J Korean Neurosurg Soc.
2022 May;65(3):422-429. 10.3340/jkns.2021.0198.
Long-Term Outcomes of Stenting on Non-Acute Phase Extracranial Supra-Aortic Dissections
- Affiliations
-
- 1Department of Radiology, Huashan Hospital Affiliated to Fudan University, Shanghai, China
- KMID: 2529587
- DOI: http://doi.org/10.3340/jkns.2021.0198
Abstract
Objective
: Extracranial supra-aortic dissections (ESADs) with severe stenosis, occlusion and/or pseudoaneurysm presents potential risk of stroke. Endovascular stenting to reconstruct non acute phase ESADs (NAP-ESADs) is an alternative to anticoagulant or antiplatelet therapy. However, its feasibility, safety and efficacy of stenting in NAP-ESADs is unclear. This study aims to investigate the long-term outcomes of the feasibility, safety and efficacy of stenting in NAP-ESADs.
Methods
: Seventy-four patients with 91 NAP-ESAD vessels with severe stenosis, occlusion and/or pseudoaneurysm presents potential risk of stroke who underwent stent remodeling were enrolled into this respective study from December 2008 to March 2020. Technical success rate, complications, clinical and angiographic results were harvested and analyzed.
Results
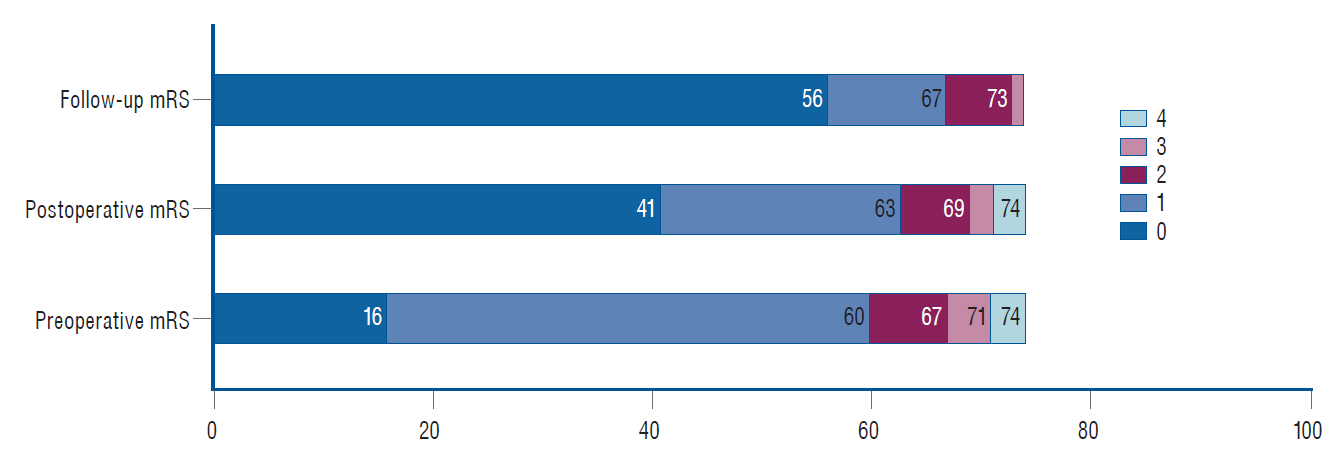
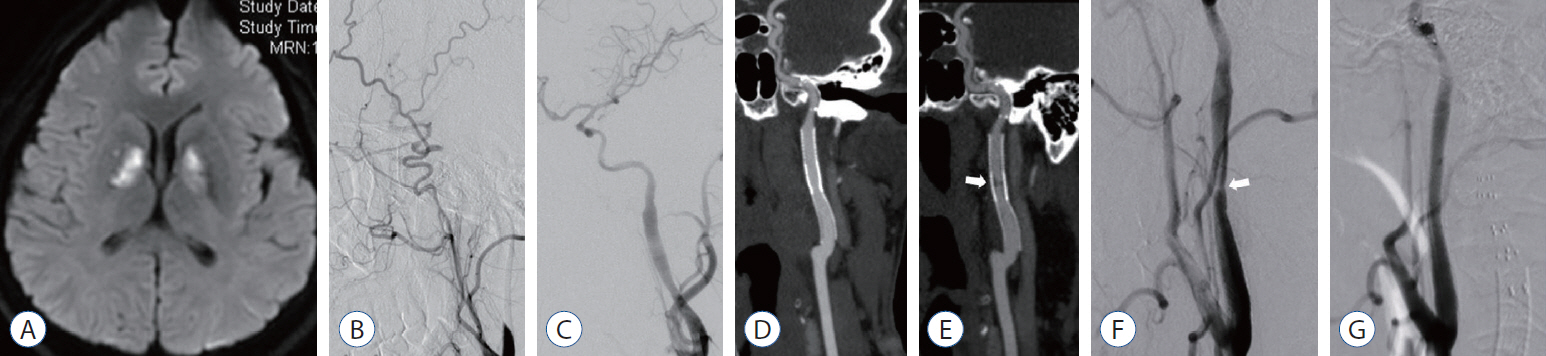
: Success rate of stent deployment was 99% (90/91) with no procedural mortality or morbidity. Transient ischemic attack occurred in three patients during operation (4.1%, 3/74). Asymptomatic embolisms of distal intracranial vessels were found in two patients (2.7%, 2/74). One hundred and forty-two stents deployed at 85 carotid (135 stents) and six vertebral (seven stents) vessels. Six stent types (Wingspan, 28/135, 20.7%; Solitaire, 10/135, 7.4%; Neuroform, 8/135, 5.9%; LVIS, 2/135, 1.5%; Precise, 75/135, 55.6%; Acculink, 12/135, 8.9%) were deployed at carotid arterial dissection while two types (Wingspan, 5/7, 71.4%; Solitaire 2/7, 28.6%) at vertebral arterial dissection. Digital subtracted angiography (56%, 51/91), computational tomography angiography (41.8%, 38/91) and high resolution magnetic resonance imaging (2.2%, 2/91) were adopted for follow up, with a mean time of 17.2±15.4 months (5–77). All patient modified Rankin Scale scores showed no increase at discharge or follow-up. Angiographically, dissections in 86 vessels in 69 patients (94.5%, 86/91) were completely reconstructed with only minor remnant dissections in four vessels in four patients (4.4%, 4/91). Severe re-stenosis in the stented segment required re-stenting in one patient (1.1%, 1/91).
Conclusion
: Stent remodeling technique provides feasible, safe and efficacious treatment of ESADs patients with severe stenosis, occlusion and/or pseudoaneurysm.
Keyword
Figure
Reference
-
References
1. Ansari SA, Thompson BG, Gemmete JJ, Gandhi D. Endovascular treatment of distal cervical and intracranial dissections with the neuroform stent. Neurosurgery. 62:636–646. discussion 636-646. 2008.
Article2. Biller J, Sacco RL, Albuquerque FC, Demaerschalk BM, Fayad P, Long PH, et al. Cervical arterial dissections and association with cervical manipulative therapy: a statement for healthcare professionals from the american heart association/american stroke association. Stroke. 45:3155–3174. 2014.
Article3. Delgado F, Bravo I, Jiménez E, Murías E, Saiz A, Vega P, et al. Endovascular treatment in the acute and non-acute phases of carotid dissection: a therapeutic approach. J Neurointerv Surg. 9:11–16. 2017.
Article4. Edgell RC, Abou-Chebl A, Yadav JS. Endovascular management of spontaneous carotid artery dissection. J Vasc Surg. 42:854–860. discussion 860. 2005.
Article5. Farouk M, Sato K, Matsumoto Y, Tominaga T. Endovascular treatment of internal carotid artery dissection presenting with acute ischemic stroke. J Stroke Cerebrovasc Dis. 29:104592. 2020.
Article6. Fava M, Meneses L, Loyola S, Tevah J, Bertoni H, Huete I, et al. Carotid artery dissection: endovascular treatment. Report of 12 patients. Catheter Cardiovasc Interv. 71:694–700. 2008.
Article7. Koge J, Iwata T, Mizuta S, Nakamura Y, Matsumoto SI, Yamada T. Successful carotid artery stenting of a dissected, highly tortuous internal carotid artery after straightening with a peripheral microguidewire. J Clin Neurosci. 53:265–268. 2018.
Article8. Lee YJ, Ahn JY, Han IB, Chung YS, Hong CK, Joo JY. Therapeutic endovascular treatments for traumatic vertebral artery injuries. J Trauma. 62:886–891. 2007.
Article9. Leys D, Bandu L, Hénon H, Lucas C, Mounier-Vehier F, Rondepierre P, et al. Clinical outcome in 287 consecutive young adults (15 to 45 years) with ischemic stroke. Neurology. 59:26–33. 2002.
Article10. Li MKA, Tsang ACO, Tsang FCP, Ho WS, Lee R, Leung GKK, et al. Long-term risk of in-stent restenosis and stent fracture for extracranial vertebral artery stenting. Clin Neuroradiol. 29:701–706. 2019.
Article11. Mehta T, Patel S, Male S, Parikh R, Mehta K, Lakshminarayan K, et al. Unplanned 30-day hospital readmissions of symptomatic carotid and vertebral artery dissection. J Stroke. 20:407–410. 2018.
Article12. Pham MH, Rahme RJ, Arnaout O, Hurley MC, Bernstein RA, Batjer HH, et al. Endovascular stenting of extracranial carotid and vertebral artery dissections: a systematic review of the literature. Neurosurgery. 68:856–866. discussion 866. 2011.
Article13. Rahal JP, Gao B, Safain MG, Malek AM. Stent recanalization of carotid tonsillar loop dissection using the enterprise vascular reconstruction device. J Clin Neurosci. 21:1141–1147. 2014.
Article14. Robertson JJ, Koyfman A. Cervical artery dissections: a review. J Emerg Med. 51:508–518. 2016.
Article15. Schievink WI. Spontaneous dissection of the carotid and vertebral arteries. N Engl J Med. 344:898–906. 2001.
Article16. Schulte S, Donas KP, Pitoulias GA, Horsch S. Endovascular treatment of iatrogenic and traumatic carotid artery dissection. Cardiovasc Intervent Radiol. 31:870–874. 2008.
Article17. Seifert T, Klein E, Legat-Wallner S, Krenn U, Brussee H, Lueger A, et al. Bilateral vertebral artery dissection and infratentorial stroke complicated by stress-induced cardiomyopathy. J Neurol Neurosurg Psychiatry. 79:480–481. 2008.
Article18. Urasyanandana K, Songsang D, Aurboonyawat T, Chankaew E, Withayasuk P, Churojana A. Treatment outcomes in cerebral artery dissection and literature review. Interv Neuroradiol. 24:254–262. 2018.
Article19. Wang J, Yue D, Chen X, Wei Z, Lu W, Wu D. Common carotid artery dissection caused by radiotherapy: a case report. Mol Clin Oncol. 5:475–477. 2016.
Article20. Zanaty M, Roa JA, Jabbour PM, Samaniego EA, Hasan DM. Recanalization of the chronically occluded internal carotid artery: review of the literature. World Neurosurg X. 5:100067. 2020.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Long-Term Changes in the Distal Aorta after Aortic Arch Replacement in Acute DeBakey Type I Aortic Dissection
- Hrombosed Aortic Dissections and Aortic Aneurysms: MRI Findings and Differential Diagnosis
- Contralateral Cerebral Infarction after Stent Placement in Carotid Artery : An Unexpected Complication
- Outcomes of Emergent Carotid Artery Stenting within 6 Hours of Symptom Onset in Patients with Acute Ischemic Stroke
- Mid-term Outcomes of Thoracic Endovascular Aortic Repair (TEVAR) in Acute Complicated Type B Aortic Dissection: A Comprehensive Analysis of Aortic Remodeling Patterns