Cancer Res Treat.
2022 Apr;54(2):406-416. 10.4143/crt.2021.441.
Radiotherapy versus Surgery in Early-Stage HPV-Positive Oropharyngeal Cancer
- Affiliations
-
- 1Department of Radiation Oncology, Seoul National University Hospital, Seoul, Korea
- 2Department of Otorhinolaryngology-Head and Neck Surgery, Seoul National University Hospital, Seoul, Korea
- 3Department of Radiation Oncology, Seoul National University Bundang Hospital, Seongnam, Korea
- 4Department of Otorhinolaryngology-Head and Neck Surgery, Seoul National University Bundang Hospital, Seongnam, Korea
- 5Department of Otorhinolaryngology-Head and Neck Surgery, SMG-SNU Boramae Medical Center, Seoul, Korea
- 6Department of Radiation Oncology, SMG-SNU Boramae Medical Center, Seoul, Korea
- KMID: 2528210
- DOI: http://doi.org/10.4143/crt.2021.441
Abstract
- Purpose
This study aimed to compare the outcomes of primary radiotherapy (RT) versus surgery in early-stage human papilloma virus–positive oropharyngeal squamous cell carcinoma (hpv+OPC), and investigate the preoperative clinical factors that can predict the requirement for postoperative adjuvant treatment.
Materials and Methods
This multicenter study included 166 patients with American Joint Committee on Cancer 8th edition-Stages I-II hpv+OPC. Sixty (36.1%) and 106 (63.9%) patients underwent primary (concurrent chemo)radiotherapy [(CC)RT] and surgery, respectively. Seventy-eight patients (73.6%) in the surgery group received postoperative (CC)RT.
Results
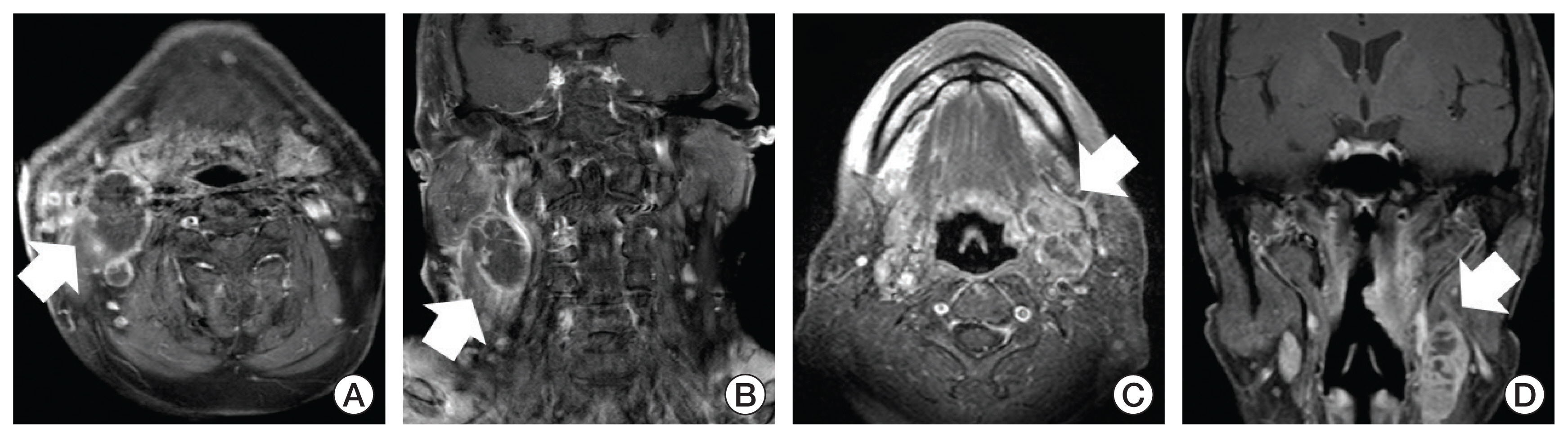
With a median follow-up of 45.6 months for survivors, the 2-year overall survival (OS), progression-free survival (PFS), and locoregional control (LC) for RT/surgery were 97.8%/96.4%, 91.1%/92.0%, and 92.9%/93.3%, respectively. In multivariate analyses, patients with synchronous radiologic extranodal extension and conglomeration (ENEcong) of metastatic lymph nodes (LNs) showed significantly poorer OS (p=0.047), PFS (p=0.001), and LC (p=0.003). In patients undergoing primary surgery, two or more clinically positive LN metastases (odds ratio [OR], 5.15; p=0.004) and LN metastases with ENEcong (OR, 3.75; p=0.009) were predictors of postoperative chemoradiotherapy. No patient in the primary RT group demonstrated late severe toxicity whereas three (2.8%), one (0.9%), and one (0.9%) patient in the surgery group showed grade 3 dysphagia, grade 3 xerostomia, and fatal oral cavity bleeding.
Conclusion
We found no differences in OS, PFS, and LC between upfront RT and surgery in stage I-II hpv+OPC which warrants comparison through a prospective trial in the treatment de-escalation era. However, most early-stage hpv+OPC patients undergoing surgery received adjuvant (CC)RT. Pretreatment LN findings were prognostic and predictive for adjuvant treatment.
Figure
Reference
-
References
1. Baskin RM, Boyce BJ, Amdur R, Mendenhall WM, Hitchcock K, Silver N, et al. Transoral robotic surgery for oropharyngeal cancer: patient selection and special considerations. Cancer Manag Res. 2018; 10:839–46.2. Morisod B, Simon C. Meta-analysis on survival of patients treated with transoral surgery versus radiotherapy for early-stage squamous cell carcinoma of the oropharynx. Head Neck. 2016; 38(Suppl 1):E2143–50.
Article3. Yamashita Y, Ikegami T, Hirakawa H, Uehara T, Deng Z, Agena S, et al. Staging and prognosis of oropharyngeal carcinoma according to the 8th edition of the American Joint Committee on Cancer Staging Manual in human papillomavirus infection. Eur Arch Otorhinolaryngol. 2019; 276:827–36.
Article4. Ang KK, Harris J, Wheeler R, Weber R, Rosenthal DI, Nguyen-Tan PF, et al. Human papillomavirus and survival of patients with oropharyngeal cancer. N Engl J Med. 2010; 363:24–35.
Article5. Zanoni DK, Patel SG, Shah JP. Changes in the 8th edition of the American Joint Committee on Cancer (AJCC) staging of head and neck cancer: rationale and implications. Curr Oncol Rep. 2019; 21:52.
Article6. You EL, Henry M, Zeitouni AG. Human papillomavirus-associated oropharyngeal cancer: review of current evidence and management. Curr Oncol. 2019; 26:119–23.
Article7. Gillison ML, Trotti AM, Harris J, Eisbruch A, Harari PM, Adelstein DJ, et al. Radiotherapy plus cetuximab or cisplatin in human papillomavirus-positive oropharyngeal cancer (NRG Oncology RTOG 1016): a randomised, multicentre, non-inferiority trial. Lancet. 2019; 393:40–50.8. Fundakowski CE, Lango M. Considerations in surgical versus non-surgical management of HPV positive oropharyngeal cancer. Cancers Head Neck. 2016; 1:6.
Article9. Nichols AC, Theurer J, Prisman E, Read N, Berthelet E, Tran E, et al. Radiotherapy versus transoral robotic surgery and neck dissection for oropharyngeal squamous cell carcinoma (ORATOR): an open-label, phase 2, randomised trial. Lancet Oncol. 2019; 20:1349–59.
Article10. Mirghani H, Blanchard P. Treatment de-escalation for HPV-driven oropharyngeal cancer: where do we stand? Clin Transl Radiat Oncol. 2018; 8:4–11.
Article11. National Comprehensive Cancer Network. Head and neck cancers (version 1, 2021) [Internet]. Plymouth Meeting, PA: National Comprehensive Cancer Network;2021. [cited 2021 Jan 10]. Available from: https://www.nccn.org/professionals/physician_gls/pdf/head-and-neck.pdf .12. Cooper JS, Zhang Q, Pajak TF, Forastiere AA, Jacobs J, Saxman SB, et al. Long-term follow-up of the RTOG 9501/intergroup phase III trial: postoperative concurrent radiation therapy and chemotherapy in high-risk squamous cell carcinoma of the head and neck. Int J Radiat Oncol Biol Phys. 2012; 84:1198–205.13. Geiger JL, Ku JA. Postoperative treatment of oropharyngeal cancer in the era of human papillomavirus. Curr Treat Options Oncol. 2019; 20:20.
Article14. Mehanna H, Robinson M, Hartley A, Kong A, Foran B, Fulton-Lieuw T, et al. Radiotherapy plus cisplatin or cetuximab in low-risk human papillomavirus-positive oropharyngeal cancer (De-ESCALaTE HPV): an open-label randomised controlled phase 3 trial. Lancet. 2019; 393:51–60.15. Peng H, Chen L, Tang LL, Li WF, Mao YP, Guo R, et al. Significant value of (18)F-FDG-PET/CT in diagnosing small cervical lymph node metastases in patients with nasopharyngeal carcinoma treated with intensity-modulated radiotherapy. Chin J Cancer. 2017; 36:95.
Article16. Biau J, Lapeyre M, Troussier I, Budach W, Giralt J, Grau C, et al. Selection of lymph node target volumes for definitive head and neck radiation therapy: a 2019 update. Radiother Oncol. 2019; 134:1–9.
Article17. Billfalk-Kelly A, Yu E, Su J, O’Sullivan B, Waldron J, Ringash J, et al. Radiologic extranodal extension portends worse outcome in cN+ TNM-8 stage I human papillomavirus-mediated oropharyngeal cancer. Int J Radiat Oncol Biol Phys. 2019; 104:1017–27.
Article18. Freitag J, Wald T, Kuhnt T, Gradistanac T, Kolb M, Dietz A, et al. Extracapsular extension of neck nodes and absence of human papillomavirus 16-DNA are predictors of impaired survival in p16-positive oropharyngeal squamous cell carcinoma. Cancer. 2020; 126:1856–72.
Article19. Huang SH, O’Sullivan B, Su J, Bartlett E, Kim J, Waldron JN, et al. Prognostic importance of radiologic extranodal extension in HPV-positive oropharyngeal carcinoma and its potential role in refining TNM-8 cN-classification. Radiother Oncol. 2020; 144:13–22.
Article20. Lee HN, Han JK, Kim HH, Shin HC, Kim IY, Jou SS. Comparative study of lymph node metastasis from squamous cell carcinoma and non-squamous cell carcinoma on neck CT. J Korean Soc Radiol. 2015; 72:271–81.
Article21. Spector ME, Chinn SB, Bellile E, Gallagher KK, Ibrahim M, Vainshtein J, et al. Matted nodes as a predictor of distant metastasis in advanced–stage III/IV oropharyngeal squamous cell carcinoma. Head Neck. 2016; 38:184–90.
Article22. Stelmes JJ, Gregoire V, Poorten VV, Golusinski W, Szewczyk M, Jones T, et al. Organ preservation and late functional outcome in oropharyngeal carcinoma: rationale of EORTC 1420, the “Best of” trial. Front Oncol. 2019; 9:999.
Article23. Nichols AC, Lang P, Prisman E, Berthelet E, Tran E, Hamilton S, et al. Treatment de-escalation for HPV-associated oropharyngeal squamous cell carcinoma with radiotherapy vs. trans-oral surgery (ORATOR2): study protocol for a randomized phase II trial. BMC Cancer. 2020; 20:125.
Article24. Yom SS, Torres-Saavedra P, Caudell JJ, Waldron JN, Gillison ML, Xia P, et al. Reduced-dose radiation therapy for HPV-associated oropharyngeal carcinoma (NRG Oncology HN-002). J Clin Oncol. 2021; 39:956–65.
Article25. Haughey BH, Hinni ML, Salassa JR, Hayden RE, Grant DG, Rich JT, et al. Transoral laser microsurgery as primary treatment for advanced-stage oropharyngeal cancer: a United States multicenter study. Head Neck. 2011; 33:1683–94.
Article26. Leonhardt FD, Quon H, Abrahao M, O’Malley BW Jr, Weinstein GS. Transoral robotic surgery for oropharyngeal carcinoma and its impact on patient-reported quality of life and function. Head Neck. 2012; 34:146–54.
Article27. Langendijk JA, Slotman BJ, van der Waal I, Doornaert P, Berkof J, Leemans CR. Risk-group definition by recursive partitioning analysis of patients with squamous cell head and neck carcinoma treated with surgery and postoperative radiotherapy. Cancer. 2005; 104:1408–17.
Article28. Baliga S, Klamer B, Jhawar S, Gamez M, Mitchell D, Blakaj A, et al. Identification of clinical and socioeconomic predictors of adjuvant therapy after trans-oral robotic surgery in patients with oropharyngeal squamous cell carcinoma. Cancers (Basel). 2020; 12:2474.
Article29. Lee B, Choi YJ, Kim SO, Lee YS, Hong JY, Baek JH, et al. Prognostic value of radiologic extranodal extension in human papillomavirus-related oropharyngeal squamous cell carcinoma. Korean J Radiol. 2019; 20:1266–74.
Article30. Ozmen OA, Alpay M, Saraydaroglu O, Demir UL, Kasapoglu F, Coskun HH, et al. Prognostic significance of soft tissue deposits in laryngeal carcinoma. Braz J Otorhinolaryngol. 2018; 84:566–73.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- De-escalated Therapy for HPV Positive Oropharyngeal Cancer
- Clinical Benefit of Vaccinating Male Against HPV-related Disease
- Human Papillomavirus in Head and Neck Cancer: Several Questions
- Human Papilloma Virus Positive Oropharyngeal Cancer
- Human papillomavirus: footprints in the population of western India