J Liver Cancer.
2022 Mar;22(1):63-68. 10.17998/jlc.2022.01.18.
Sorafenib combined with radiation therapy for advanced hepatocellular carcinoma with portal and hepatic vein invasion extending to the inferior vena cava: a complete response case according to modified RECIST criteria
- Affiliations
-
- 1Center for Liver and Pancreatobiliary Cancer, Goyang, Korea
- 2Graduate School of Cancer Science and Policy, Goyang, Korea
- 3Center for Proton Therapy, Goyang, Korea
- 4Department of Radiology, National Cancer Center, Goyang, Korea
- KMID: 2528298
- DOI: http://doi.org/10.17998/jlc.2022.01.18
Abstract
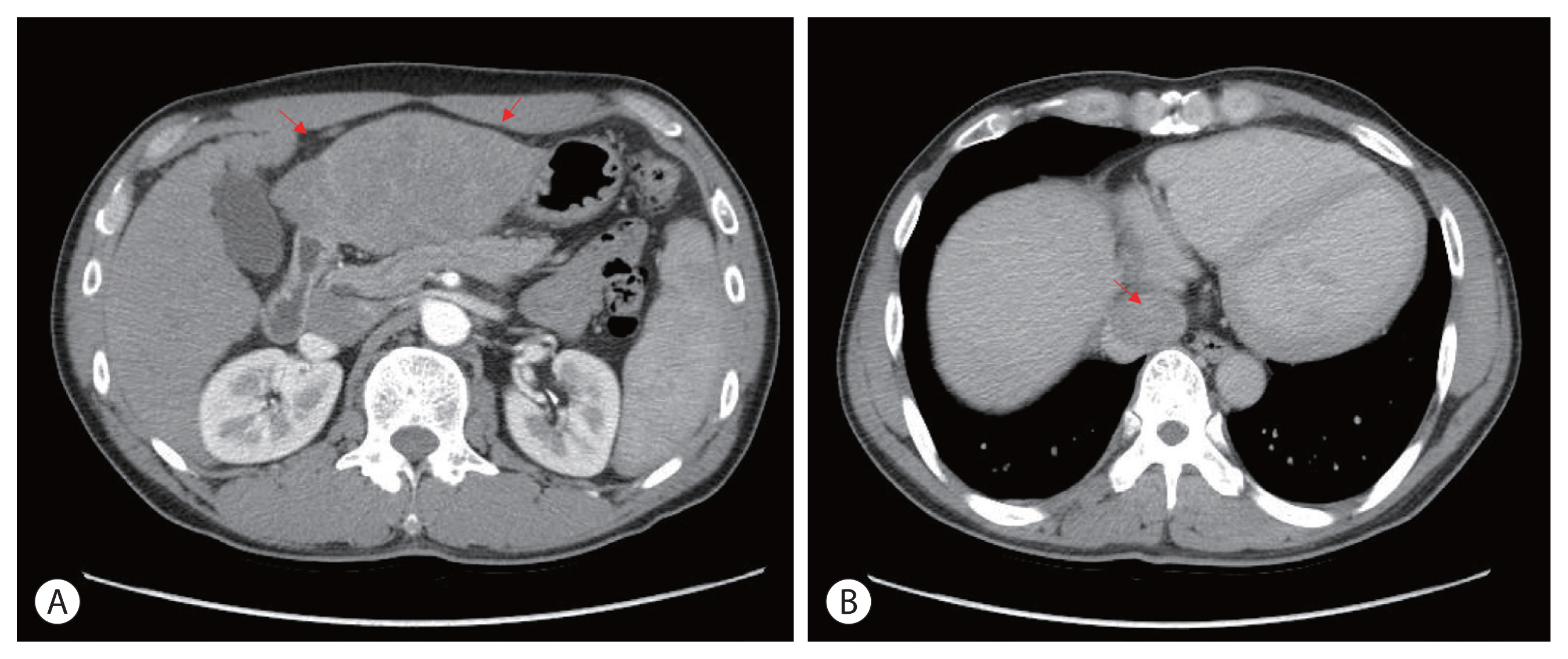
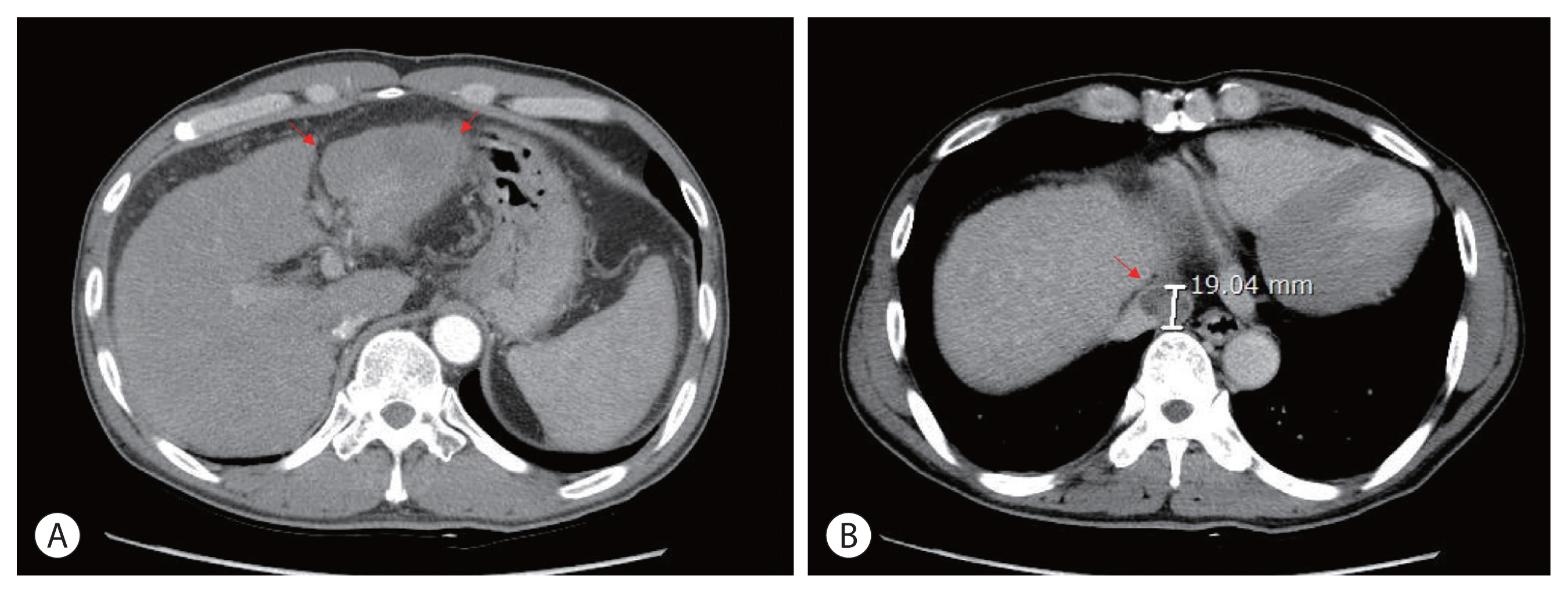
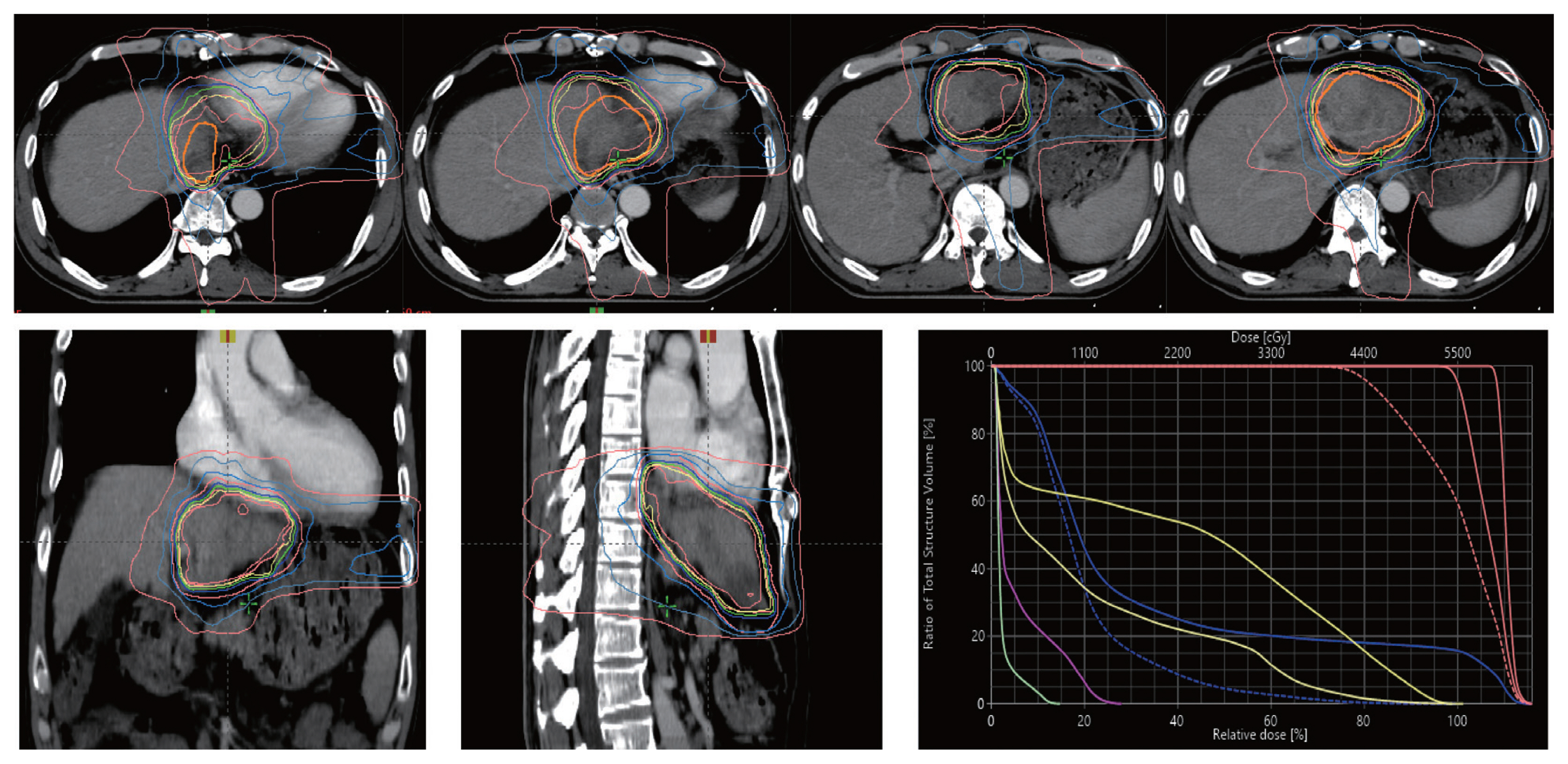
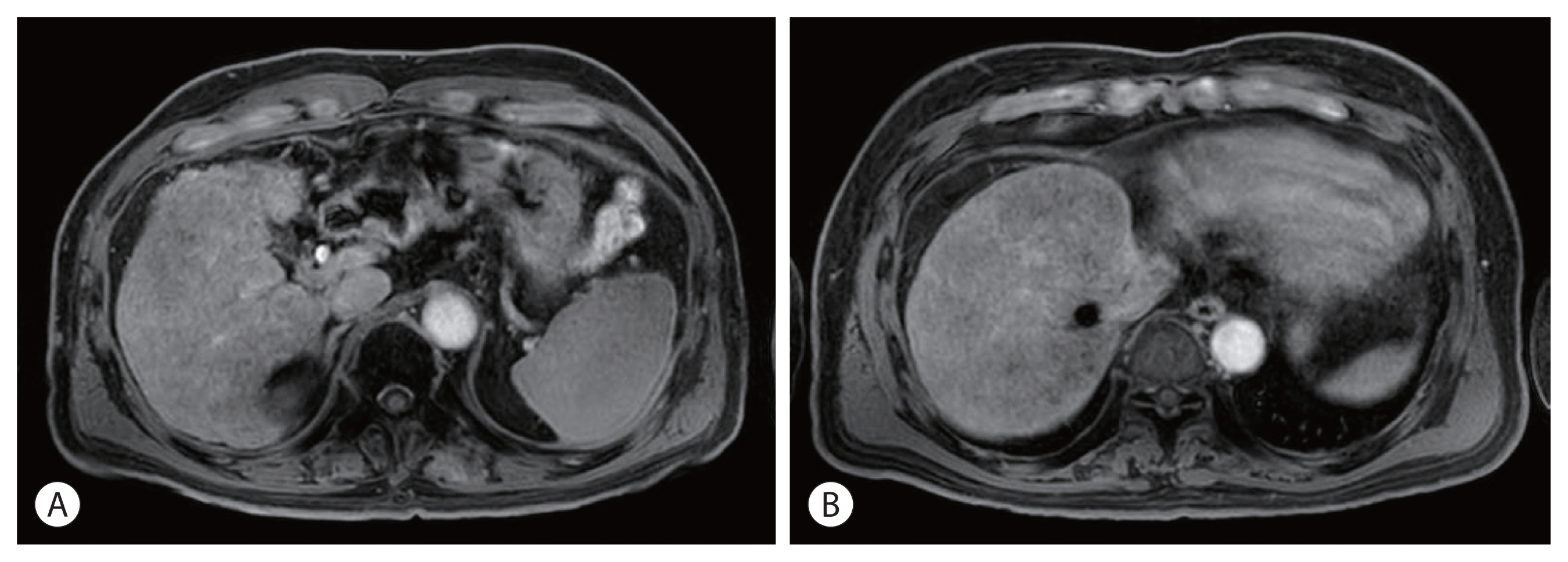
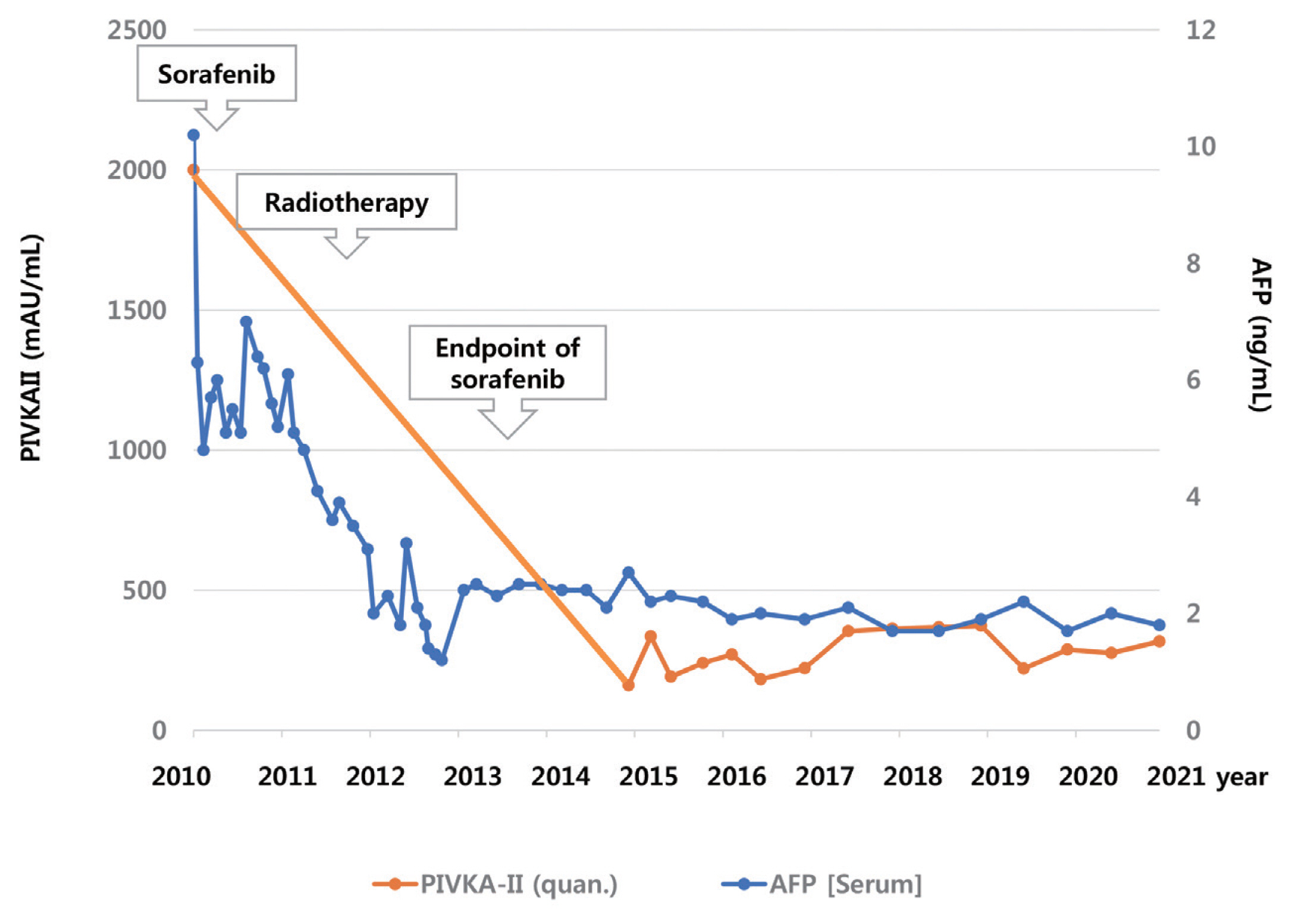
- The prognosis of patients with advanced hepatocellular carcinoma (HCC) with tumor thrombus extending to the inferior vena cava (IVC) is extremely poor. Herein, we present a rare case of advanced HCC that was treated with sorafenib and radiotherapy, leading to complete remission. This patient had a 9 cm infiltrative HCC occupying almost the entire left lobe with a tumor thrombus extending through the hepatic vein, IVC, and left portal vein. The patient received 400 mg sorafenib twice daily. One year after the start of sorafenib, intensity-modulated radiation therapy for viable HCC and tumor thrombus was performed with a dose of 5,500 cGy. Twenty-seven months after the starting date of sorafenib, there was no intratumoral arterial enhancement, which suggested a complete response according to the modified RECIST criteria. This case suggests that the combination of sorafenib and radiotherapy might provide clinical benefits in patients with advanced HCC with IVC tumor thrombus.
Figure
Cited by 1 articles
-
Is multidisciplinary treatment effective for hepatocellular carcinoma with portal vein tumor thrombus?
Won Hyeok Choe
J Liver Cancer. 2022;22(1):1-3. doi: 10.17998/jlc.2022.03.15.
Reference
-
References
1. Chun YH, Ahn SH, Park JY, Kim DY, Han KH, Chon CY, et al. Clinical characteristics and treatment outcomes of hepatocellular carcinoma with inferior vena cava/heart invasion. Anticancer Res. 2011; 31:4641–4646.2. Okada S. How to manage hepatic vein tumour thrombus in hepatocellular carcinoma. J Gastroenterol Hepatol. 2000; 15:346–348.
Article3. Korean Liver Cancer Association; National Cancer Center. 2018 Korean Liver Cancer Association-National Cancer Center Korea practice guidelines for the management of hepatocellular carcinoma. Gut Liver. 2019; 13:227–299.4. Wilhelm SM, Carter C, Tang L, Wilkie D, McNabola A, Rong H, et al. BAY 43-9006 exhibits broad spectrum oral antitumor activity and targets the RAF/MEK/ERK pathway and receptor tyrosine kinases involved in tumor progression and angiogenesis. Cancer Res. 2004; 64:7099–7109.
Article5. Chang YS, Adnane J, Trail PA, Levy J, Henderson A, Xue D, et al. Sorafenib (BAY 43-9006) inhibits tumor growth and vascularization and induces tumor apoptosis and hypoxia in RCC xenograft models. Cancer Chemother Pharmacol. 2007; 59:561–574.
Article6. Kim YJ, Jung J, Joo JH, Kim SY, Kim JH, Lim YS, et al. Combined transarterial chemoembolization and radiotherapy as a first-line treatment for hepatocellular carcinoma with macroscopic vascular invasion: necessity to subclassify Barcelona Clinic Liver Cancer stage C. Radiother Oncol. 2019; 141:95–100.
Article7. Rim CH, Kim CY, Yang DS, Yoon WS. External beam radiation therapy to hepatocellular carcinoma involving inferior vena cava and/or right atrium: a meta-analysis and systemic review. Radiother Oncol. 2018; 129:123–129.
Article8. Cha J, Seong J, Lee IJ, Kim JW, Han KH. Feasibility of sorafenib combined with local radiotherapy in advanced hepatocellular carcinoma. Yonsei Med J. 2013; 54:1178–1185.
Article9. Chen SW, Lin LC, Kuo YC, Liang JA, Kuo CC, Chiou JF. Phase 2 study of combined sorafenib and radiation therapy in patients with advanced hepatocellular carcinoma. Int J Radiat Oncol Biol Phys. 2014; 88:1041–1047.
Article10. Frankfurt O, Rosen ST. Mechanisms of glucocorticoid-induced apoptosis in hematologic malignancies: updates. Curr Opin Oncol. 2004; 16:553–563.
Article11. Wild AT, Gandhi N, Chettiar ST, Aziz K, Gajula RP, Williams RD, et al. Concurrent versus sequential sorafenib therapy in combination with radiation for hepatocellular carcinoma. PLoS One. 2013; 8:e65726.
Article12. Zhao JD, Liu J, Ren ZG, Gu K, Zhou ZH, Li WT, et al. Maintenance of Sorafenib following combined therapy of three-dimensional conformal radiation therapy/intensity-modulated radiation therapy and transcatheter arterial chemoembolization in patients with locally advanced hepatocellular carcinoma: a phase I/II study. Radiat Oncol. 2010; 5:12.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Advanced Hepatocellular Carcinoma with Portal Vein Tumor Invasion that Showed Favorable Prognosis after Combined External Radiation Therapy and Sorafenib Therapy
- A Case of Hepatocellular Carcinoma with Portal Vein Tumor Thrombosis Treated by Hepatic Artery Injection Chemotherapy and Radiotherapy
- A Case of Successful Hepatic Resection after Insufficient Response to Transarterial Chemoembolization and Radiation Therapy in Hepatocellular Carcinoma with Portal Vein Invasion
- Sorafenib Treatment in Advanced Hepatocellular Carcinoma with Tumor Thrombus Nearly Occupying the Entire Right Atrium
- Hepatocellular Carcinoma Extending to the Inferior Vena Cava and Right Atrium-A Case Report of 4 Years Survival after Repeated Transcatheter Arterial Chemoembolization Therapy -