Acute Crit Care.
2022 Feb;37(1):120-123. 10.4266/acc.2020.00983.
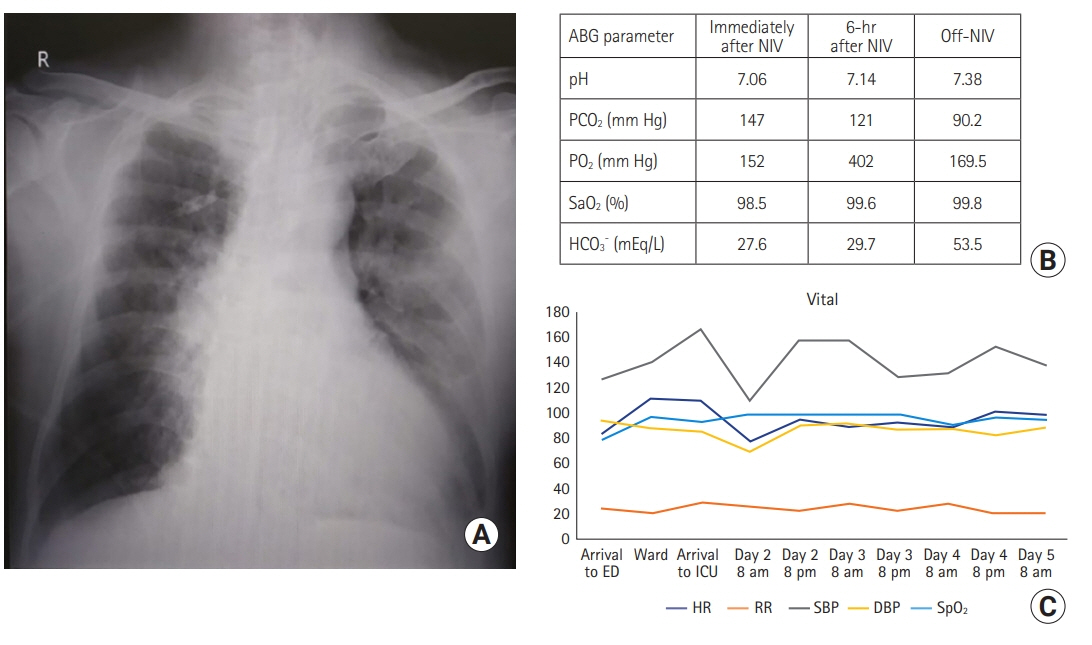
Successful noninvasive ventilation in a severely acidotic and hypercapnic comatose COVID-19 patient with multiple comorbidities: a case report
- Affiliations
-
- 1Department of Anesthesia, Pain and Critical Care, All India Institute of Medical Sciences, Raipur, India
- KMID: 2527915
- DOI: http://doi.org/10.4266/acc.2020.00983
Abstract
- Effective use of noninvasive ventilation in patients with chronic obstructive pulmonary disease is well-known. However, noninvasive ventilation in patients presenting with altered sensorium and severe acidosis (pH <7.1) has been rarely described. Invasive mechanical ventilation is associated with high mortality in coronavirus disease 2019 (COVID-19), and use of noninvasive ventilation over invasive ventilation is an area of investigation. We report a case of COVID-19-induced acute exacerbation of chronic obstructive pulmonary disease in a 66-year-old male. His past medical history included obstructive sleep apnea, hypertension, cor pulmonale, atrial fibrillation, and amiodarone-induced hypothyroidism. On presentation, he had acute hypercapnic respiratory failure, severe acidosis (partial pressure of carbon dioxide [PCO2], 147 mm Hg; pH, 7.06), and altered mentation. The patient was successfully managed with noninvasive ventilation, avoiding endotracheal intubation, invasive ventilation, and related complications. Although precarious, a trial of noninvasive ventilation can be considered in COVID-19-induced acute exacerbation of chronic obstructive pulmonary disease with hypercapnic respiratory failure, severe acidosis, and altered mentation.
Figure
Reference
-
1. Osadnik CR, Tee VS, Carson-Chahhoud KV, Picot J, Wedzicha JA, Smith BJ. Non-invasive ventilation for the management of acute hypercapnic respiratory failure due to exacerbation of chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2017; 7:CD004104.
Article2. Addala D, Shrimanker R, Davies MG. Non-invasive ventilation: initiation and initial management. Br J Hosp Med (Lond). 2017; 78:C140–4.
Article3. Kogo M, Nagata K, Ito J, Sato Y, Teraoka S, Kato R, et al. Noninvasive positive pressure ventilation for the treatment of acute hypoxic respiratory failure with altered consciousness level. Eur Respir J. 2016; 48(Suppl 60):PA3573.
Article4. Steriade AT, Johari S, Sargarovschi N, Necula D, Tudose CE, Ionita D, et al. Predictors of outcome of noninvasive ventilation in severe COPD exacerbation. BMC Pulm Med. 2019; 19:131.
Article5. Ozsancak Ugurlu A, Habesoglu MA. Epidemiology of NIV for acute respiratory failure in COPD patients: results from the international surveys vs. the "real world". COPD. 2017; 14:429–38.
Article6. Sweet DD, Naismith A, Keenan SP, Sinuff T, Dodek PM. Missed opportunities for noninvasive positive pressure ventilation: a utilization review. J Crit Care. 2008; 23:111–7.
Article7. Lee HW, Choi SM, Lee J, Park YS, Lee CH, Yoo CG, et al. Reduction of PaCO2 by high-flow nasal cannula in acute hypercapnic respiratory failure patients receiving conventional oxygen therapy. Acute Crit Care. 2019; 34:202–11.
Article8. Meduri GU, Conoscenti CC, Menashe P, Nair S. Noninvasive face mask ventilation in patients with acute respiratory failure. Chest. 1989; 95:865–70.
Article9. Schreiber A, Fusar Poli B, Bos LD, Nenna R. Noninvasive ventilation in hypercapnic respiratory failure: from rocking beds to fancy masks. Breathe (Sheff). 2018; 14:235–7.
Article10. Meduri GU, Abou-Shala N, Fox RC, Jones CB, Leeper KV, Wunderink RG. Noninvasive face mask mechanical ventilation in patients with acute hypercapnic respiratory failure. Chest. 1991; 100:445–54.
Article11. Alqahtani JS, Oyelade T, Aldhahir AM, Alghamdi SM, Almehmadi M, Alqahtani AS, et al. Prevalence, severity and mortality associated with COPD and smoking in patients with COVID-19: a rapid systematic review and meta-analysis. PLoS One. 2020; 15:e0233147.
Article12. Simons SO, Hurst JR, Miravitlles M, Franssen FM, Janssen DJ, Papi A, et al. Caring for patients with COPD and COVID-19: a viewpoint to spark discussion. Thorax. 2020; 75:1035–9.
Article13. Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: 2019 report [Internet]. Global Initiative for Chronic Obstructive Lung. Disease; 2019 [cited 2021 Jan 14]. Available from: https://goldcopd.org/wp-content/uploads/2018/11/GOLD-2019-v1.7-FINAL-14Nov2018-WMS.pdf.14. Gonçalves G, Saeed H, Abdelrahim ME, Harb HS, Madney YM, Eng K, et al. Non-invasive ventilation in patients with an altered level of consciousness: a clinical review and practical insights. Adv Respir Med. 2020; 88:233–44.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Acute Neuromuscular Respiratory Failure
- Mechanical Ventilation of the Children
- Noninvasive Positive Pressure Ventilation Using a Face Mask for a Child with Spinal Muscular Atrophy: A case report
- Multiple Abscesses Following COVID-19 Vaccination: A Case Report
- Comorbidities in the COVID-19 Pandemic: Scopus-Based Bibliometric Analysis