J Liver Cancer.
2022 Mar;22(1):4-13. 10.17998/jlc.2022.01.16.
Radioembolization for hepatocellular carcinoma: what clinicians need to know
- Affiliations
-
- 1Department of Radiology, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2528291
- DOI: http://doi.org/10.17998/jlc.2022.01.16
Abstract
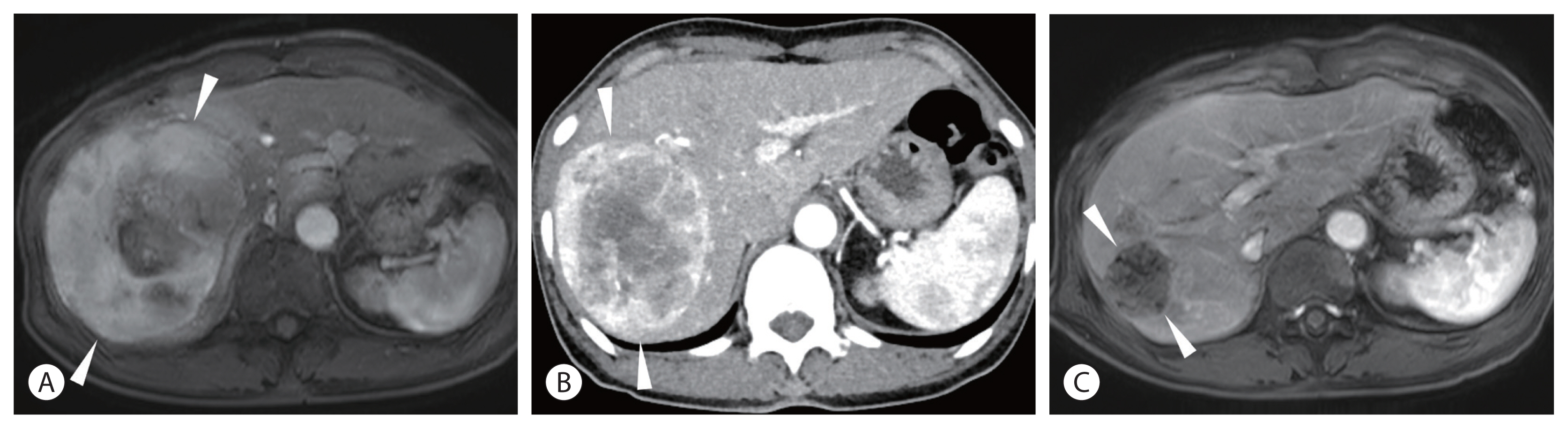
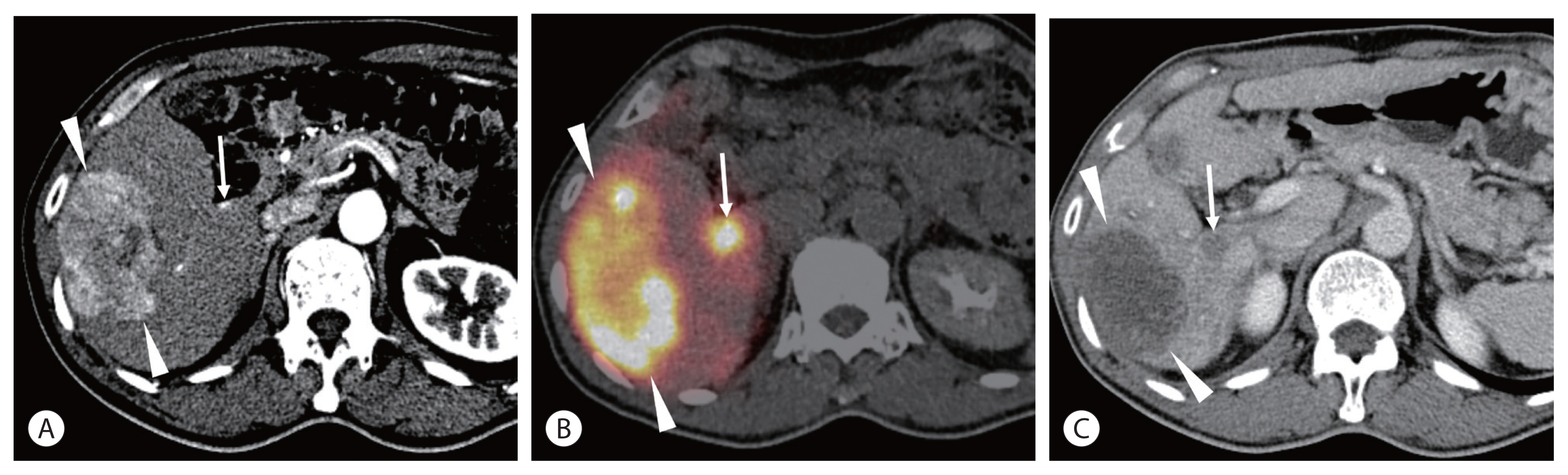
- Transarterial radioembolization (TARE) with yttrium 90 (90Y) has been used in the management of hepatocellular carcinoma (HCC) for more than 10 years in Korea. There are two types of 90Y radioactive microspheres available, namely, glass and resin microspheres, with comparable clinical outcomes. In general, TARE outperforms transarterial chemoembolization regarding post-embolization syndrome, time to progression, tumor downsizing for liver transplantation, and hospitalization stay. Although TARE is commonly recommended for patients with unresectable large HCCs, it can be an alternative to or performed in combination with ablation, surgical resection, and systemic treatment. This review aimed to address 90Y radioactive microspheres, patient selection, clinical outcomes, simulation tests, radioembolization procedures, follow-up imaging, and complications.
Keyword
Figure
Reference
-
References
1. Kim HC. Radioembolization for the treatment of hepatocellular carcinoma. Clin Mol Hepatol. 2017; 23:109–114.
Article2. Salem R, Lewandowski RJ, Kulik L, Wang E, Riaz A, Ryu RK, et al. Radioembolization results in longer time-to-progression and reduced toxicity compared with chemoembolization in patients with hepatocellular carcinoma. Gastroenterology. 2011; 140:497–507.
Article3. Salem R, Gilbertsen M, Butt Z, Memon K, Vouche M, Hickey R, et al. Increased quality of life among hepatocellular carcinoma patients treated with radioembolization, compared with chemoembolization. Clin Gastroenterol Hepatol. 2013; 11:1358–1365.
Article4. Kallini JR, Gabr A, Salem R, Lewandowski RJ. Transarterial radioembolization with yttrium-90 for the treatment of hepatocellular carcinoma. Adv Ther. 2016; 33:699–714.
Article5. Salem R, Lewandowski RJ, Sato KT, Atassi B, Ryu RK, Ibrahim S, et al. Technical aspects of radioembolization with 90Y microspheres. Tech Vasc Interv Radiol. 2007; 10:12–29.6. Salem R, Lewandowski RJ, Mulcahy MF, Riaz A, Ryu RK, Ibrahim S, et al. Radioembolization for hepatocellular carcinoma using yttrium-90 microspheres: a comprehensive report of long-term outcomes. Gastroenterology. 2010; 138:52–64.
Article7. Hilgard P, Hamami M, Fouly AE, Scherag A, Müller S, Ertle J, et al. Radioembolization with yttrium-90 glass microspheres in hepatocellular carcinoma: European experience on safety and long-term survival. Hepatology. 2010; 52:1741–1749.
Article8. Sangro B, Carpanese L, Cianni R, Golfieri R, Gasparini D, Ezziddin S, et al. Survival after yttrium-90 resin microsphere radioembolization of hepatocellular carcinoma across Barcelona clinic liver cancer stages: a European evaluation. Hepatology. 2011; 54:868–878.
Article9. Mazzaferro V, Sposito C, Bhoori S, Romito R, Chiesa C, Morosi C, et al. Yttrium-90 radioembolization for intermediate-advanced hepatocellular carcinoma: a phase 2 study. Hepatology. 2013; 57:1826–1837.
Article10. Thornton LM, Geller BS, Pepin EW, Shah JL, Kapp M, Toskich BB. Safety of radioembolization in the setting of angiographically apparent arterioportal shunting. J Vasc Interv Radiol. 2018; 29:1511–1518.
Article11. Lee EJ, Chung HW, Jo JH, So Y. Radioembolization for the treatment of primary and metastatic liver cancers. Nucl Med Mol Imaging. 2019; 53:367–373.
Article12. Vouche M, Lewandowski RJ, Atassi R, Memon K, Gates VL, Ryu RK, et al. Radiation lobectomy: time-dependent analysis of future liver remnant volume in unresectable liver cancer as a bridge to resection. J Hepatol. 2013; 59:1029–1036.
Article13. Padia SA, Johnson GE, Horton KJ, Ingraham CR, Kogut MJ, Kwan S, et al. Segmental yttrium-90 radioembolization versus segmental chemoembolization for localized hepatocellular carcinoma: results of a single-center, retrospective, propensity score-matched study. J Vasc Interv Radiol. 2017; 28:777–785.
Article14. Salem R, Johnson GE, Kim E, Riaz A, Bishay V, Boucher E, et al. Yttrium-90 radioembolization for the treatment of solitary, unresectable HCC: the legacy study. Hepatology. 2021; 74:2342–2352.
Article15. Salem R, Gordon AC, Mouli S, Hickey R, Kallini J, Gabr A, et al. Y90 radioembolization significantly prolongs time to progression compared with chemoembolization in patients with hepatocellular carcinoma. Gastroenterology. 2016; 151:1155–1163.
Article16. Gabr A, Kulik L, Mouli S, Riaz A, Ali R, Desai K, et al. Liver transplantation following yttrium-90 radioembolization: 15-year experience in 207-patient cohort. Hepatology. 2021; 73:998–1010.
Article17. Vilgrain V, Pereira H, Assenat E, Guiu B, Ilonca AD, Pageaux GP, et al. Efficacy and safety of selective internal radiotherapy with yttrium-90 resin microspheres compared with sorafenib in locally advanced and inoperable hepatocellular carcinoma (SARAH): an open-label randomised controlled phase 3 trial. Lancet Oncol. 2017; 18:1624–1636.18. Chow PKH, Gandhi M, Tan SB, Khin MW, Khasbazar A, Ong J, et al. SIRveNIB: selective internal radiation therapy versus sorafenib in asia-pacific patients with hepatocellular carcinoma. J Clin Oncol. 2018; 36:1913–1921.19. Ricke J, Klümpen HJ, Amthauer H, Bargellini I, Bartenstein P, de Toni EN, et al. Impact of combined selective internal radiation therapy and sorafenib on survival in advanced hepatocellular carcinoma. J Hepatol. 2019; 71:1164–1174.
Article20. Tai D, Loke K, Gogna A, Kaya NA, Tan SH, Hennedige T, et al. Radioembolisation with Y90-resin microspheres followed by nivolumab for advanced hepatocellular carcinoma (CA 209–678): a single arm, single centre, phase 2 trial. Lancet Gastroenterol Hepatol. 2021; 6:1025–1035.
Article21. Yoon SM, Ryoo BY, Lee SJ, Kim JH, Shin JH, An JH, et al. Efficacy and safety of transarterial chemoembolization plus external beam radiotherapy vs sorafenib in hepatocellular carcinoma with macroscopic vascular invasion: a randomized clinical trial. JAMA Oncol. 2018; 4:661–669.
Article22. Spreafico C, Sposito C, Vaiani M, Cascella T, Bhoori S, Morosi C, et al. Development of a prognostic score to predict response to yttrium-90 radioembolization for hepatocellular carcinoma with portal vein invasion. J Hepatol. 2018; 68:724–732.
Article23. Abouchaleh N, Gabr A, Ali R, Al Asadi A, Mora RA, Kallini JR, et al. 90Y radioembolization for locally advanced hepatocellular carcinoma with portal vein thrombosis: long-term outcomes in a 185-patient cohort. J Nucl Med. 2018; 59:1042–1048.
Article24. Hamoui N, Minocha J, Memon K, Sato K, Ryu R, Salem R, et al. Prophylactic embolization of the gastroduodenal and right gastric arteries is not routinely necessary before radioembolization with glass microspheres. J Vasc Interv Radiol. 2013; 24:1743–1745.
Article25. Gabr A, Ranganathan S, Mouli SK, Riaz A, Gates VL, Kulik L, et al. Streamlining radioembolization in UNOS T1/T2 hepatocellular carcinoma by eliminating lung shunt estimation. J Hepatol. 2020; 72:1151–1158.
Article26. Wright CL, Werner JD, Tran JM, Gates VL, Rikabi AA, Shah MH, et al. Radiation pneumonitis following yttrium-90 radioembolization: case report and literature review. J Vasc Interv Radiol. 2012; 23:669–674.
Article27. Salem R, Thurston KG. Radioembolization with 90Yttrium microspheres: a state-of-the-art brachytherapy treatment for primary and secondary liver malignancies. Part 1: technical and methodologic considerations. J Vasc Interv Radiol. 2006; 17:1251–1278.
Article28. Garin E, Tselikas L, Guiu B, Chalaye J, Edeline J, de Baere T, et al. Personalised versus standard dosimetry approach of selective internal radiation therapy in patients with locally advanced hepatocellular carcinoma (DOSISPHERE-01): a randomised, multicentre, open-label phase 2 trial. Lancet Gastroenterol Hepatol. 2021; 6:17–29.
Article29. Kim HC, Choi JW, Lee M, Kim YJ, Paeng JC, Chung JW. Lung shunt reduction for yttrium-90 radioembolization: chemoembolization versus radioembolization. In Vivo. 2021; 35:2305–2312.
Article30. Tafti BA, Padia SA. Dosimetry of Y-90 microspheres utilizing Tc-99 m SPECT and Y-90 PET. Semin Nucl Med. 2019; 49:211–217.31. McCann JW, Larkin AM, Martino LJ, Eschelman DJ, Gonsalves CF, Brown DB. Radiation emission from patients treated with selective hepatic radioembolization using yttrium-90 microspheres: are contact restrictions necessary? J Vasc Interv Radiol. 2012; 23:661–667.
Article32. Joo I, Kim HC, Kim GM, Paeng JC. Imaging evaluation following 90Y radioembolization of liver tumors: what radiologists should know. Korean J Radiol. 2018; 19:209–222.
Article33. Kim HC, Kim YJ, Lee JH, Suh KS, Chung JW. Feasibility of boosted radioembolization for hepatocellular carcinoma larger than 5 cm. J Vasc Interv Radiol. 2019; 30:1–8.
Article34. Kim HC, Joo I, Lee M, Chung JW. Benign biliary stricture after yttrium-90 radioembolization for hepatocellular carcinoma. J Vasc Interv Radiol. 2020; 31:2014–2021.
Article35. Yim SY, Kim JD, Jung JY, Kim CH, Seo YS, Yim HJ, et al. Gastrectomy for the treatment of refractory gastric ulceration after radioembolization with 90Y microspheres. Clin Mol Hepatol. 2014; 20:300–305.
Article36. Kim HC, Kim YJ, Paeng JC, Chung JW. Yttrium-90 radioembolization of the right inferior phrenic artery in 20 patients with hepatocellular carcinoma. J Vasc Interv Radiol. 2018; 29:556–563.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Role of Yttrium-90 Radioembolization in the Management of Hepatocellular Carcinoma
- Radioembolization for the treatment of hepatocellular carcinoma
- Treatments Other than Sorafenib for Patients with Advanced Hepatocellular Carcinoma
- Complications Related to Transarterial Treatment of Hepatocellular Carcinoma: A Comprehensive Review
- Concurrent transarterial radioembolization and combination atezolizumab/ bevacizumab treatment of infiltrative hepatocellular carcinoma with portal vein tumor thrombosis: a case report