Endocrinol Metab.
2022 Apr;37(2):323-332. 10.3803/EnM.2022.1413.
Usefulness of Real-Time Quantitative Microvascular Ultrasonography for Differentiation of Graves’ Disease from Destructive Thyroiditis in Thyrotoxic Patients
- Affiliations
-
- 1Division of Endocrinology and Metabolism, Department of Internal Medicine Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Division of Endocrinology and Metabolism, Department of Internal Medicine, Uijeongbu St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Uijeongbu, Korea
- KMID: 2529224
- DOI: http://doi.org/10.3803/EnM.2022.1413
Abstract
- Background
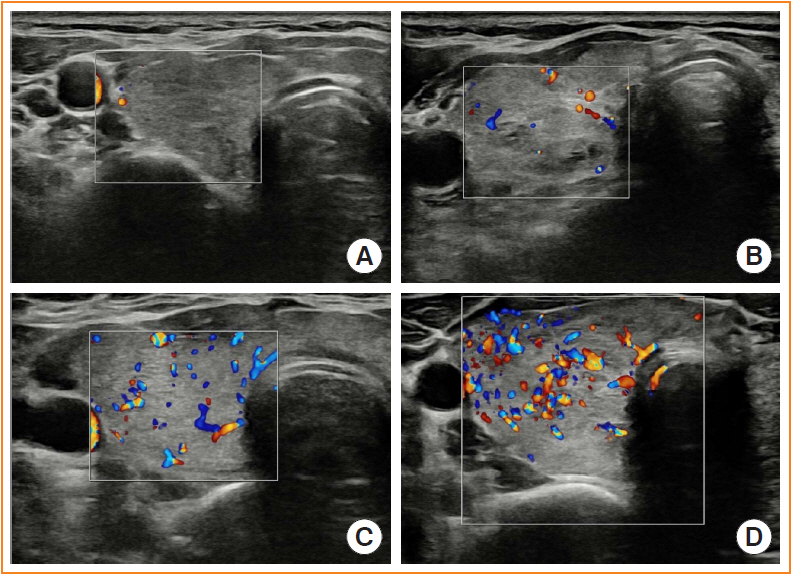
Microvascular ultrasonography (MVUS) is a third-generation Doppler technique that was developed to increase sensitivity compared to conventional Doppler. The purpose of this study was to compare MVUS with conventional color Doppler (CD) and power Doppler (PD) imaging to distinguish Graves’ disease (GD) from destructive thyroiditis (DT).
Methods
This prospective study included 101 subjects (46 GDs, 47 DTs, and eight normal controls) from October 2020 to November 2021. All ultrasonography examinations were performed using microvascular flow technology (MV-Flow). The CD, PD, and MVUS images were semi-quantitatively graded according to blood flow patterns. On the MVUS images, vascularity indices (VIs), which were the ratio (%) of color pixels in the total grayscale pixels in a defined region of interest, were obtained automatically. Receiver operating characteristic curve analysis was performed to verify the diagnostic performance of MVUS. The interclass correlation coefficient and Cohen’s kappa analysis were used to analyze the reliability of MVUS (ClinicalTrials.gov:NCT04879173).
Results
The area under the curve (AUC) for CD, PD, MVUS, and MVUS-VI was 0.822, 0.844, 0.808, and 0.852 respectively. The optimal cutoff value of the MVUS-VI was 24.95% for distinguishing GD and DT with 87% sensitivity and 80.9% specificity. We found a significant positive correlation of MVUS-VI with thyrotropin receptor antibody (r=0.554) and with thyroid stimulating immunoglobulin bioassay (r=0.841). MVUS showed high intra- and inter-observer reliability from various statistical method.
Conclusion
In a real time and quantitative manner, MVUS-VI could be helpful to differentiate GD from thyroiditis in thyrotoxic patients, with less inter-observer variability.
Keyword
Figure
Cited by 1 articles
-
The Early Changes in Thyroid-Stimulating Immunoglobulin Bioassay over Anti-Thyroid Drug Treatment Could Predict Prognosis of Graves’ Disease
Jin Yu, Han-Sang Baek, Chaiho Jeong, Kwanhoon Jo, Jeongmin Lee, Jeonghoon Ha, Min Hee Kim, Jungmin Lee, Dong-Jun Lim
Endocrinol Metab. 2023;38(3):338-346. doi: 10.3803/EnM.2023.1664.
Reference
-
1. Kahaly GJ. Management of Graves thyroidal and extrathyroidal disease: an update. J Clin Endocrinol Metab. 2020; 105:3704–20.
Article2. Chung JH. Antithyroid drug treatment in Graves’ disease. Endocrinol Metab (Seoul). 2021; 36:491–9.
Article3. Alzahrani AS, Ceresini G, Aldasouqi SA. Role of ultrasonography in the differential diagnosis of thyrotoxicosis: a noninvasive, cost-effective, and widely available but underutilized diagnostic tool. Endocr Pract. 2012; 18:567–78.4. Hiromatsu Y, Ishibashi M, Miyake I, Soyejima E, Yamashita K, Koike N, et al. Color Doppler ultrasonography in patients with subacute thyroiditis. Thyroid. 1999; 9:1189–93.
Article5. Donkol RH, Nada AM, Boughattas S. Role of color Doppler in differentiation of Graves’ disease and thyroiditis in thyrotoxicosis. World J Radiol. 2013; 5:178–83.
Article6. Rosario PW, Santos JB, Nunes NS, da Silva AL, Calsolari MR. Color flow Doppler sonography for the etiologic diagnosis of thyrotoxicosis. Horm Metab Res. 2014; 46:505–9.
Article7. Yoo J, Je BK, Choo JY. Ultrasonographic demonstration of the tissue microvasculature in children: microvascular ultrasonography versus conventional color Doppler ultrasonography. Korean J Radiol. 2020; 21:146–58.
Article8. Xiao XY, Chen X, Guan XF, Wu H, Qin W, Luo BM. Superb microvascular imaging in diagnosis of breast lesions: a comparative study with contrast-enhanced ultrasonographic microvascular imaging. Br J Radiol. 2016; 89:20160546.
Article9. Dubinsky TJ, Revels J, Wang S, Toia G, Sonneborn R, Hippe DS, et al. Comparison of superb microvascular imaging with color flow and power Doppler imaging of small hepatocellular carcinomas. J Ultrasound Med. 2018; 37:2915–24.
Article10. Durmaz MS, Sivri M. Comparison of superb micro-vascular imaging (SMI) and conventional Doppler imaging techniques for evaluating testicular blood flow. J Med Ultrason (2001). 2018; 45:443–52.
Article11. Ahn HS, Lee JB, Seo M, Park SH, Choi BI. Distinguishing benign from malignant thyroid nodules using thyroid ultrasonography: utility of adding superb microvascular imaging and elastography. Radiol Med. 2018; 123:260–70.
Article12. Zhu YC, Zhang Y, Deng SH, Jiang Q. A prospective study to compare superb microvascular imaging with grayscale ultrasound and color Doppler flow imaging of vascular distribution and morphology in thyroid nodules. Med Sci Monit. 2018; 24:9223–31.
Article13. Cappelli C, Pirola I, Gandossi E, Marini F, Cristiano A, Casella C, et al. Ultrasound microvascular blood flow evaluation: a new tool for the management of thyroid nodule? Int J Endocrinol. 2019; 2019:7874890.
Article14. Sarikaya B, Demirbilek H, Akata D, Kandemir N. The role of the resistive index in Hashimoto’s thyroiditis: a sonographic pilot study in children. Clinics (Sao Paulo). 2012; 67:1253–7.
Article15. Ota H, Amino N, Morita S, Kobayashi K, Kubota S, Fukata S, et al. Quantitative measurement of thyroid blood flow for differentiation of painless thyroiditis from Graves’ disease. Clin Endocrinol (Oxf). 2007; 67:41–5.
Article16. Vita R, Di Bari F, Perelli S, Capodicasa G, Benvenga S. Thyroid vascularization is an important ultrasonographic parameter in untreated Graves’ disease patients. J Clin Transl Endocrinol. 2019; 15:65–9.
Article17. Corona G, Biagini C, Rotondi M, Bonamano A, Cremonini N, Petrone L, et al. Correlation between, clinical, biochemical, color Doppler ultrasound thyroid parameters, and CXCL-10 in autoimmune thyroid diseases. Endocr J. 2008; 55:345–50.
Article18. Bogazzi F, Bartalena L, Brogioni S, Burelli A, Manetti L, Tanda ML, et al. Thyroid vascularity and blood flow are not dependent on serum thyroid hormone levels: studies in vivo by color flow doppler sonography. Eur J Endocrinol. 1999; 140:452–6.
Article19. Bayramoglu Z, Kandemirli SG, Akyol Sari ZN, Kardelen AD, Poyrazoglu S, Bas F, et al. Superb microvascular imaging in the evaluation of pediatric Graves disease and Hashimoto thyroiditis. J Ultrasound Med. 2020; 39:901–9.
Article20. Shih SR, Chang JS, Lin LC, Chang YC, Li HY, Lee CY, et al. The relationship between thyrotropin receptor antibody levels and intrathyroid vascularity in patients with Graves’ disease. Exp Clin Endocrinol Diabetes. 2013; 121:1–5.
Article21. Kim J. ROC curves and sample size and inferiority [Internet]. Statistics4everyone;2021; [cited 2022 Mar 25]. Available from: https://data-play3.shinyapps.io/ROC_pretty/.22. Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016; 15:155–63.
Article23. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977; 33:159–74.
Article24. Scappaticcio L, Trimboli P, Keller F, Imperiali M, Piccardo A, Giovanella L. Diagnostic testing for Graves’ or non-Graves’ hyperthyroidism: a comparison of two thyrotropin receptor antibody immunoassays with thyroid scintigraphy and ultrasonography. Clin Endocrinol (Oxf). 2020; 92:169–78.
Article25. Viglietto G, Romano A, Manzo G, Chiappetta G, Paoletti I, Califano D, et al. Upregulation of the angiogenic factors PlGF, VEGF and their receptors (Flt-1, Flk-1/KDR) by TSH in cultured thyrocytes and in the thyroid gland of thiouracilfed rats suggest a TSH-dependent paracrine mechanism for goiter hypervascularization. Oncogene. 1997; 15:2687–98.
Article26. Sato K, Yamazaki K, Shizume K, Kanaji Y, Obara T, Ohsumi K, et al. Stimulation by thyroid-stimulating hormone and Grave’s immunoglobulin G of vascular endothelial growth factor mRNA expression in human thyroid follicles in vitro and flt mRNA expression in the rat thyroid in vivo. J Clin Invest. 1995; 96:1295–302.
Article27. Sato K. Vascular endothelial growth factors and thyroid disorders. Endocr J. 2001; 48:635–46.
Article28. Lytton SD, Kahaly GJ. Bioassays for TSH-receptor autoantibodies: an update. Autoimmun Rev. 2010; 10:116–22.
Article29. Kahaly GJ, Diana T, Kanitz M, Frommer L, Olivo PD. Prospective trial of functional thyrotropin receptor antibodies in Graves disease. J Clin Endocrinol Metab. 2020; 105:e1006–14.
Article30. Choi YM, Kwak MK, Hong SM, Hong EG. Changes in thyroid peroxidase and thyroglobulin antibodies might be associated with Graves’ disease relapse after antithyroid drug therapy. Endocrinol Metab (Seoul). 2019; 34:268–74.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Interferon-Alpha-Induced Destructive Thyroiditis Followed by Graves' Disease in a Patient with Chronic Hepatitis C: A Case Report
- Differential Diagnostic Value of Total T3/Free T4 Ratio in Graves' Disease and Painless Thyroiditis Presenting Thyrotoxicosis
- A Case of Painless Thyroiditis Followed by Graves' Disease
- The value of the mean peak systolic velocity of the superior thyroidal artery in the differential diagnosis of thyrotoxicosis
- A Case of Graves' Disease Following Subacute Thyroiditis Presented with Creeping