Clinical practice guidelines for optimizing bone health in Korean children and adolescents
- Affiliations
-
- 1Department of Pediatrics, Seoul National University Children's Hospital, Seoul National University College of Medicine, Seoul, Korea
- 2Department of Pediatrics, Severance Children’s Hospital, Endocrine Research Institute, Yonsei University College of Medicine, Seoul, Korea
- 3Department of Pediatrics, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea
- 4Department of Pediatrics, Korea University College of Medicine, Seoul, Korea
- 5Department of Pediatrics, Dong-A University Hospital, Busan, Korea
- 6Department of Pediatrics, Korea Cancer Center Hospital, Seoul, Korea
- 7Department of Pediatrics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 8Department of Pediatrics, St. Vincent’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 9Department of Pediatrics, Kyung Hee University Hospital at Gangdong, Kyung Hee University College of Medicine, Seoul, Korea
- KMID: 2528192
- DOI: http://doi.org/10.6065/apem.2244060.030
Abstract
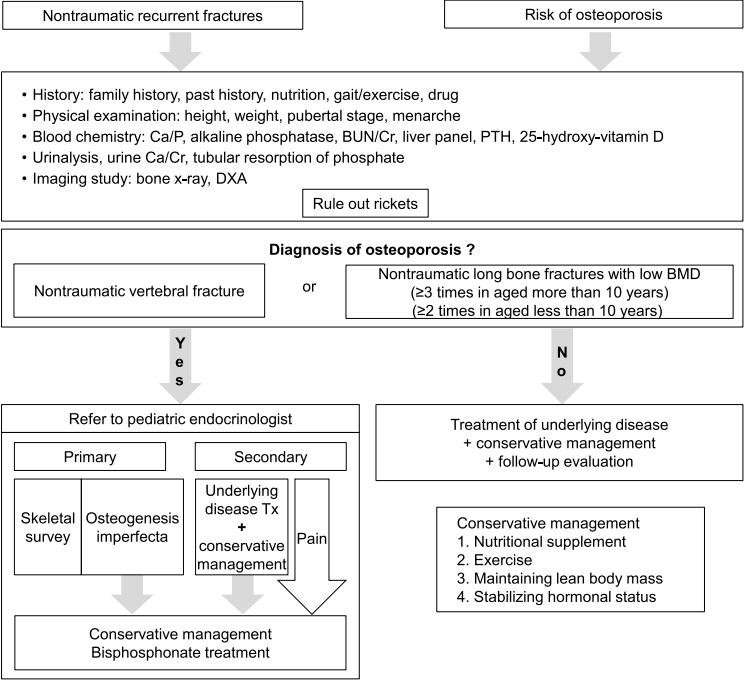
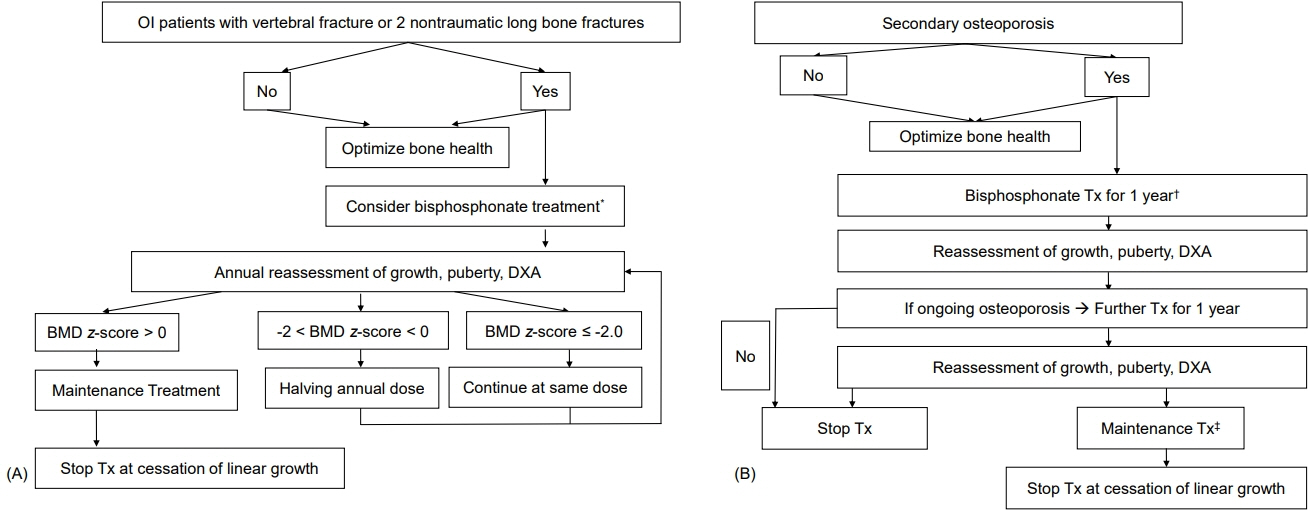
- The Committee on Pediatric Bone Health of the Korean Society of Pediatric Endocrinology has newly developed evidence-based clinical practice guidelines for optimizing bone health in Korean children and adolescents. These guidelines present recommendations based on the Grading of Recommendations, which includes the quality of evidence. In the absence of sufficient evidence, conclusions were based on expert opinion. These guidelines include processes of bone acquisition, definition, and evaluation of low bone mineral density (BMD), causes of osteoporosis, methods for optimizing bone health, and pharmacological treatments for enhancing BMD in children and adolescents. While these guidelines provide current evidence-based recommendations, further research is required to strengthen these guidelines.
Keyword
Figure
Cited by 4 articles
-
Factors affecting bone mineral density in children and adolescents with systemic lupus erythematosus
Su Jin Park, Soo Yeun Sim, Dae Chul Jeong, Byung-Kyu Suh, Moon Bae Ahn
Ann Pediatr Endocrinol Metab. 2024;29(3):191-200. doi: 10.6065/apem.2346060.030.Magnesium as an adjunct to nimodipine in subarachnoid hemorrhage: a meta-analysis
Sukjin Hong, Riva Satya Radiansyah, Yuri Pamungkas, Ilham Ikhtiar
J Yeungnam Med Sci. 2025;42:26. doi: 10.12701/jyms.2025.42.26.Commentary on "Pediatric and adult osteoporosis: a contrasting mirror"
Yoon-Sok Chung
Ann Pediatr Endocrinol Metab. 2025;30(1):55-56. doi: 10.6065/apem.2448244.122.Essential micronutrients in children and adolescents with a focus on growth and development: a narrative review
Sukjin Hong
J Yeungnam Med Sci. 2025;42:25. doi: 10.12701/jyms.2025.42.25.
Reference
-
References
1. Ma NS, Gordon CM. Pediatric osteoporosis: where are we now? J Pediatr. 2012; 161:983–90.2. Heaney RP, Abrams S, Dawson-Hughes B, Looker A, Marcus R, Matkovic V, et al. Peak bone mass. Osteoporos Int. 2000; 11:985–1009.3. American Academy of Pediatrics Steering Committee on Quality Improvement and Management. Classifying recommendations for clinical practice guidelines. Pediatrics. 2004; 114:874–7.4. Boot AM, de Ridder MA, van der Sluis IM, van Slobbe I, Krenning EP, Keizer-Schrama SM. Peak bone mineral density, lean body mass and fractures. Bone. 2010; 46:336–41.5. Berger C, Goltzman D, Langsetmo L, Joseph L, Jackson S, Kreiger N, et al. Peak bone mass from longitudinal data: implications for the prevalence, pathophysiology, and diagnosis of osteoporosis. J Bone Miner Res. 2010; 25:1948–57.6. Lim JS, Hwang JS, Lee JA, Kim DH, Park KD, Cheon GJ, et al. Bone mineral density according to age, bone age, and pubertal stages in Korean children and adolescents. J Clin Densitom. 2010; 13:68–76.7. Yi KH, Hwang JS, Kim EY, Lee JA, Kim DH, Lim JS. Reference values for bone mineral density according to age with body size adjustment in Korean children and adolescents. J Bone Miner Metab. 2014; 32:281–9.8. Golden NH, Abrams SA; Committee on Nutrition. Optimizing bone health in children and adolescents. Pediatrics. 2014; 134:e1229–43.9. Bishop N, Arundel P, Clark E, Dimitri P, Farr J, Jones G, et al. Fracture prediction and the definition of osteoporosis in children and adolescents: the ISCD 2013 Pediatric Official Positions. J Clin Densitom. 2014; 17:275–80.10. Root AW, Levine MA. Disorders of mineral metabolism II. Abnormalities of mineral homeostasis in the newborn, infant, child and adolescent. In : Sperling MA, editor. Pediatric endocrinology. 5th ed. Philadelphia (PA): Elsevier;2021. p. 705–813.11. De Paula F, Black DM, Rosen CJ. Osteoporosis: basic and clinical aspects. In : Melmed S, Auchus RJ, Goldfine AB, Koennig RJ, Rosen CJ, editors. William's textbook of endocrinology. 14th ed. Philadelphia (PA): Elsevier;2020. p. 1256–97.12. Imerci A, Canbek U, Haghari S, Surer L, Kocak M. Idiopathic juvenile osteoporosis: a case report and review of the literature. Int J Surg Case Rep. 2015; 9:127–9.13. Drake MT, Khosla S. Role of sex steroids in the pathogenesis of osteoporosis. Rosen CJ. Primer on the metabolic bone diseases and disorders of mineral metabolism. 7th ed. Washington DC: The American Society of Bone and Mineral Metabolism;2008. p. 208–13.14. Tritos NA, Klibanski A. Effects of growth hormome on bone. Prog Mol Biol Transl Sci. 2016; 138:193–211.15. Giustina A, Mazziotti G, Ganalis E. Growth hormone, insulin-like growth factors, and the skeleton. Endocr Rev. 2008; 29:535–59.16. Bassett JH. Williams GR. Role of thyroid hormones in skeletal development and bone maintenance. Endocr Rev. 2016; 37:135–87.17. Sundaraghavan V, Mazur MM, Evans B, Liu J, Ebraheim NA. Diabetes and bone health: latest evidence and clinical implications. Ther Adv Musculoskelet Dis. 2017; 9:67–74.18. Castrogiovanni P, Trovato FM, Szychlinska MA, Nsir H, Imbesi R, Musumeci G. The importance of physical activity in osteoporosis. From the molecular pathways to the clinical evidence. Histol Histopathol. 2016; 31:1183–94.19. Grover M, Bachrach LK. Osteoporosis in children with chronic illness. Diagnosis, monitoring, and treatment. Curr Osteoporos Rep. 2017; 15:271–82.20. Compston J. Glucocorticoid-induced osteoporosis: an update. Endocrine. 2018; 61:7–16.21. Henderson RC, Berglund LM, May R, Zemel BS, Grossberg RI, Johnson J, et al. The relationship between fractures and DXA measures of BMD in the distal femur of children and adolescents with cerebral palsy or muscular dystrophy. J Bone Miner Res. 2010; 25:520–6.22. Fehlings D, Switzer L, Agarwal P, Wong C, Sochett E, Stevenson R, et al. Informing evidence-based clinical practice guidelines for children with cerebral palsy at risk of osteoporosis: a systematic review. Dev Med Child Neurol. 2012; 54:106–16.23. Hough JP, Boyd RN, Keating JL. Systematic review of interventions for low bone mineral density in children with cerebral palsy. Pediatrics. 2010; 125:e670–8.24. Iwasaki T, Nonoda Y, Ishii M. Long-term outcomes of children and adolescents who had cerebral palsy with secondary osteoporosis. Curr Med Res Opin. 2012; 28:737–47.25. Rodd C, Lang B, Ramsay T, Alos N, Huber AM, Cabral DA, et al. Incident vertebral fractures among children with rheumatic disorders 12 months after glucocorticoid initiation: a national observational study. Arthritis Care Res (Hoboken). 2012; 64:122–31.26. Vierucci F, Saggese G, Cimaz R. Osteoporosis in childhood. Curr Opin Rheumatol. 2017; 29:535–46.27. Schmidt S, Mellstrom D, Norjavaara E, Sundh SV, Saalman R. Low bone mineral density in children and adolescents with inflammatory bowel disease: a population-based study from Western Sweden. Inflamm Bowel Dis. 2009; 15:1844–50.28. El-Matary W, Sikora S, Spady D. Bone mineral density, vitamin D, and disease activity in children newly diagnosed with inflammatory bowel disease. Dig Dis Sci. 2011; 56:825–9.29. Pappa H, Thayu M, Sylvester F, Leonard M, Zemel B, Gordon C. Skeletal health of children and adolescents with inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 2011; 53:11–25.30. Hogler W, Wehl G, van Staa T, Meister B, Klein-Franke A, Kropshofer G. Incidence of skeletal complications during treatment of childhood acute lymphoblastic leukemia: comparison of fracture risk with the General Practice Research Database. Pediatr Blood Cancer. 2007; 48:21–7.31. Alos N, Grant RM, Ramsay T, Halton J, Cummings EA, Miettunen PM, et al. High incidence of vertebral fractures in children with acute lymphoblastic leukemia 12 months after the initiation of therapy. J Clin Oncol. 2012; 30:2760–7.32. Lalayiannis AD, Crabtree NJ, Fewtrell M, Biassoni L, Milford DV, Ferro CJ, et al. Assessing bone mineralisation in children with chronic kidney disease: what clinical and research tools are available? Pediatr Nephrol. 2020; 35:937–57.33. Helenius I, Remes V, Salminen S, Valta H, Makitie O, Holmberg C, et al. Incidence and predictors of fractures in children after solid organ transplantation: a 5-year prospective, population-based study. J Bone Miner Res. 2006; 21:380–7.34. Johnston CC Jr, Miller JZ, Slemenda CW, Reister TK, Hui S, Christian JC, et al. Calcium supplementation and increases in bone mineral density in children. N Engl J Med. 1992; 327:82–7.35. Lloyd T, Andon MB, Rollings N, Martel JK, Landis JR, Demers LM, et al. Calcium supplementation and bone mineral density in adolescent girls. JAMA. 1993; 270:841–4.36. Winzenberg TM, Powell S, Shaw KA, Jones G. Vitamin D supplementation for improving bone mineral density in children. Cochrane Database Syst Rev. 2010; (10):CD006944.37. Greene DA, Naughton GA. Calcium and vitamin-D supplementation on bone structural properties in peripubertal female identical twins: a randomised controlled trial. Osteoporos Int. 2011; 22:489–98.38. The Korean Nutrition Society. 2020 Dietary reference intakes for Koreans: application [Internet]. Seoul (Korea): The Korean Nutrition Society;[cited 2022 Feb 1]. Available from: http://www.kns.or.kr.39. Rosen CJ, Abrams SA, Aloia JF, Brannon PM, Clinton SK, Durazo-Arvizu RA, et al. IOM committee members respond to Endocrine Society vitamin D guideline. J Clin Endocrinol Metab. 2012; 97:1146–52.40. Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, et al. Evaluation, treatment, and prevention of vitamin D deficiency: Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011; 96:1911–30.41. Committee on Nutrition and the Council on Sports Medicine and Fitness. Sports drinks and energy drinks for children and adolescents: are they appropriate? Pediatrics. 2011; 127:1182–9.42. Hind K, Burrows M. Weight-bearing exercise and bone mineral accrual in children and adolescents: a review of controlled trials. Bone. 2007; 40:14–27.43. McKay HA, Petit MA, Schutz RW, Prior JC, Barr SI, Khan KM. Augmented trochanteric bone mineral density after modified physical education classes: a randomized school-based exercise intervention study in prepubescent and early pubescent children. J Pediatr. 2000; 136:156–62.44. MacKelvie KJ, Khan KM, Petit MA, Janssen PA, McKay HA. A school-based exercise intervention elicits substantial bone health benefits: a 2-year randomized controlled trial in girls. Pediatrics. 2003; 112:e447.45. Petit MA, McKay HA, MacKelvie KJ, Heinonen A, Khan KM, Beck TJ. A randomized school-based jumping intervention confers site and maturity-specific benefits on bone structural properties in girls: a hip structural analysis study. J Bone Miner Res. 2002; 17:363–72.46. Specker B, Thiex NW, Sudhagoni RG. Does exercise influence pediatric bone? A systematic review. Clin Orthop Relat Res. 2015; 473:3658–72.47. Field AE, Gordon CM, Pierce LM, Ramappa A, Kocher MS. Prospective study of physical activity and risk of developing a stress fracture among preadolescent and adolescent girls. Arch Pediatr Adolesc Med. 2011; 165:723–8.48. Hohman EE, Balantekin KN, Birch LL, Savage JS. Dieting is associated with reduced bone mineral accrual in a longitudinal cohort of girls. BMC Public Health. 2018; 18:1285.49. Baroncelli GI, Bertelloni S. The use of bisphosphonates in pediatrics. Horm Res Paediatr. 2014; 82:290–302.50. Dwan K, Phillipi CA, Steiner RD, Basel D. Bisphosphonate therapy for osteogenesis imperfecta. Cochrane Database Syst Rev. 2016; 10:CD005088.51. Alcausin MB, Briody J, Pacey V, Ault J, McQuade M, Bridge C, et al. Intravenous pamidronate treatment in children with moderate-to-severe osteogenesis imperfecta started under three years of age. Horm Res Paediatr. 2013; 79:333–40.52. Baroncelli GI, Vierucci F, Bertelloni S, Erba P, Zampollo E, Giuca MR. Pamidronate treatment stimulates the onset of recover y phase reducing fracture rate and skeletal deformities in patients with idiopathic juvenile osteoporosis: comparison with untreated patients. J Bone Miner Metab. 2013; 31:533–43.53. Bachrach LK, Ward LM. Clinical review 1: bisphosphonate use in childhood osteoporosis. J Clin Endocrinol Metab. 2009; 94:400–9.54. Simm PJ, Biggin A, Zacharin MR, Rodda CP, Tham E, Siafarikas A, et al. Consensus guidelines on the use of bisphosphonate therapy in children and adolescents. J Paediatr Child Health. 2018; 54:223–33.55. Ozel S, Switzer L, Macintosh A, Fehlings D. Informing evidence-based clinical practice guidelines for children with cerebral palsy at risk of osteoporosis: an update. Dev Med Child Neurol. 2016; 58:918–23.56. Iwasaki T, Takei K, Nakamura S, Hosoda N, Yokota Y, Ishii M. Secondary osteoporosis in long-term bedridden patients with cerebral palsy. Pediatr Int. 2008; 50:269–75.57. Thornton J, Ashcroft DM, Mughal MZ, Elliott RA, O'Neill TW, Symmons D. Systematic review of effectiveness of bisphosphonates in treatment of low bone mineral density and fragility fractures in juvenile idiopathic arthritis. Arch Dis Child. 2006; 91:753–61.58. Acott PD, Wong JA, Lang BA, Crocker JF. Pamidronate treatment of pediatric fracture patients on chronic steroid therapy. Pediatr Nephrol. 2005; 20:368–73.59. El-Husseini AA, El-Agroudy AE, El-Sayed MF, Sobh MA, Ghoneim MA. Treatment of osteopenia and osteoporosis in renal transplant children and adolescents. Pediatr Transplant. 2004; 8:357–61.60. Sbrocchi AM, Forget S, Laforte D, Azouz EM, Rodd C. Zoledronic acid for the treatment of osteopenia in pediatric Crohn's disease. Pediatr Int. 2010; 52:754–61.61. Gordon KE, Dooley JM, Sheppard KM, MacSween J, Esser MJ. Impact of bisphosphonates on survival for patients with Duchenne muscular dystrophy. Pediatrics. 2011; 127:e353–8.62. Sbrocchi AM, Rauch F, Jacob P, McCormick A, McMillan HJ, Matzinger MA, et al. The u s e of i nt r ave nou s bisphosphonate therapy to treat vertebral fractures due to osteoporosis among boys with Duchenne muscular dystrophy. Osteoporos Int. 2012; 23:2703–11.63. Lee JM, Kim JE, Bae SH, Hah JO. Efficacy of pamidronate in children with low bone mineral density during and after chemotherapy for acute lymphoblastic leukemia and non-Hodgkin lymphoma. Blood Res. 2013; 48:99–106.64. Carpenter PA, Hoffmeister P, Chesnut CH 3rd, Storer B, Charuhas PM, Woolfrey AE, et al. Bisphosphonate therapy for reduced bone mineral density in children with chronic graft-versus-host disease. Biol Blood Marrow Transplant. 2007; 13:683–90.65. Suresh E, Pazianas M, Abrahamsen B. Safety issues with bisphosphonate therapy for osteoporosis. Rheumatology (Oxford). 2014; 53:19–31.66. Khosla S, Bilezikian JP, Dempster DW, Lewiecki EM, Miller PD, Neer RM, et al. Benefits and risks of bisphosphonate therapy for osteoporosis. J Clin Endocrinol Metab. 2012; 97:2272–82.67. Makitie O. Causes, mechanisms and management of paediatric osteoporosis. Nat Rev Rheumatol. 2013; 9:465–75.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- School-based nutrition interventions can improve bone health in children and adolescents
- Development and Implementation of Clinical Practice Guidelines: Current Status in Korea
- Obesity in Children and Adolescents: 2022 Update of Clinical Practice Guidelines for Obesity by the Korean Society for the Study of Obesity
- Metabolic syndrome in children and adolescents
- 2017 Clinical practice guidelines for dyslipidemia of Korean children and adolescents