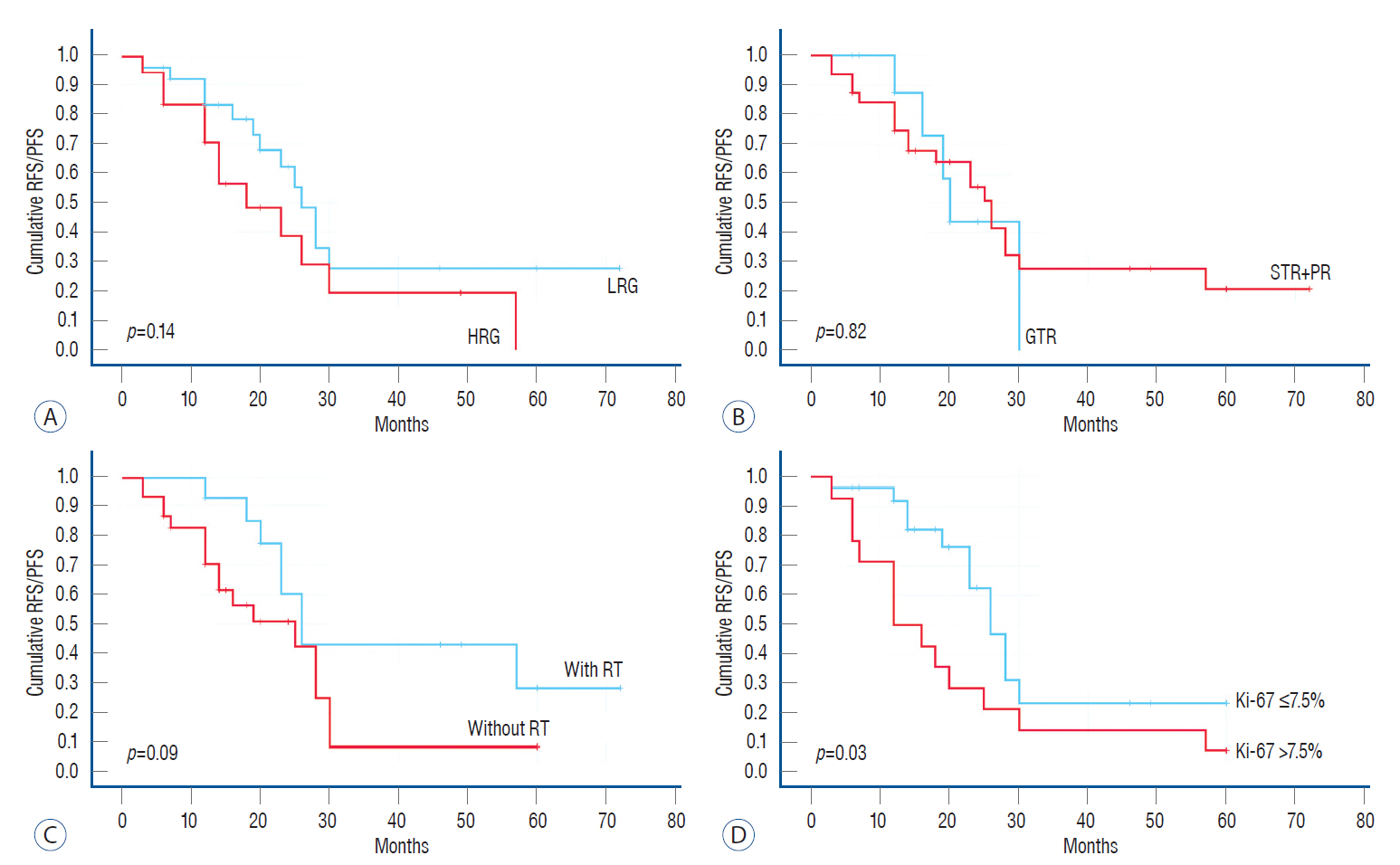
: Fifty patients were divided into the low-risk group (LRG) and high-risk group (HRG) based on the cranial chordoma grading system (CCGS). The Karnofsky Performance Scale scores and gross total resection rate of the LRG were significantly higher than those of the HRG (p<0.05). The incidence of complications and mortality in the LRG were lower than those of HRG. The analysis of cumulative survival and cumulative recurrence free survival/progression free survival (RFS/PFS) showed no statistical differences in the extent of resection for survival, recurrence, or progression. Univariate and multivariate analyses showed that Ki-67 was significantly associated with tumor recurrence and was an independent hazard factor (p=0.02).
Conclusion
: The CCGS can help neurosurgeons anticipate surgical outcomes. Pathological results are important in evaluating the possibility of tumor recurrence, and postoperative radiotherapy improves overall survival and RFS/PFS.
Keyword
Figure
Reference
-
References
1. al-Mefty O, Borba LA. Skull base chordomas: a management challenge. J Neurosurg. 86:182–189. 1997.
Article2. Brito da Silva H, Straus D, Barber JK, Rostomily RC, Ferreira M Jr, Sekhar LN. Cranial chordoma: a new preoperative grading system. Neurosurgery. 83:403–415. 2018.3. Choy W, Terterov S, Kaprealian TB, Trang A, Ung N, Desalles A, et al. Predictors of recurrence following resection of intracranial chordomas. J Clin Neurosci. 22:1792–1796. 2015.
Article4. Colli B, Al-Mefty O. Chordomas of the craniocervical junction: follow-up review and prognostic factors. J Neurosurg. 95:933–943. 2001.
Article5. Colli BO, Al-Mefty O. Chordomas of the skull base: follow-up review and prognostic factors. Neurosurg Focus. 10:E1. 2001.
Article6. Diaz RJ, Maggacis N, Zhang S, Cusimano MD. Determinants of quality of life in patients with skull base chordoma. J Neurosurg. 120:528–537. 2014.
Article7. Di Maio S, Rostomily R, Sekhar LN. Current surgical outcomes for cranial base chordomas: cohort study of 95 patients. Neurosurgery. 70:1355–1360. discussion 1360. 2012.8. Di Maio S, Temkin N, Ramanathan D, Sekhar LN. Current comprehensive management of cranial base chordomas: 10-year meta-analysis of observational studies. J Neurosurg. 115:1094–1105. 2011.
Article9. Eid AS, Chang UK, Lee SY, Jeon DG. The treatment outcome depending on the extent of resection in skull base and spinal chordomas. Acta Neurochir (Wien). 153:509–516. 2011.
Article10. Forsyth PA, Cascino TL, Shaw EG, Scheithauer BW, O’Fallon JR, Dozier JC, et al. Intracranial chordomas: a clinicopathological and prognostic study of 51 cases. J Neurosurg. 78:741–747. 1993.
Article11. Gay E, Sekhar LN, Rubinstein E, Wright DC, Sen C, Janecka IP, et al. Chordomas and chondrosarcomas of the cranial base: results and follow-up of 60 patients. Neurosurgery. 36:887–897. discussion 896-897. 1995.12. Gui S, Zong X, Wang X, Li C, Zhao P, Cao L, et al. Classification and surgical approaches for transnasal endoscopic skull base chordoma resection: a 6-year experience with 161 cases. Neurosurg Rev. 39:321–332. discussion 332-333. 2016.
Article13. Hoch BL, Nielsen GP, Liebsch NJ, Rosenberg AE. Base of skull chordomas in children and adolescents: a clinicopathologic study of 73 cases. Am J Surg Pathol. 30:811–818. 2006.14. Jägersberg M, El Rahal A, Dammann P, Merkler D, Weber DC, Schaller K. Clival chordoma: a single-centre outcome analysis. Acta Neurochir (Wien). 159:1815–1823. 2017.
Article15. Jahangiri A, Chin AT, Wagner JR, Kunwar S, Ames C, Chou D, et al. Factors predicting recurrence after resection of clival chordoma using variable surgical approaches and radiation modalities. Neurosurgery. 76:179–185. discussion 185-186. 2015.
Article16. Korten AG, ter Berg HJ, Spincemaille GH, van der Laan RT, Van de Wel AM. Intracranial chondrosarcoma: review of the literature and report of 15 cases. J Neurol Neurosurg Psychiatry. 65:88–92. 1998.
Article17. McMaster ML, Goldstein AM, Bromley CM, Ishibe N, Parry DM. Chordoma: incidence and survival patterns in the United States, 1973-1995. Cancer Causes Control. 12:1–11. 2001.18. Nishigaya K, Kaneko M, Ohashi Y, Nukui H. Intradural retroclival chordoma without bone involvement: no tumor regrowth 5 years after operation. Case report. J Neurosurg. 88:764–768. 1998.
Article19. Ormerod R. A case of chordoma presenting in the nasopharynx. J Laryngol Otol. 74:245–254. 1960.
Article20. Roberti F, Sekhar LN, Kalavakonda C, Wright DC. Posterior fossa meningiomas: surgical experience in 161 cases. Surg Neurol. 56:8–20. discussion 20-21. 2001.
Article21. Samii A, Gerganov VM, Herold C, Hayashi N, Naka T, Mirzayan MJ, et al. Chordomas of the skull base: surgical management and outcome. J Neurosurg. 107:319–324. 2007.
Article22. Smoll NR, Gautschi OP, Radovanovic I, Schaller K, Weber DC. Incidence and relative survival of chordomas: the standardized mortality ratio and the impact of chordomas on a population. Cancer. 119:2029–2037. 2013.23. Soo MY. Chordoma: review of clinicoradiological features and factors affecting survival. Australas Radiol. 45:427–437. 2001.
Article24. Stacchiotti S, Sommer J, Chordoma Global Consensus Group. Building a global consensus approach to chordoma: a position paper from the medical and patient community. Lancet Oncol. 16:e71–e83. 2015.
Article25. Thodou E, Kontogeorgos G, Scheithauer BW, Lekka I, Tzanis S, Mariatos P, et al. Intrasellar chordomas mimicking pituitary adenoma. J Neurosurg. 92:976–982. 2000.
Article26. Tzortzidis F, Elahi F, Wright D, Natarajan SK, Sekhar LN. Patient outcome at long-term follow-up after aggressive microsurgical resection of cranial base chordomas. Neurosurgery. 59:230–237. discussion 230-237. 2006.
Article27. Walcott BP, Nahed BV, Mohyeldin A, Coumans JV, Kahle KT, Ferreira MJ. Chordoma: current concepts, management, and future directions. Lancet Oncol. 13:e69–e76. 2012.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical Strategy for Skull Base Chordomas : Transnasal Midline Approach or Transcranial Lateral Approach
- Intracranial Chordomas:Clinical Review and Therapeutic Outcome
- A longitudinal study on the growth of the cranial base
- The Outcome of Surgery Treatment of Cranial Base Meningiomas
- Correlation between Histologic Differentiation and Prognosis of Prostate Adenocarcinoma